WS Sample
advertisement

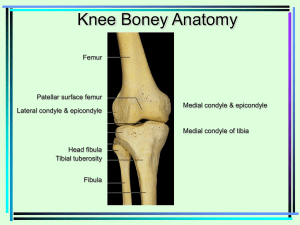
Laurel Greenfield (Ortho) PAMF Samples <BODY> The patient comes in today for a referral from Dr. Richard Sandor from the Camino Medical Group in Mountain View. Comes in today for bilateral knee pain. She states that she has had no specific injury. She has had 1 year of discomfort and pain with predominantly of the left greater than right knee pain. The pain is anteriorly. Denies any locking or catching episodes. She states that she has difficulty getting up from the floor when sitting or climbing stairs. She complains of some crepitation. Has gotten some physical therapy. Has also had previous MRIs that have been done on both knees. She comes in today for treatment and care. CURRENT MEDICAL PROBLEMS: The patient denies any history of hypertension, diabetes, seizures, heart murmurs, or asthma. CURRENT MEDICATIONS: None. ALLERGIES: None. SURGICAL HISTORY: 2 C-sections in January 2004 and May 2008. TOBACCO USE: None. ALCOHOL USE: None. PHYSICAL EXAMINATION: A 33-year-old, right-hand dominant female who stands 5 feet, weighs 150. She is in no apparent distress. Physical examination of the right lower extremity shows a 1+ effusion. She has no erythema or ecchymosis. She has motion of zero degrees of extension, 130 degrees of flexion. No anterior or posterior drawer. No medial or lateral joint line tenderness. 1+ patellofemoral crepitation. MRI of the right knee shows a large effusion. No meniscal tear. Shows a contusion of the lateral femoral condyle, and her MRI was performed on July 2, 2009. Physical examination of left knee shows 1+ effusion. No erythema or ecchymosis. She has motion of zero degrees of extension, 130 degrees of flexion. No anterior or posterior drawer. No medial or lateral joint line tenderness. 1+ patellofemoral crepitation. MRI of the left knee from June 18, 2009 shows a large effusion, no meniscal tear. ASSESSMENT: Bilateral chondromalacia of the patella. RECOMMENDATION AND PLAN OPTIONS: A long discussion was carried out with the patient, and greater than 50 percent of the time during today’s 45-minute consultation was spent counseling the patient in regards to her diagnoses and her treatment alternatives. She was given brochures and information, instructed on exercise program to follow. Discussed options such as the possibility of viscosupplementation, and the possibility of future surgical intervention with her. At this point in will continue with her exercise program, and she should follow back up with Dr. King on as-needed basis. </BODY> <BODY> Patient was seen in conjunction with Dr. King as a new patient, previously seen by Melissa Fought. He comes in today for his right ankle. He is a 29-year-old male who sustained a right ankle inversion injury sustaining initially a syndesmotic disruption, underwent an open reduction internal fixation with 2 large frag screws. He states that after he had had the surgery, he fell down the stairs 2 weeks later and sustained a medial malleolar fracture. He underwent a second surgery to have a reduction. He comes in today with continued discomfort and pain anteriorly in the ankle and would like to have his hardware removed. PHYSICAL EXAMINATION: RIGHT LOWER EXTREMITY, RIGHT ANKLE: He is neurovascularly intact. He has no erythema or ecchymosis. He has dorsiflexion of zero, plantar flexion 20, inversion 15, eversion is 10. His incision sites are clean, dry and intact. He has no erythema. He does have some noted swelling. ASSESSMENT: Right ankle impingement syndrome, post open reduction internal fixation, 2 syndesmotic screws and 2 medial malleolar screws. RECOMMENDATION AND PLAN OPTIONS: Options surgical and nonsurgical were discussed. A long discussion was carried out with him in regards to his treatment and care, surgical and nonsurgical. At this time, he would like to proceed with surgical intervention undergoing a right ankle arthroscopy with debridement with removal of 2 large frag screws. He will be scheduled for surgery in August. In the meantime, activity modification, pain free, was recommended, and he will follow up with us at that time. </BODY> <BODY> He comes in for examination. Right knee post ACL reconstruction with allograft with lateral meniscal reconstruction with meniscal allograft June 10, 2009. States he is doing much better. Has not started therapy yet or a CPM. He has been on his crutches and his knee brace. On examination, he has a 1+ effusion. His wound sites are clean, dry, and intact. He has -3 degrees of extension, 40 degrees of flexion. ASSESSMENT: Right knee post ACL reconstruction with lateral meniscal reconstruction. RECOMMENDATION AND PLAN: Begin CPM machine. Begin some physical therapy. Given instructions and a prescription. Instructions on wound care were discussed, and he should follow back up with Dr. King in 4 weeks for reexamination/reassessment. He knows he can contact us if he has any questions or concerns. </BODY> <BODY> Gordon comes in today for examination of his left knee. He is a 27-year-old, right-hand-dominant male who noticed left knee discomfort and pain while working on a fishing boat. 20-foot boat, fishing, lifting nets and heavy activities; started having some discomfort and soreness. He comes in today for treatment and care. CURRENT MEDICAL PROBLEMS: The patient denies any history of hypertension, diabetes, seizures, heart murmur, or asthma. Does have a history of acid reflux. CURRENT MEDICATIONS: 1. Aleve. 