i. secondary iol implantation
advertisement
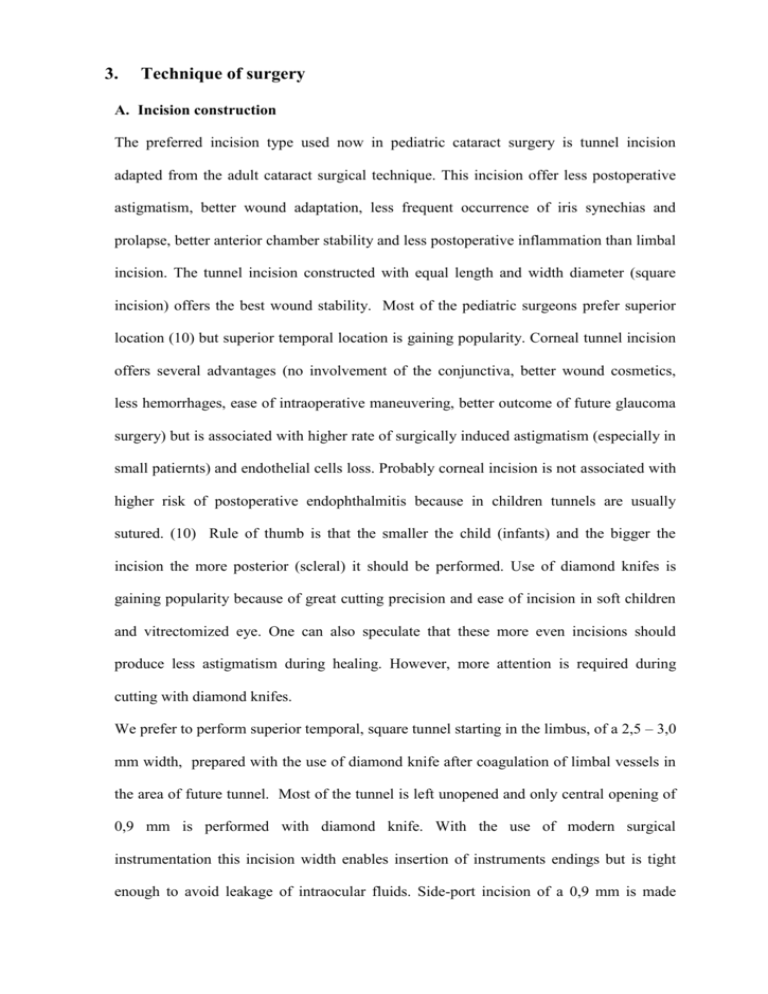
3. Technique of surgery A. Incision construction The preferred incision type used now in pediatric cataract surgery is tunnel incision adapted from the adult cataract surgical technique. This incision offer less postoperative astigmatism, better wound adaptation, less frequent occurrence of iris synechias and prolapse, better anterior chamber stability and less postoperative inflammation than limbal incision. The tunnel incision constructed with equal length and width diameter (square incision) offers the best wound stability. Most of the pediatric surgeons prefer superior location (10) but superior temporal location is gaining popularity. Corneal tunnel incision offers several advantages (no involvement of the conjunctiva, better wound cosmetics, less hemorrhages, ease of intraoperative maneuvering, better outcome of future glaucoma surgery) but is associated with higher rate of surgically induced astigmatism (especially in small patiernts) and endothelial cells loss. Probably corneal incision is not associated with higher risk of postoperative endophthalmitis because in children tunnels are usually sutured. (10) Rule of thumb is that the smaller the child (infants) and the bigger the incision the more posterior (scleral) it should be performed. Use of diamond knifes is gaining popularity because of great cutting precision and ease of incision in soft children and vitrectomized eye. One can also speculate that these more even incisions should produce less astigmatism during healing. However, more attention is required during cutting with diamond knifes. We prefer to perform superior temporal, square tunnel starting in the limbus, of a 2,5 – 3,0 mm width, prepared with the use of diamond knife after coagulation of limbal vessels in the area of future tunnel. Most of the tunnel is left unopened and only central opening of 0,9 mm is performed with diamond knife. With the use of modern surgical instrumentation this incision width enables insertion of instruments endings but is tight enough to avoid leakage of intraocular fluids. Side-port incision of a 0,9 mm is made about 90º to the left of the tunnel in front of limbal vascular arcade with the use of diamond knife. B. Anterior capsule surgery Surgery of the anterior capsule is one of most difficult stages of cataract surgery in children because of extreme elasticity of the capsule, necessity to use more force to tear the capsule, ease of extension of tearing out toward the lens equator, high vitreous pressure, ease of anterior chamber collapse and frequent poor pupil dilatation. The preparations for anterior capsule surgery include pupil dilatation with 1:10000 intracameral adrenaline injection (if there are no systemic contraindications) and filling the anterior chamber with viscoelastic agents. Authors preference is high-viscosity cohesive viscoelastics because of better space creation by these agents (which is important in shallow, easily collapsing during surgical manipulations anterior chamber of small children), better maintenance of pupil dilatation and anterior capsule flattening (easier, more controlled capsulorhexis). The most popular techniques of anterior capsule surgery nowadays include manual continuous curvilinear capsulorhexis (the most difficult to perform), vitrectorhexis (performed with the use of a vitrector supported by a Venturi pump) and radiofrequency diathermy capsulotomy. Less popular of techniques include can-opener technique, Fugo plasma blade capsulotomy and two-incision push-pull technique (36, 40, 42). Comparative studies have shown that manual continuous curvilinear capsulorhexis produce more stronge, smooth, tear resistant, elastic capsular edge than bipolar radiofrequency capsulotomy and vitrectorhexis although results the last method were nearly comparable with the first one (37-40, 42). Therefore, although the most difficult, manual continuous curvilinear capsulorhexis remains gold standard of anterior capsular surgery in pediatric cataract. (Fig. 14) Indocyanine green staining of the anterior capsule may facilitate performance of manual continuous curvilinear capsulorhexis in children (40). Authors preferred technique of anterior capsular surgery is manual continuous curvilinear capsulorhexis performed after filling anterior chamber with high-viscosity cohesive viscoelastic