Medical Record Procedures at MGH Hospital
advertisement
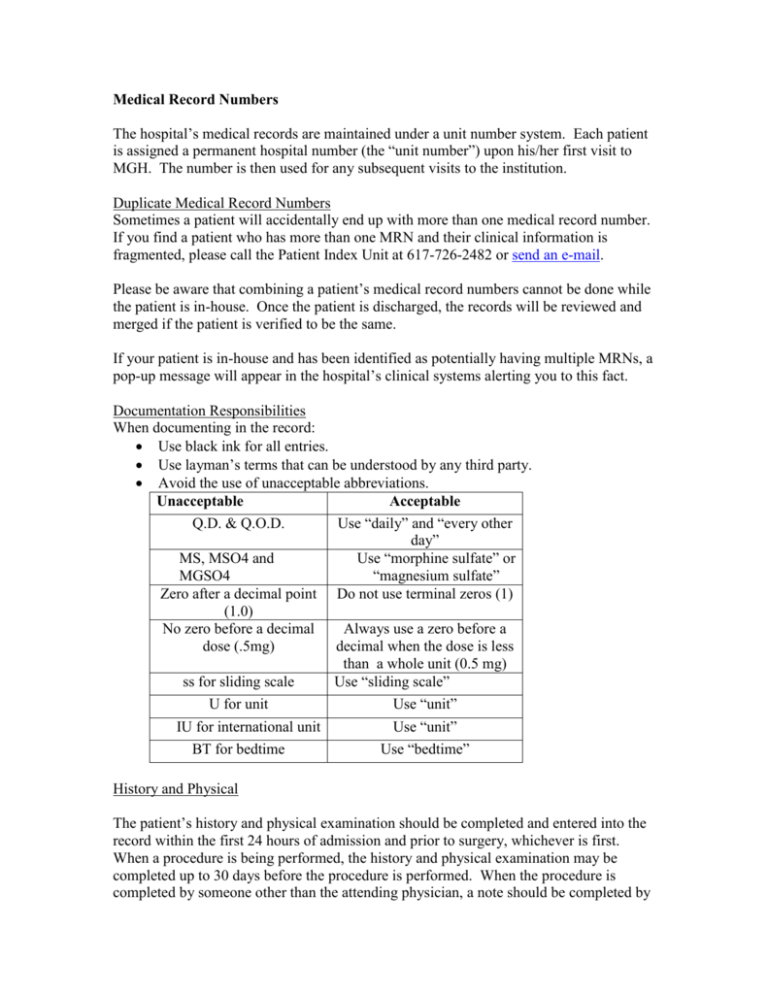
Medical Record Numbers The hospital’s medical records are maintained under a unit number system. Each patient is assigned a permanent hospital number (the “unit number”) upon his/her first visit to MGH. The number is then used for any subsequent visits to the institution. Duplicate Medical Record Numbers Sometimes a patient will accidentally end up with more than one medical record number. If you find a patient who has more than one MRN and their clinical information is fragmented, please call the Patient Index Unit at 617-726-2482 or send an e-mail. Please be aware that combining a patient’s medical record numbers cannot be done while the patient is in-house. Once the patient is discharged, the records will be reviewed and merged if the patient is verified to be the same. If your patient is in-house and has been identified as potentially having multiple MRNs, a pop-up message will appear in the hospital’s clinical systems alerting you to this fact. Documentation Responsibilities When documenting in the record: Use black ink for all entries. Use layman’s terms that can be understood by any third party. Avoid the use of unacceptable abbreviations. Unacceptable Acceptable Q.D. & Q.O.D. Use “daily” and “every other day” MS, MSO4 and Use “morphine sulfate” or MGSO4 “magnesium sulfate” Zero after a decimal point Do not use terminal zeros (1) (1.0) No zero before a decimal Always use a zero before a dose (.5mg) decimal when the dose is less than a whole unit (0.5 mg) ss for sliding scale Use “sliding scale” U for unit Use “unit” IU for international unit BT for bedtime Use “unit” Use “bedtime” History and Physical The patient’s history and physical examination should be completed and entered into the record within the first 24 hours of admission and prior to surgery, whichever is first. When a procedure is being performed, the history and physical examination may be completed up to 30 days before the procedure is performed. When the procedure is completed by someone other than the attending physician, a note should be completed by the other physician indicating his or her evaluation and agreement with the described plan. Progress Note Progress notes should be entered into the record within 24 hours of the visit, and finalized within 21 days after the visit. These notes document the necessity of the patient’s stay in an acute care institution. The attending physician or designee will enter dated, timed, and authenticated daily progress notes documenting the patient’s progress. Operative Report A complete and concise operative report should be dictated and finalized within 24 hours by the responsible physician after completion of surgery or any invasive procedure. Discharge Summaries A complete and concise discharge summary must be completed within 24 hours of the patient’s discharge. The responsible physician should complete the record at the time the patient is discharged. The medical record remains on the patient units for 24 hours after a patient’s discharge so that the record is available for completion. Principal (Discharge) Diagnosis A joint effort between the physician and HIS coder is essential to achieve complete and accurate documentation and prompt, appropriate hospital reimbursement. A vague principal (discharge) diagnoses that is unrelated to the reason for admission or does not accurately identify the reason for the patient’s admission will reduce reimbursement. The most common errors in Principal Dx are: Traumas: The principal diagnosis for traumas is listed as the cause of injury, a non-specific site of injury or simply trauma rather than the specific injury that is treated. MD Principal Dx Coder Principal Dx Lightening Strike 1st degree burn, back Polytrauma SDH Gun Shot Wound Injury, iliac vein Admitting Symptoms: Symptoms at the time of admission (in the ED) or those most representative of the condition are listed as the principal diagnosis even when a definitive condition is treated. MD Principal Dx Coder Principal Dx Chest Pain CAD or MI Abdominal Pain Cholecystitis/Choledochlithiasis Low Back Pain Lumbar Disk Hernia ion Hypoxia or AMS Aspiration PNA Surgery Performed Listed as Principal Diagnosis: The patient’s surgery is listed as the principal diagnosis instead of the diagnosis. MD Principal Dx Appendectomy Cholecystectomy THR Coder Principal Dx Acute Appendicitis Chronic Cholecystitis Osteoarthritis, hip Dictation Physicians can dictate inpatient operative notes and discharge summaries into a computerized dictation system from any MGH touch-tone telephone. Each physician is assigned his/her own six digit provider number with which to access the dictation system. General Guidelines for Dictation Identify yourself by your full name and Department. State if you are dictating for another physician, however you must still use your own individual six digit provider number Spell out the patient’s full name and state the patient’s medical record number. Indicate paragraphs and punctuation. For operative notes, give the date(s) of surgery, pre-and post-operative diagnoses/is and the name(s) of all procedures performed. For Discharge Summaries, give the admit and discharge dates. Upon completion, state the number of copies required and to whom they are to be sent. You must state and spell the full names and addresses of physicians who should receive copies. Cell phones should not be used for dictations Detailed guidelines for inpatient dictation are available in the HIS Transcription Department at 617-726-2488 and the web site https://hub.partners.org/wiki. Inpatient Dictation System Instructions 1. 