Cellulitis is a spreading bacterial infection of the skin and tissues
advertisement

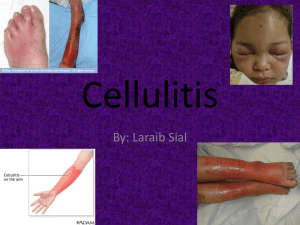
Cellulitis is a common infection of the lower layers of skin (dermis) and the subcutaneous tissues (areas underneath the skin) caused by a spreading bacterial infection of the skin and tissues beneath the skin. The main bacteria involved in cellulitis are Staphylococci are the bacteria that most commonly cause cellulitis, followed by Streptococci. Less commonly, other types of bacteria may cause cellulitis. What does cellulitis look like? Cellulitis usually begins as a small area of pain and redness and tenderness , swelling, and redness. As this red area begins to enlarge, the person may develop a fever—sometimes with chills and sweats— and swollen lymph nodes ("swollen glands") near the area of infected skin. The signs of cellulitis include redness, warmth, swelling, and pain in the involved tissues. Any skin wound or ulcer that exhibits these signs may be developing cellulitis. Cellulitis is a common infection of the lower layers of skin (dermis) and the subcutaneous tissues (areas underneath the skin) caused by a bacterial infection. While cellulitis sometimes develops around wounds in the skin or surgical incisions, in other cases it arises without an obvious source for the bacterial infection. Staphylococci are the bacteria that most commonly cause cellulitis, followed by Streptococci. Less commonly, other types of bacteria may cause cellulitis. What are the symptoms of cellulitis? Cellulitis usually begins as a small area of pain and redness on the skin. This area spreads to surrounding tissues, resulting in the typical signs of inflammation – redness, swelling, warmth, and pain. A person with cellulitis can also develop fever and/or swollen lymph nodes in the area of the infection. Who is at risk for cellulitis? Anyone may develop cellulitis. Males and females and people of all races are equally likely to become infected. However, people whose immune systems are weakened for any reason (including from chemotherapy for cancer or other immune-suppressing drugs) and those with diabetes are at highest risk for developing cellulitis. Antibiotics are essential for the treatment of cellulitis. Penicillin derivatives are often prescribed to treat cellulitis, but other antibiotics can also be effective. In more advanced cases of cellulitis, hospitalization and administration of intravenous antibiotics may be required. If not appropriately treated, the bacterial infection can spread throughout the body, resulting in serious illness. Definition Cellulitis refers to an infection of the skin that may spread to tissue just beneath the skin's surface. It may occur anywhere on the body, but most commonly affects the face or lower legs. Causes Cellulitis is usually caused by a bacterial infection. The infection may come from bacteria that normally lives on the skin or bacteria from other sources. The bacterial infection may be caused by: A minor injury to the skin, such as a cut, scratch, blister, puncture, or bite, that becomes infected and spreads into the surrounding skin Chickenpox blisters that open up and become infected with bacteria Injuries that occur in natural bodies of water that become infected with germs found in the water A cut or abrasion that becomes infected by food bacteria while handling fish, poultry, eggs, or meat Bacteria that enter the body through surgical wounds or a catheter in a vein Infection in a person with diabetes or a weakened immune system Bacteria spreading from an upper respiratory or ear infection Impaired circulation (tends to cause recurrence of cellulitis) Puncture Wound Risk Factors A risk factor is something that increases your chance of getting a disease or condition. Risk factors include: Insect, animal, or human bites Diabetes Weakened immune system, such as AIDS Alcoholism Chronic use of steroids Kidney and liver failure Surgical procedures Poor circulation or peripheral vascular disease Swelling or fluid retention Intravenous drug abuse Burns Exposure to fish, meat, hides, shellfish, poultry, or eggs Symptoms Symptoms may begin within hours or days and can include: Skin inflammation that begins in a small area and spreads. This includes: o Redness o Pain or tenderness o Swelling o Warmth o A red streak (possibly) Swollen lymph nodes Fever or chills Fatigue Headache Cellulitis near the eyes may cause pain with eye movements and should be treated urgently Diagnosis The doctor will ask about your symptoms and medical history, and perform a physical exam. Expect to answer questions about how the wound occurred and exposure to animals or natural bodies of water. Your skin will be closely examined. Using a colored pen on your skin, the doctor can mark the border of the cellulitis to monitor its progress. Tests may include: Wound culture—a sterile applicator swabbed across the area and sent to a lab to be tested for bacteria and type of antibiotics to use in treating the infection. (This test is rarely, if ever, performed anymore since the bacteria on the swab will reflect the bacteria that colonize our skin normally and, hence, the test is not useful.) Blood tests—to help determine the severity of the