agent, with “frequent grasp/regrasp technique”, tearing force directed toward the center of the pupil and capsulorhexis size of no more than 4,0 mm (size of opening will enlarge during next step of operation because of capsule elasticity). Fig. 14 Anterior capsule 2 years after manual capsulorhexis in 2,5-years-old child. C. Multiquadrant, cortical-cleaving hydrodissection Because of softness of children’s lens nucleus and cortex hydrodissection is not so important step in pediatric cataract surgery than it is in adults. However, this technique facilitates lens substance removal, decrease its time and lessens volume of used fluid. (41) D. Aspiration of lens substance The aim of aspiration is to remove thoroughly lens substance to clear visual axis and to prevent future proliferation of mitotically active lens epithelial cells and visual axis opacification. Because children’s lens nucleus and cortex are soft any method of phacoemulsification or phacofragmentation are used and only simple irrigation and aspiration of lens substance is performed. Two methods of irrigation and aspiration are used: single-port and bimanual. Both methods can be manual and automated. Bimanual approach is preferably used in pediatric cases because of more thorough removal of lens substance (especially in subincisional space), better maintenance of anterior chamber and less fluctuations of fluids in the anterior chamber. Standard irrigation/aspiration hand pieces are used but lens material can be also aspirated using vitrector with irrigation/aspiration working mode which shortens time of surgery and diminish anterior chamber manipulations associated with repeated entries into the eye during changing of hand pieces before posterior capsulectomy and anterior vitrectomy. Use of automated irrigation/aspiration helps in maintaining of the anterior chamber because of better balancing of aspiration and infusion. E. Posterior capsule surgery and anterior vitrectomy It is well known that posterior capsule opacification is very rapid in children. The younger the child the more pronounced is opacification. It is caused by proliferation and migration of residual lens epithelial cells and their transformation to myofibroblasts. (40) In children vitreous is the dense structure and anterior vitreous face is in closed contact with posterior capsule. Therefore it can act as a scaffold not only for lens epithelial cells, but also for metaplastic pigment epithelial cells, exudates. (42) Visual axis opacification (VAO) is the most common complication and one of the most important in pediatric cataract surgery because it induces amblyopia and it stops development of binocular vision if it occurs during the critical period of visual development in children. Therefore most surgeons routinely perform posterior capsulotomy in children younger then 8-10 years. (40, 42) However, primary posterior capsulotomy is not enough to prevent VAO if it is performed without anterior vitrectomy (40, 42, 43). Also posterior optic capture without anterior vitrectomy do not ensure clear visual axis. (35) Therefore primary posterior capsulotomy and anterior vitrectomy is regarded nowadays as standard surgical procedure of pediatric cataract surgery in children younger than 8-10 years. (40, 42, 43, 44) Various options have been proposed how to perform posterior capsulotomy and anterior vitrectomy. As with anterior capsulorhexis posterior capsulotomy can be made with manual technique, vitrector or with radiofrequency diathermy. The last method is nowadays the least popular because capsular margin after this procedure is the least tear resistant. Posterior capsule is much thinner than anterior one (4-9μm) and performance of manual capsulorhexis or vitrectorhexis is more complicated than anterior capsulorhexis although achieved opening margin is smooth and strong. Many surgeons prefer to perform posterior capsulotomy with vitrector if anterior vitrectomy is simultaneously planned. Capsule opening margin after this procedure is strong enough to maintain position of IOL in the capsular bag and both procedures are made with one instrument what shortens time of surgery. Diameter of posterior capsulotomy should be 4,0 to 4,5 mm and anterior vitrectomy should be 3 mm deep to prevent capsule opacification. (40, 45) (Fig. 15, 16) Only central anterior vitreous should be removed. There are still controversies whether they should