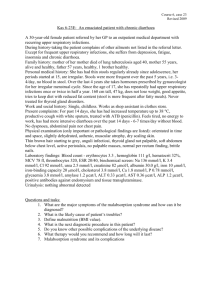
Case 1: Gastrointestinal bleeding
advertisement

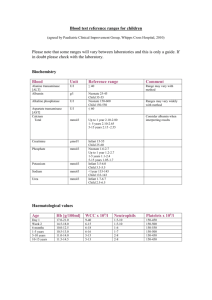
Case 1: Gastrointestinal bleeding 40 year old man, manager, consults his doctor because in the last two weeks he has alternately completely black stools. Although otherwise he feels well, he is aware that about two years he feels an unpleasant sensation in the epigastrium. Initially, this sense appeared in the late afternoon, but recently also in the middle of the night waking him from sleep. He suppresses pain by either eating or tablets containing bicarbonate (baking soda). He does not take other medicines. Last week, he noticed that he has "shortened breath" when he went upstairs. In his job, the patient is in a constant stress, sometimes he drinks alcoholic beverages and is a heavy smoker. Physical examination: the patient is markedly pale, the color is most obvious in the conjunctiva and on the nails. Apart from a slightly elevated heart rate (100/min) and a sense of tension in the epigastrium, he is without a physical examination findings. Stool obtained at digital rectal examination, is dark and is positive for blood. 1. The patient's hematocrit was 21%, hemoglobin 60g/l, red blood cells 4x106/l. how would you evaluate these results? 2. How may be associated pallor, dyspnea, and slightly elevated heart rate? 3. How will change the blood count after sudden loss of blood - eg haematemesis? 4. How would you prove that the patient is bleeding chronically? 5. Black stool is a sign of bleeding from upper GIT. Why? How could you recognize bleeding from the lower parts of GIT? What may be the cause of such bleeding? 6. What the patient is most likely suffering from? 7. What is the most likely cause of bleeding in this patient? Case 2: Bleeding -Injury 31-year-old man was brought to the Emergency by a helicopter after a five feet fall on sharp rocks. The man was alert and oriented when his friends reached him, and could move all four extremities quite easily. He had multiple scrapes over his anterior torso and a large gash over his right anterior upper thigh (near the groin) which was bleeding profusely. A makeshift tourniquet slowed the bleeding. The patient became increasingly disoriented during the flight, reaching the emergency room about 40 minutes after the fall. Physical Examination: The patient was lethargic but responsive to shouting and sternal pinch. He had multiple abrasions over his chin, neck, anterior thorax, and abdomen. A six- 1 inch-long, half-inch deep laceration was noted in the right inguinal region, extending into the right, upper thigh. The tourniquet placed in this area was soaked with blood. Vital signs were as follows: HR = 112 (supine) and 128 (sitting), BP = 108 / 60 (supine) and 92 / 52 (sitting), RR = 32. Skin was cold and clammy, and nail beds, palms, and mucous membranes were pale. Laboratory findings: Haemoglobin Hematocrit White blood cells Sodium Potassium Chloride Creatinine Urea SGPT SGOT Glucose Blood pH pCO2 HCO3pO2 Hodnoty 150 g/l 46% 7 400 138 mmol/ 5,1 mmol/l 104mmol/l Norma 115-155g/l 36-45% 4300 -10,000/mm3 136-145 mmol/l 3.7-5.2 mmol/l 96-106 mmol/l 150 umol/l 15 mmol/l 40 -120 μmol/l 2,8 -8 mmol/l 41 IU/l 48 IU/l 0-33IU/l 0-41 IU/l 7,5 mmol/l 3,5, - 5,5 mmol/l 7,28 31 mm Hg 14 mmol/ 78 mm Hg 7,36 – 7,46 40 mm Hg 22-26 mmol/l 90 – 100 mm Hg Urinary output in the first 60 minutes in ER was 20 ml (color was dark yellow). Urine specific gravity was 1.029 (normal = 1.003 - 1.030). Central venous pressure ranged from 1 to 3 cm H2O throughout the cardiac cycle (normal = range = 5.5 to 13 cm H2O). ECG revealed normal sinus rhythm with slight ST-depression in most leads. 1. What is the patient's main problem now? 2. Is the patient's urine output in the standard? Why is it important to monitor the urine volume and quality? 3. Why has the patient increased urea and creatinine? 