Limbs 8 – Lower limb Nerves and Vessels
advertisement

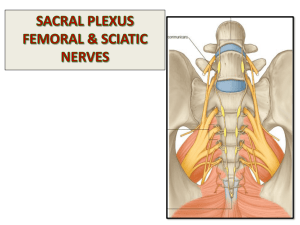
Session 8 – Review of Lower Limb Nerves and Vessels Neurology of Lower Limb: Function of the lumbro-sacral plexus is parallel to brachial plexus Includes the anterior rami of L2-S4 L2-L4 – femoral and obturator nerves L4-S3 – sciatic nerve Femoral and peroneal nerves are posterior divisions of the spinal nerve roots Obturator and tibial nerves are anterior divisions of the spinal nerve roots Compression of the spinal roots often results after lumbar disc injury – pain is felt down route of affected nerve. L4 or L5 is common leading to sciatica Destruction of the sciatic nerve in the buttock – flaccid paralysis of hamstrings, paralysis of all muscles below the knee and loss of most sensation below the knee Injury to common peroneal nerve – paralysis of extensor and peroneal compartment of leg results in foot drop accompanied by loss of sensation over most of antero-lateral leg and dorsum of foot Injury to the femoral nerve – nerve relatively superficial in groin and rarely damged except by doctors (iatrogenic injuries) – commonest during hip replacements or repair of inguinal hernias Meralgia paraesthetica is caused by compression of the lateral cutaneous nerve as it passes 2cm medial to the anterior superior iliac spine at the level of the inguinal ligament Obturator nerve is rarely damaged – pain along distribution of nerve is often sign of pelvic malignancy Injury to the superior gluteal nerve – supplies gluteus minimus and medius so damage causes Tredelenberg gait where the pelvis lurches during ealking. Commonest injury through hip replacement as only lies 5cm from tip of great trochanter Injury to sciatic nerve – commonest cause is hip replacement. The peroneal division more at risk than tibial division. To avoid injury injections are always given in the upper lateral quadrant of buttock. Injury to common peroneal nerve – damage at the level of the hip and as winds round the fibular neck – damage from trauma, knee replacement and plaster cast compression The tibial nerve runs deep so is rarely damaged alone Injury to the saphenous nerve is common – often damaged at the medial malleolus after varicose vein surgery or at the knee after ACL surgery Anaesthetic nerve blocks – include femoral, sciatic, ankle, lateral cutaneous nerve. Vessels of the Lower Limb: Femoral hernias pass into the femoral canal which is medial to the femoral vein in the femoral sheath The femoral artery and vein can be cannulated in the groin In a shocked patient cannulation may not be easy – the anatomical surface marking of the long saphenous (2cm above and proximal to the tip of the medial malleolus) may be cut-down – a small incision is made and a venous cannular placed in under direct vision Acute arterial embolism can be caused by sudden occlusion of an atherosclerotic vessel or by AF thrombus – if sudden and so no time for collateral circulation to develop distal tissue becomes ischaemic, and necrotic if the clot is not cleared in hours (e.g. popliteal artery can lead to amputation) Intermittant claudication is where gradual occlusion of the arteries within the limb occurs. The muscles distal become ischaemic during exercise causing pain Compartment syndromes: Can occur anywhere in leg, but most common in lower leg The three compartments of the leg – anterior, posterior and lateral are bound by very tight fascia which only let the enclosed muscles well to a certain degree before resisting further expansion Fractures of soft tissue injuries can lead to a rise in compartmental pressure This causes the arterial supply and venous drainage in that compartment to be shut off resulting in muscle death, loss of movement and contractures Acute compartment syndrome occurs after trauma to a limb such as surgery or fracture. Unless the fascia is released surgically by fasciotomy the muscle will die Arterial pulse is not lost in acute compartment syndrome - pressure only needs to rise from 25mmHg to 60mmHg to cause compartment syndrome when arterial pressure is 120/80mmHg Chronic compartment syndrome occurs in athletes where the muscle swells and causes activity related pain Varicose Veins and deep venous insufficiency: Superficial veins and perforating veins have valves to prevent backflow from deep system The most important valve is at the sapheno-femoral junction If valves become incompetent blood flows back into the superficial system causing varicose veins Varicose veins are dilated and tortuous superficial veins Can be painful and cause discomfort on standing Increased pressure in the veins may become pathological causing skin changes (lipodermatosclerosis) and skin ulcers due to venous insufficiency Page 1 Deep Vein Thrombosis: When thrombosis occurs in the deep veins Often silent but may present with pain and swelling in calf or proximal thigh A distal DVT occurs in the calf, proximal DVT extends into thigh and pelvis Proximal DVT is very dangerous as risk of propagation into the lungs Can occur idiopathically but is associated with immobility, trauma, surgery of the abdomen pelvis or limbs, obesity, malignancy, pregnancy and use of the pill The main consequences are – propagation to the lungs leading to PE or increased back pressure in the deep veins casuing venous insufficiency and leg ulcers (post-phlebitic syndrome) Superficial vens may also clot or become inflamed/infected – superficial thrombophlebitis which is less dangerous than DVT but very painful Superficial veins as grafts in elective surgery: The saphenous veins are often used in cardiac and vascular surgery as grafts Need to be orientated correctly due to presence of valves As there is excellent anastomoses in the leg the removal of the superficial veins rarely causes a problem Page 2