be performed or after IOL implantation. It is easier to perform the procedures first but then it is more difficult to implant IOL in the bag in a soft vitrectomized eye. IOL is more easily implanted into the bag with the intact posterior capsule and IOL is already in place before posterior capsule management but then is more difficult to remove capsule and anterior vitreous. Performance of manual posterior capsulorhexis with IOL in the bag may be troublesome because tilted IOL can produce uneven tensions of different parts of posterior capsule. The more common practice now is to do posterior capsulotomy and anterior vitrectomy before IOL implantation. (42) Posterior capsulotomy and anterior vitrectomy can also be performed through pars plana, usually after IOL implantation. (42, 46) With this approach one can obtain larger capsule opening because IOL is already in place and no vitreous strand will be attached to wound but this procedure extends the time and scope of operation (most pediatric cataract surgeon are not routinely familiar with pars plana approach), requires additional incision of sclera and pars plana and scleral and conjunctival suturing. Therefore this technique is now not commonly used. Primary posterior capsulotomy with optic capture was described by Gimbel and DeBroff. (47) However, if optic capture if performed without anterior vitrectomy it do not ensure clear visual axis. (45) Optic capture is rarely used because it is technically challenging, associated with higher rate of IOL subluxation and future IOL exchange is more difficult. (40) Nd-YAG laser capsulotomy is nowadays rarely used as a primary procedure because of high reopacification rate (scaffold of the anterior vitreous face is not removed). The author’s preferred approach is to perform both limbal posterior capsulotomy of 4,0 to 4,5 mm diameter and anterior vitrectomy with vitrector and side-port separate irrigation before IOL implantation. F. IOL implantation Preferable method is implantation with the use of injectors because of more aseptic condition of this maneuver and smaller incision. During implantation it is very important to place lower haptic in the capsular bag which sometimes may be difficult in children’s soft, vitrectomized eye because of movements of lower haptic during unfolding. It is advisable to wait until lower haptic unfold completely in the center of anterior chamber and guide it into the bag with the spatula or hook inserted through the side-port. G. Bimanual aspiration/irrigation of viscoelastic agent Postoperative IOP elevation is infrequent after cataract surgery in children because of good outflow facility. However, it is advisable to remove viscoelastics from the anterior chamber at the end of operation. H. Wound suturing Tunnel incision in children usually is not self sealing because of high elasticity of pediatric cornea and sclera. More poor wound healing can be also attributed to frequent eye rubbing in children, more frequent eye trauma, using of higher doses of steroids and more vivid behavior of children after the surgery. Performance of detailed slit lamp examination of the wound to diagnose leakage is often difficult or even impossible in small children. Clinical observations of Basti and coworkers have shown that unsutured wounds are usually not watertight in children after cataract surgery especially when anterior vitrectomy was performed. (48). Therefore it is advisable to suture tunnel incision after pediatric cataract surgery. (49) In USA only 2,8% of pediatric ophthalmologists performing cataract surgery left incision unsutured. (6) Usually wound 2,5 – 3,0 mm is closed with one single 10/0 nylon suture although 10/0 Vicryl adsorbable sutures are also used. (49) It is important that needle entries should be equidistant from wound edges, placed at the same depth of cornea or sclera, placed perpendicular to wound and knots should be hidden inside wound. Suture tension should be corrected with Maloney keratometer with the eye filled with Ringer solution injected through the side-port. These precautions should diminish development of postoperative astigmatism in children. Fig. 15 Implanted IOL three years after surgery in 5-year-old child. Note anterior and posterior capsulorhexis and opacification of the anterior capsule. TABLE IV Technique of pediatric cataract surgery (authors preference) 1. Coagulation of limbal vessels in the area of future limbus tunnel 2. Preparation of unopened limbus, superior temporal, square tunnel of a 2,5 – 3,0 mm width with the use of diamond knife 3. 