4. How would change the patient’s hematocrit within 24 hours if the patient was stabilized? Why? 2 Case 3: Bleeding - Shock Two teenagers, Adam and Ben, are involved in an automobile accident , and both suffer significant blood loss. They are taken to the nearest trauma centre. Adam has mean arterial pressure of 55 mmHg, a pulse pressure of 20 mmHg and a heart rate of 120 beats per minute. He is anxious, but alert, has a slightly decreased urine output and has cool pale skin. Ben has a mean arterial pressure of 40 mmHg, a barely measurable pulse pressure and a heart rate of 160 beats per minute. He is comatose, has no urine output and is has cold skin. Adam is treated by stopping the bleeding and administering Ringer’s lactate solution intravenously and a blood transfusion. The physicians are prepared to administer a positive inotropic agent but find it unnecessary since Adam shows signs of improvement. During the next five hours Adam’s mean arterial pressure increases back to normal and his heart rate simultaneously decreases to a normal value of 75 beats per minute. His skin gradually warms and the normal pink color returns. Ben is treated in the same way as Adam, but despite the physician’s efforts, he dies. 1. Is it possible to estimate the amount of lost blood from the findings? 2. Why have Adam and Ben decreased blood pressure and increased heart rate? Describe the changes in the body. 3. Why is their skin pale and cold? Which other sign could you see on it? 4. Why the quality of pulse (or the pulse pressure) is important? 5. What are the first signs of decreased brain perfusion? When the unconsciousness occurs? 6. What is the cause of oliguria or anuria? Why is the finding important? How could you distinguish the prerenal azotemia and renal failure? 7. Why are Adam and Ben treated with Ringer solution at first? 8. Why were the physicians prepared to administer a positive inotropic agent? 9. Why could not Ben be rescued? 3 Case 4: MOF Mr. Roberts, age 63, arrived in the ED unconscious with stab wounds to the right upper abdomen after fighting off a bugler in his home. After 2000 ml of fluid was infused, Mr. Roberts was taken to surgery, where a right thoracotomy and right upper abdomen laparotomy were performed. Liver And duodenal lacerations were repaired. The abdominal cavity was irrigated with antibiotic solution and 3 drains were placed. Mr. Roberts received 6 units of PRBC and 3 litres of LR. Following assessment data are gathered: BP 92/52; HR 114; RR12; Temp. 36.2°C pH 7,34; PaCO2 36 torr; PaO2 84 torr; HCO3- 21 mmol/l Hgb 10; HCT 31; WBC 13,6 1. Which types of shock may Mr.Roberts develop? Why? Mr.Roberts remained stable until post-op day 2. He received IV. fluids at 125 ml/hod, nasogastric drainage averaged 200 ml/8 hours, urine output averaged 40-50 ml/hr. At 22.oo on post –op day 2, Mr.Roberts became agitated, and following assessment data were obtained: BP 90/60; HR 126; RR12; Temp. 38.6°C pH 7,30; PaCO2 46 torr; PaO2 65 torr; HCO3- 25 mmol/l Hgb 9; HCT 27; WBC 4,2 2. What do you thing is happening? What additional assessments do you want to support your conclusion? What do you expect to be done now? By the next morning, Mr. Roberts was receiving fluids at 175 ml/hr and vasopressor therapy has been started. Several fluid boluses of 250ml NS have given. Urine output is less than 30ml/hr. The following assessment data has been obtained: BP 80/50; HR 132; RR28; Temp. 40,1°C Glu 270 g/100 ml (N = 80-120g/100ml) WBC 22 3. Why has the patient hyperglycemia? By the sixth post-op day, Mr. Roberts condition continues to deteriorate. His skin is cool, mottled and moist. Scleras are yellow-tinged. He is no longer responsive to stimuli. The cardiac monitor displays sinus tachycardia with episodes of ventricular tachycardia; ST elevation in leads V2 – V5 ; T wave inversion in all leads and Q waves present in leads V1 – V4. Urinary output is 3-5 ml/hr. Abdomen is grossly distended and bowel sounds are absent. The following data has been obtained: BP 72/46; HR 140; RR14; Temp. 38.6°C pH 7,14; PaCO2 49 torr; PaO2 46 torr Na+ 152 mmol/l; K+ 5,9; Creat 3,4; BUN 104;amylase in urine 290 Hgb 9; HCT 27; WBC 4,2 Temp. 35.5°C 4. Which organs are dysfunctional? 4