2. 3. 4. 5. 6. Call 617-724-3125 and wait for the prompt. Enter you six digit provider number, then # on the keypad. To dictate press 1, to review a dictation press 3 Enter the 2-digit work type code (see below), then # on the keypad. Enter the 7-digit medical record number, then # on the keypad. To start to record, press 2 (you will hear a continuous tone that stops when you begin to dictate.). 7. To end the dictation, press 5, and hang up. Work types 11- Operative Reports 22- Discharge Summary 66- STAT transfer summary: (to be used only when a patient is being transferred to another healthcare facility) Incomplete Records Records not completed on the Patient Care Units or in the Same Day Surgical Unit are filed in the Incomplete Area within the Health Information Services Department on the 8th floor of the Founders Building 617-726-2490. A weekly listing of incomplete records is compiled and a notification e-mail is sent to each responsible physician. Delinquent Records When a record remains incomplete for 14 days or more, it is considered delinquent. If you have 3 or more delinquent records or any delinquent dictations you are eligible for suspension. Suspension allows the physician time to complete their delinquent records. The following privileges are not allowed during suspension: Admitting Privileges Operating Room Privileges Billing Privileges Any questions or problems about incomplete records should be immediately discussed with the Record Completion Department at 617-726-2490. Requesting Records Patient Care Immediate Record Requests for a patient’s MGH paper medical record for patient care purposes may be made by calling the Record Control Center at 617-726-2477 Research All records requested for research may be reviewed only in the Doctors’ Reading Room. Records may not be removed and must be reviewed within two weeks or they will be returned to the file. A maximum of 20 Record Request Slips are accepted at one time. These can be sent via telephone, email, or fax. Returning Records Inpatient Records Inpatient records should not be put in return boxes or sent through house mail. HIS picks up patient records that are left on the unit and delivers them to Record Processing for analysis, coding and completion. Outpatient Records Outpatient records should be returned to the Record Control Center by calling 617-7242477 to request that the records be picked up. Transferring Records As records are needed throughout the institution for a variety of reasons, it is imperative that HIS know the location of all records at any given time. Users are therefore requested to inform the department whenever they “lend” a record that is currently in their possession. Medical records can never leave the MGH campus. Release of Medical Records Medical record information is considered confidential and should not be discussed with anyone except the patient without appropriate written authorization. Outpatient Records Patient and third party requests for medical records, including photocopies, should be directed to the Release of Information Unit of the Health Information Services Department at 617-726-2361. Inpatient Records When a current inpatient requests to see a copy of his or her medical record, refer the patient to his or her attending physician. Faxing Information Patient information should not be faxed outside the institution. Refer all requests for faxed patient information to the Release of Information Department’s on-site fax number at 617-724-4559 or they can call 617-726-2361. Electronic Copies of Medical Records Occasionally a patient may request an electronic copy of their medical record information instead of a paper copy. These inquiries or requests should be directed to the on-site Release of Information Unit at 617-726-2469. Disability Forms/General Relief/Welfare Forms The Release of Information Unit is not responsible for completing insurance disability forms or General Relief/Welfare forms. These forms are to be completed by the physician. Requests for copies of medical records to accompany a disability/general relief/welfare form can be referred to the Release of Information Unit. If you have any questions about the release of medical records, call the Release of Information Unit at 617-726-2361 and refer to the medical record policies in the Clinical Policy and Procedure Manual.