0,9 mm anterior chamber opening in the center of tunnel incision 4. 0,9 mm sideport incision (diamond knife) 5. Pupil dilation with the use of intracameral injection of 1:10 000 adrenaline solution 6. Filling anterior chamber with high viscosity viscoelastic agent 7. Manual continuous curvilinear capsulorhexis (“frequent grasp/ regrasp technique”, tearing force directed toward the center of the pupil, capsulorhexis size no more than 4 mm) 8. Multiquadrant, cortical-cleaving hydrodissection 9. Automated bimanual irrigation and aspiration of lens substance 10. Limbal posterior capsulotomy (4,0 to 5,0 mm diameter) and anterior vitrectomy with the use of vitrector and separate side-port irrigation 11. Enlargement of tunnel incision to 2,5 – 3,0 mm incision (according to the type of IOL and injector) with diamond knife 12. Loading of foldable IOL to the injector 13. Injector implantation of IOL 14. Bimanual aspiration/irrigation of viscoelastic agent 15. Tunnel suturing with single 10/0 nylon 16. Suture tension adjustment with the use of Maloney keratometer 4-5 mm 4 mm Fig, 16 Schematic presentation of the technique of pediatric cataract surgery with IOL implantation I. SECONDARY IOL IMPLANTATION 1. Timing of surgery There are two main indications for secondary IOL implantation in a child after cataract surgery without IOL implantation: noncompliance to other forms of aphakic correction and IOL implantation as final aphakia correction. In first situation secondary implantation can be performed at any age even in a child younger than 1 year. Main indication for the surgery is achievement of the best conditions for the development of binocular vision. So, the decision of the age of surgery must be individually considered according to a situation. Up to now there are no recommendations concerning the age of IOL implantation for final aphakic correction. From one side implantation should be performed as late as possible because axial growth is increasing until age of 14 years. (Fig. 8) This ensures the smallest residual refraction for the rest of the adult life. From the other side contact lenses or thick aphakic eyeglasses are very inconvenient for the child and create both cosmetic (eyeglasses) and maintenance problems (contact lenses). A lot of parents are asking for IOL implantation because they afraid that with going to school for the most of the day they will loose control over the child and changing of the life environment from home to school will create new problems for the aphakic child. Primary school starts at different age in various countries, usually between 5 and 7 years of life. In Poland children go to school at age of 6 years but the first year is so called preschool education. The changes of IOL power necessary for aphakia correction are small after 7-8 years of life (Fig. 12). Therefore the author’s recommendation is to perform secondary implantation before starting regular school activity i.e. at age of 7 years. 2. Technique of implantation Generally the technique of secondary IOL implantation is similar to primary IOL implantation. The main difference is that we are not removing opacified lens but we have to create the support for IOL using different anatomical structures inside the eye. The methods of IOL fixation includes: in-the bag fixation, ciliary sulcus fixation, optic capture, scleral fixation, iris fixation and anterior chamber fixation. A. In-the bag-fixation In-the-bag implantation creates the best position for IOL because it sequestrates acrylic IOL material from the highly reactive uveal tissues and ensures its best centration. (50) Bag reopening is possible if previous lensectomy was properly performed leaving peripheral parts of both anterior and posterior capsules in place. If lensectomy is performed early (in infants) intensive proliferation of lens epithelial cells creates cortical masses separating peripheral parts of the anterior and posterior capsules. They can not to be absorbed because they are trapped in the bag by the fusion of the incised edges of the anterior and posterior capsules. It forms the space for the future secondary implantation. In older children lens epithelial cells proliferation is much less intensive and both capsules fuse together far to the