infection X-rays, bone scans, or CAT scans—to check for gangrene under the skin or evidence that the infection has spread to the bone Treatment The treatment goal is to eliminate the infection and reduce discomfort. Most cases of cellulitis resolve after a week or two of treatment. An infected wound can be cleaned and any dead tissue removed. If a collection of pus (called an abscess) is present, it can be drained. Severe cellulitis, cellulitis in a diabetic or immune suppressed person, or an infection on the face may require hospital care. Treatment includes: Medication Antibiotics may be taken by mouth or injected into a muscle or vein, depending on the severity of the infection. Take the entire prescription as directed until all the medicine prescribed is used. Otherwise, the infection may return. Supportive Care This may include resting in bed or elevating the infected area higher than your heart. The doctor might recommend applying warm or cool compresses to the area. Change your dressings as directed by your doctor, and protect your skin from additional injury. Do not scratch or rub the area. Facial cellulitis is a bacterial skin infection that occurs on the face. The infection is characterized by swelling, redness, warmth, and pain. Risk factors for the condition include problems in the lymphatic system, upper respiratory infections, and infections of the teeth or middle ear. In addition to the appearance of the skin in the affected area, symptoms of facial cellulitis may include fever, chills, irritability, and a swollen, tender, warm tongue. Treatment for facial cellulitis involves antibiotics and recurrence prevention. The most common cellulitis cause in adults with no medical conditions is group A streptococcus, which is a bacterium commonly found in the throat and on the skin. Another common cause in adults is Staphylococcus aureus (S. aureus), which is a bacterium that is commonly found on human skin and mucosa (lining of mouth and nose). Other Cellulitis Causes In rare cases, other bacteria can cause cellulitis. When this does occur, it is usually the result of a medical condition such as diabetes, HIV, or AIDS, or because the cellulitis is in a very specific place. Other bacteria that can lead to cellulitis include: Methicillin-resistant S. aureus (MRSA) P. aeruginosa Vibrio vulnificus Clostridium septicum Pasteurella multocida Erysipelothrix E. coli Group B streptococcus. Know the Risk Factors Cellulitis research has shown that people with certain risk factors are more likely to develop the infection. Generally, cellulitis risk factors include: Problems with the lymphatic system Vein problems Swelling of the leg Breaks in the skin Obesity. Specific cellulitis risk factors include: Surgical wounds Skin ulcer (such as a diabetic foot ulcer) Athlete's foot Eczema, psoriasis, or other skin conditions that may cause a break in the skin A previous episode of cellulitis Surgery with lymph node removal Radiation therapy Coronary artery bypass surgery IV drug use Chemotherapy Pregnancy Certain conditions (such as diabetes, HIV or AIDS, leukemia, lymphoma, psoriasis, dyshidrosis, lupus, and heart failure). Risk factors for cellulitis are not causes of the condition; however, such risk factors do increase a person's chance of developing the infection. People who think that they may be at risk of developing cellulitis should discuss this concern with their doctor. Symptoms of Facial Cellulitis Facial cellulitis symptoms occur at the location of the infected skin (local cellulitis symptoms) or on other parts of the body (systemic cellulitis symptoms). Common local and systemic symptoms of facial cellulitis include: Fever Irritability Swelling and redness of the cheek Itching and burning of the cheek Swollen, tender, warm tongue. Other symptoms of facial cellulitis may include: Chills Body aches Vomiting Decreased appetite. Diagnosing Facial Cellulitis Your doctor can make a facial cellulitis diagnosis by asking a number of questions, reviewing your medical history, performing a physical exam, and ordering certain blood tests. The most reliable way of diagnosing facial cellulitis is by examining the affected area. An area affected by cellulitis will be: Red Warm to the touch Swollen Painful. Your doctor will also look for breaks in your skin (such as cuts, bruises, scrapes, eczema, or other skin conditions) where bacteria could have entered. A blood test can determine if there is any indication of an infection. Treatment of Facial Cellulitis The goal of facial cellulitis treatment is to treat the affected area and any underlying conditions that would cause a reoccurrence. Specific treatment for facial cellulitis includes antibiotics and recurrence prevention. Facial cellulitis treatment will begin with antibiotics. Depending on the severity of facial cellulitis, antibiotics are given either in the hospital, at home, or in a combination of these two locations. Be sure to tell your doctor if you are allergic to penicillin. Up to 30 percent of people who receive treatment for facial cellulitis will experience a recurrence of the infection. Therefore, doctors may prescribe antibiotics for longer periods of time for patients who continue to get facial cellulitis.