periphery. Reopening of the bag is of course not always possible. Sometimes dissected posterior capsule is not strong enough to support IOL. Wilson reported the technique of bag opening with the use of vitrectomy probe. (51) In these operation fused capsular edges are cut with vitrector, separated, capsular bag is cleaned of cortical masses with aspiration and irrigation, capsular bag is opened with viscoelastic and IOL implantation is performed. B. Ciliary sulcus fixation If capsules are inseparable and in-the-bag implantation is not possible ciliary sulcus fixation is chosen. (Fig. 17) There are some reports that sulcus fixation is quite safe and effective in children (52, 53, 54). Avad studied position of secondary sulcus implanted IOLs in children and did not observed haptic erosion into the sclera, ciliary body or sulcus. (53) However, pigment dispersion syndrome may sometimes develop in long-term in some children because of the direct contact of IOL material with pigmented layer of the iris. If IOL diameter is not properly chosen IOL may move or tilt inside the eye and papillary capture may develop. Fig, 17 Schematic presentation of the technique of secondary IOL implantation with sulcus fixation. C. Optic capture Optic capture of the ciliary sulcus implanted IOL behind the fused anterior and posterior capsules is sometimes used to achieve better centration of an IOL. (50) (Fig. 18) However, children with optic capture are more prone to synechia formation and development cellular deposits on an IOL optic. (55) Fig, 18 Schematic presentation of the technique of secondary IOL implantation with sulcus fixation and optic capture. D. Scleral fixation Scleral suture IOL fixation is used if capsular support is absent. Several techniques of this procedure both ab externo and ab interno have been described. (56) Their detailed description is outside of scope of this chapter. The aim of the operation is to suture IOL to the sclera in the ciliary sulcus with the use of 10/0 polypropylene suture with long (16 mm) straight needle. (Fig. 19) Two partial-thickness scleral flaps are prepared at 2 (or 4) and 8 (or 10) o’clock positions. They are used afterwards to cover the prolene suture knots and to prevent endophthalmitis and conjunctiva erosion over the knot. It is advisable to avoid 3 and 9 o’clock position because of the presence of long ciliary arteries and nerves. Scleral flaps are prepared after incision of the conjunctiva or limbal incision is made and sclera is dissected backwards without dissecting the conjunctiva. (57) The straight needle of 10/0 polypropylene suture is then passed through the sclera under one of the scleral flaps (0,75 mm posterior to the limbus), entering the posterior chamber and going out of the eye under the flap on the other side of cornea. The suture is taken out of the posterior chamber cut and one end is tied to IOL haptic pushed out of the injector nozzle. IOL is injected to the posterior chamber with the second haptic left in the wound. Second end of polypropylene suture is then tied to this haptic and IOL is placed in posterior chamber. The author preference is to use foldable, hydrophilic IOLs with complex haptic (Super-flex, Rayner) because of better uveal biocompatibility of acrylic hydrophilic material and closed, deformation-resistant haptic system. It is very important to adequately fixate polypropylene suture to the sclera under the flap with 1 or 2 large bites and carefully close covering flaps with 10/0 nylon sutures. IOL scleral fixation technique is usually safe and effective for secondary IOL implantation in children but some serious complications have been reported in the literature. They include polypropylene knots erosion through the conjunctiva, endophthalmitis (probably caused by the exposed knots), suture rupture and IOL dislocation although these complications do not occur so frequent in children. (56, 58, 59) Fig, 19 Schematic presentation of the technique of secondary IOL implantation with scleral fixation. E. Iris fixation IOL can be fixated to the iris with the prolene suture or using iris-claw design. Much more common is now iris-claw popularized by Jan Worst. Pediatric and foldable iris-claw IOL’s are now produced. Iris-claw IOL is fixated to the iris in the anterior chamber using grasping mechanism of “claws”. (Fig. 20) The technique of implantation is simple. The lens is introduced into the anterior chamber and peripheral parts of the iris at 3 and 9 o’clock position are enclavated inside the claws. (60) It is also possible to fixate IOL to the back of the iris in posterior chamber. Peripheral iridectomy is performed to prevent papillary block. The advantage of iris-claw IOLs is that it can be fixated to the internal structure of the eye (in opposition to scleral fixated IOLs). The lens can be easily removed and exchanged. Postoperative complications include: papillary ovaling, iris root tear, glaucoma (closure of peripheral iridectomy), lens dislocation and endothelial cell damage, although they occur infrequently with the late generations of iris-claw IOLs. (60) Resistance of the iris tissue to long-term grasping of “claws” and long-term effects of IOL in the anterior chamber on corneal endothelium are yet to be determined. Fig, 20 Schematic presentation of the technique of secondary IOL implantation with iris-claw fixation. Iris suturing of IOLs with polypropylene suture (Fig. 21) is not frequently performed in pediatric cataract surgery. This technique is sometimes used for suturing one haptic of dislocated sclerally fixed IOL because the surgery can be performed through two small openings of the anterior chamber without necessity of preparing new scleral flap for fixation. Fig, 21 Schematic presentation of the technique of secondary IOL implantation with iris fixation. F. Anterior chamber fixation Until recently anterior chamber IOLs (ACIOLs) were not used in pediatric cataract surgery because of frequency of complications associated with the implantation of previous generations of ACIOLs. May be the situation will change with introduction of modern, flexible, open loop ACIOLs but the experience with these IOL designs is still limited. 3. Choice of IOL IOls which are preferred by surgeon for cataract surgery are used for secondary in-the-bag implantation. Special pediatric sized and for patient with microcornea iris-claw IOL’s are now produced for iris fixation. Until now there are no recommendations about the use of IOL for ciliary sulcus and scleral fixation in children. The author preference is Super-flex IOL (Rayner, UK). This IOL is produced from hydrophilic acrylic material has mm and overall length of 12.50 mm and has optic diameter of 6.25 closed loop, complex haptic. Its hydrophilic material ensures the best uveal biocompatibility when in touch with iris tissue (see above). This lens fits better for ciliary sulcus diameter because of enlarged overall diameter comparing to standard IOLs for in-the-bag implantation. Haptics with closed loop, not too elastic, complex system provides good IOL stabilization, centration and adaptation in the cilary sulcus. Closed loop haptic system is also more versatile in use for scleral fixation because polypropylene suture can be tied or looped through the haptics without tying. References 1. GilbertC., Foster A.: childhood blidness in the context of VISION 2020 – The right to sight. Bull WHO 2001; 79:227-232. 2. Seroczyńska M, Prost M, Mędrun J, Łukasiak E, Oleksiak E: The causes of childhood blindness and visual impairment in Poland. Klin Oczna, 2001; 103: 117120. 3. Seroczyńska M., Grałek M., Kanigowska K.: The analysis of the causes of blindness and significant vision loss among children and youth - between 1999 and 2003. Okulistyka, 2004; 4: 58-62 4. Birch EE, Stager DR, Leffler J, Weakley D: Early treatment of congenital cataract minimizes unequivoal competition. Invest Ophthalmol Vis Sci, 1998; 39 1560-1566. 5. Birch, EE, Swanson WH, Stager, DR, Woody M, Everret M: Outcome after early treatment of dense congenital unilateral cataract. Invest Ophthalmol Vis Sci, 1993, 34: 3687-3699. 6. Birch, EE, Stager, DR: The critical period for surgical treatment of dense congenital unilateral cataract. Invest Ophthalmol Vis Sci, 1996, 37: 1532-1538. 7. Chen T C, Walton D S, Bhatia L S: Aphakic Glaucoma After Congenital Cataract Surgery Arch Ophthalmol, 2004, 122: 1819 - 1825. 8. Facciani J, Trivedi RH, Wilson ME: Postoperative glaucoma. in: Wilson ME, Trivedi RH, Pandey SK (eds): Pediatric cataract surgery. Lippincott, Wiliams &Wilkins, 2005. 9. Letocha CE, Pavlin CJ: Follow-up of r patients with Ridley intraocular lens implantation. J Cataract Refract Surg, 199, 25: 587-591. 10. Wilson ME, Bartholomew LR, Trivedi RH: Pediatric cataract surgery and intraocular lens implantation: Practice preferences of the 2001 ASCRS and AAPOS memberships. J Cataract Refract Surg, 2003; 29: 1811-1820. 11. Trivedi RH, Wilson ME: Primary intraocular lens implantation in infantile cataract surgery. in: Wilson ME, Trivedi RH, Pandey SK (eds): Pediatric cataract surgery. Lippincott, Wiliams &Wilkins, 2005. 12. Infants Aphakia Treatment Study www.nei.nih.gov/neitrials/viewStudyWeb.aspx?id=108#Results 13. Dahan E: Pediatric cataract surgery. In: Yanoff M, Duker J.S: Ophthalmology, St.Louis, 2004. 14. Lam DSC, Chua JKH, Leung ATS, Fan DSP, Ng JSK, Rao SK: Sutureless Pars Plana Anterior Vitrectomy Through Self-sealing Sclerotomies in Children. Arch Ophthalmol, 2000, 118: 850-851. 15. Bluestein E.C., Wilson M.E., Wang X.H. et al: Dimensions of the pediatric crystalline lens: implications for intraocular lenses in children. J Pediatr Ophthalmol Strabismus. 1996; 33, 18-20. 16. Wilson M.E., Apple D.J., Bluestein E.C., Wang X.H.: Intraocular lenses for pediatric implantations: biomaterials, designs and sizings. J Cataract Refract Surg, 1994; 20, 584-591. 17. Schmidbauer J.M., Escobar-Gomez M., Apple A.J. et al: Effect of haptic angulation on posterior opacification in modern foldable lenses with square, truncated edge. J Cataract Refract Surg, 2002; 28, 1251-1255. 18. Wilson M.E., Elliot L.A, Peterseim M.M.W. et al: AcrySof acrylic intraocular lens implantation in children: Clinical indications of biocompatibility. JAAPOS; 2001, 5, 377-380. 19. Schmidbauer J.M., Amon M., Kirguer A., et al: Comparison of the biocompatibility of 2 foldable intraocular lenses with sharp optic edges. J Cataract Refract Surg, 2001; 27, 1579-1585 20. Abela-Formanek C., Amon M., Schauersberger J. et al: Results of hydrophilic, hydrophobic and silicone intraocular lenses in uveitic eyes with cataract: Comparison to a control group. J Cataract Refract Surg, 2002; 28, 1141-1152. 21. Abela-Formanek C., Amon M., Schauersberger J. et al: Uveal and capsular biocompatibility of 2 foldable acrylic intraocular lenses in patients with uveitis or pseudoexfolation syndrome: Comparison to a control group. J Cataract Refract Surg, 2002; 28, 1153-1159. 22. Amon M.: Biocompatibility of intraocular lenses. J Cataract Refract Surg, 2001; 27, 850-854. 23. McCulley J.P.: Biocompatibility of intraocular lenses. Eye&Contact Lens: Science & Clinical Practice, 2003; 29, 155-163. 24. Vargas L.G., Peng Q., Apple D.J., Escobar-Gomez M., et al: Evaluation of 3 modern single-piece foldable intraocular lenses: Clinicopathological study of posterior capsule opacification in a rabbit model. J Cataract Refract Surg, 2002; 28, 1241-1250. 25. Prost M.: Biocompatibility of different IOLs in children. Paper presented at XXI Congress of European Society of Cataract and Refractive Surgeons, Munich 2003. 26. McLoone E., Mahon G.,Archer D., Best R.: Silicone oil-intraocular lens interaction: which lens to use?. Br J Ophthalmol, 2001; 85, 543-545. 27. Apple D.J., Isacs R.T., Kent D.G. et al: Silicone adhesions to intraocular lenses: an experimental study comparing various biomaterials. J Cataract Refract Surg, 1997; 23, 536-544. 28. Pandey S.K., Werner L., Wilson M.E. et al: Capsulorhexis ovaling and capsular bag stretch after rigid and foldable intraocular lens implantation: an experimental study in pediatric human eyes. J Cataract Refract Surg, 2004; 30, 2183-2191. 29. Jacobi P.C., Dietlein T.S., Konen W.: Multifocal intraocular lens implantation in pediatric cataract surgery. Ophthalmology, 2001; 108, 1375-1380. 30. Hunter D.G.: Multifocal intraocular lenses in children. Ophthalmology, 2001; 108, 1373-1374. 31. Mainster MA, Sparrow, JR: How much blue light should an IOL transmit? Brit J Ophthalmol, 2003; 87: 1523-1529. 32. Prost M. (ed.): Development of the human eye in children. Children’s Memorial Health Institute Publications, 2000, Warsaw, Poland. 33. Prost M.: IOL power calculation in cataract operations in children. Klin Oczna, 2004, 106: 691-694. 34. Trivedi RH, Wilson ME: Intraocular lens power calculation in children. Magazyn Okulistyczny (Poland), 2005; 4 (8): 294-300. 35. McClathey SK, Hofmeister FM: Intraocular lens power calculation for children. in: Wilson ME, Trivedi RH, Pandey SK (eds): Pediatric cataract surgery. Lippincott, Wiliams &Wilkins, 2005. 36. Hamada S, Walters BC, Nischal K: Two-incision push-pull capsulorhexis for paediatric cataract surgery. Poster presented at 30th Meeting of European Paediatric Ophthalmological Society, Manchester, 14-15 October, 2004. 37. Wilson ME, Bluestein EC, Wang XP, Apple DJ: Comparison of mechanized anterior capsulectomy and manual continuous capsulorhexis in pediatric eyes. J Cataract Refract Surg, 1994; 20:602-606. 38. Luck J, Brahma AK, Noble BA: A comparative study of the elastic properties of continuous tear curvilinear capsulorhexis versus capsulorhexis produced by radiofrequency endodiathermy. Br J Ophthalmol, 1994; 78: 392-396. 39. Morgan JE, Ellington RB, Young RD, Tumal GJ: The mechanical properties of the human lens capsule following capsulorhexis or radiofrequency diathermy capsulotomy. Arch Ophthalmol, 114: 1110-1115. 40. Guo S, Wagner R, Caputo A: Management of the anterior and posterior lens capsule and vitreous in pediatric cataract surgery. J Pediatr Ophthalmol Strabismus, 2004; 41: 330-337. 41. Vasavada AR, Trivedi RH, Apple DJ, Ram J, Werner I: Randomized , clinical trial of multiquadrant hydrodissection in pediatric cataract surgery. Am J Ophthalmol, 2003; 135: 84-88. 42. Trivedi RH, Wilson ME: Posterior capsulotomy an anterior vitrectomy for the management of pediatric cataracts. in: Wilson ME, Trivedi RH, Pandey SK (eds): Pediatric cataract surgery. Lippincott, Wiliams &Wilkins, 2005. 43. Forbes BJ, Guo S: Update on the surgical management of pediatric cataracts. J Pediatr Ophthalmol Strabismus, 2006: 43: 143-151. 44. BenEzra D, Gohen E: Posterior capsulectomy in pediatric cataract surgery: the necessity of choice. Ohthalmology, 1997; 104: 2168-2174. 45. Koch DD, Kohnen T: Retrospective comparison of techniques to prevent secondary cataract formation after posterior chamber intraocular lens implantation in infants and children. J Cataract Refract Surg, 1997; 23 (suppl 1): 657-663. 46. Buckley EG, Klombers LA, Seaber JH, Scalise-Gordy A, Minzter R: Management of the posterior capsule during pediatric intraocular lens implantation. Am J Ophthalmol, 1993; 115: 722-728. 47. Gimbel HV, DeBroff BM: Posterior capsulotomy with optic capture: maintaining a cler visual axis after the pediatric cataract surgery. J Cataract Refract Surg,1994; 20: 658-664. 48. Basti S, Krisnamahary M, Gupta S: Results of sutureless wound construction in children undergoing cataract extraction. J Pediatr Ophthalmol Strabismus, 1996; 33: 52-54. 49. Trivedi RH, Wilson ME: Principles of incision construction in pediatric cataract surgery. in: Wilson ME, Trivedi RH, Pandey SK (eds): Pediatric cataract surgery. Lippincott, Wiliams &Wilkins, 2005. 50. Trivedi RH, Wilson ME: Secondary intraocular lens implantation in children. in: Wilson ME, Trivedi RH, Pandey SK (eds): Pediatric cataract surgery. Lippincott, Wiliams &Wilkins, 2005 51. Wilson, ME, Englert JA, Greenwald MJ: In-the-bag secondary IOL implantation in children. JAAPOS, 1999, 3: 350-355. 52. DeVaro JM, Buckley EG, Avner S, Seaber J: Secondary posterior chamber intraocular lens implantation in in pediatric patients. Am J Ophthalmol, 1997, 123: 24-30. 53. Avad AH, Mullaney PH, Al-Hamad A et al: Secondary posterior chamber intraocular lens implantation in children. JAAPOS, 1998, 2: 269-274. 54. Biglan AW, Cheng KP, Davis JS, Gerontis CC: Secondary intraocular lens implantation after cataract surgery in children. Am J Ophthalmol, 1997, 123: 224234. 55. Vasavada AR, Trivedi RH: Role of optic capture in congenital cataract and intraocular lens surgery in children. J Cataract Refract Surg, 2000, 26: 824-831. 56. Pandey SK, Wilson ME: Transcleral suture fixation of posterior chamber intraocular lenses. in: Wilson ME, Trivedi RH, Pandey SK (eds): Pediatric cataract surgery. Lippincott, Wiliams &Wilkins, 2005. 57. Hofman R: Scleral fixation without conjunctival dissection. Paper presented at XXIV Congress of ESCRS, London, 13.09,2006. 58. Zetterstrom C, Lundvall A, Weeber H, Jeeves M: Sulcus fixation without capsular support in children. J Cataract Refract Surg,1999, 25: 776-781. 59. Mittelviefhaus H, Mittelviefhaus K, Gerling J: Transscleral suture fixation of posterior chamber intraocular lenses in children under 3 years. Graefes Arch Clin Exp Ophthalmol, 2000, 238: 143-148. 60. Singh DA, Singh K, Verma A, Singh RSJ: The iris-claw (Artisan) lens. in: Wilson ME, Trivedi RH, Pandey SK (eds): Pediatric cataract surgery. Lippincott, Wiliams &Wilkins, 2005 Recommended reading 1. Wilson ME, Trivedi RH, Pandey SK (eds): Pediatric cataract surgery. Lippincott, Wiliams &Wilkins, 2005.