2. Valerian and valerian root. ALLERGIES: None. SURGICAL HISTORY: 4, 2009. Jaw surgery in 1998, right knee surgery March TOBACCO USE: None. ALCOHOL USE: Occasional. REVIEW OF SYSTEMS: acid reflux. 13-point review of systems contributory to EXAMINATION: 27-year-old, right-hand-dominant male stands 5 feet 9 inches, weighs 170 pounds. He is ambulatory with no assistive devices. Examination of the left lower extremity showed no effusion. Motion +2 degrees extension, 135 degrees of flexion. No anterior posterior drawer. No Lachman. No pivot. 1+ medial joint line tenderness, no lateral joint line tenderness. ASSESSMENT: Left knee possible medial meniscus tear, chondromalacia. RECOMMENDATION, PLAN, OPTIONS: A long discussion was carried out with the patient in regards to treatment and care. At this time would like to proceed with an MRI. He was sent downstairs for an MRI and came back for reevaluation. MRI 2nd evaluation did show a medial meniscal tear and options were discussed with him. At this time he would like to proceed with undergoing a diagnostic and operative arthroscopy, partial medial meniscectomy, possible meniscal repair. He will be scheduled for surgery in July. In the meantime activity modification, pain free, were recommended and discussed, and he will followup with Dr. King postoperatively. </BODY> <BODY> REASON FOR ADMISSION: Right shoulder diagnostic and operative arthroscopy revision, acromioplasty, capsulolabral reconstruction repair, anterior capsulorrhaphy, and SLAP repair as indicated. CHIEF COMPLAINT: Right shoulder pain. HISTORY OF PRESENT ILLNESS: This is a 39-year-old, right-handdominant female who has a history of right shoulder multidirectional instability with ligament laxity. She has had 5 previous surgeries; the last surgery was 17 years ago. She states that she continues to have instability, but pain has changed and has increased. She was seen and evaluated by Dr. King on May 26, 2009. She was diagnosed with right shoulder multidirectional instability with ligament laxity and post previous failed surgery with new onset of right shoulder rotator cuff tendinitis and hooked acromion. A long discussion had been carried out with her in regard to her treatment and care, surgical and nonsurgical, and the risks and complications. At this time she would like to proceed with surgical intervention undergoing a right shoulder diagnostic and operative arthroscopy, acromioplasty, revision capsulolabral reconstruction repair, capsulorrhaphy, and SLAP repair as indicated. CURRENT MEDICAL PROBLEMS: A history of psoriatic osteoarthritis, bipolar disorder, and bleeding ulcers. Also a history of postoperative surgical nausea. Diabetes: None. Hypertension: None. CURRENT MEDICATIONS: acid. ALLERGIES: Methotrexate, Femara, Depakote, and folic DEMEROL. SURGICAL HISTORY: Shoulder surgeries x5, stomach surgery, tubal ligation, and breast reductions. SOCIAL HISTORY: Tobacco use: None. Alcohol use: None. PHYSICAL EXAMINATION: A 40-year-old right-hand-dominant female who stands 5 feet 3 inches, weighs 185 pounds. CHEST: Clear. There were no wheezes or rales that were appreciated and her heart had a regular rate and rhythm. There were no murmurs, rubs, or gallops to be noted. RIGHT UPPER EXTREMITY AND THE RIGHT SHOULDER: Forward elevation to 170. External rotation at 90 is 90. Internal rotation at 90 is 90. Supraspinatus strength testing 5/5. External rotation testing 5/5. She has a 1+ positive apprehension with Hawkins, 1+ pain, 2+ cross-body, trace AC tenderness, and positive O’Brien test. IMAGING: MRI of the right shoulder was reviewed with the patient. She has type III hooked acromion, AC arthritis, rotator cuff tendonitis, labral tears, and metallic artifact. ASSESSMENT: Right shoulder impingement syndrome with recurrent subluxation anterior with a flap tear. RECOMMENDATION AND PLAN OPTIONS: Options and treatment alternatives were discussed. At this time would like to proceed with surgical intervention undergoing a right shoulder diagnostic and operative arthroscopic, acromioplasty with revision capsulolabral reconstruction, capsulorrhaphy, and SLAP repair as indicated. The patient was told of the diagnosis and was given a choice of the treatment options available. The patient was told of the surgical and the nonsurgical treatment options, as well as the risks and benefits associated with each of the treatment options. Prior to the patient giving consent the patient expressed an understanding of the diagnosis and the treatment options, both surgical and nonsurgical. The patient's questions were answered. With an expressed understanding of the diagnosis and the treatment alternatives the patient requests surgical intervention. </BODY> <BODY> PHYSICAL EXAMINATION: 34-year-old, right-hand-dominant male who stands 5 feet 4 inches, weighs 170 pounds. Ambulatory with no assistive devices. Examination of the left upper extremity is neurovascularly intact. No erythema or ecchymosis. He has 2+ tenderness over the lateral epicondyle. Increased pain with resistance with extension. 1+ tenderness over the medial epicondyle with no pain with flexion. ASSESSMENT: Left elbow lateral epicondylitis greater than medial epicondylitis. RECOMMENDATIONS AND PLAN OPTIONS: Options and treatment alternatives were discussed with an expressed understanding of the risks associated with the cortisone injection. He would like to proceed. After sterile prep, 1 cc of 1 percent lidocaine mixed with 0.5 cc of Kenalog was injected over the lateral epicondyle. He was told to modify his activities, continue with a good stretching and strengthening program, and he needs to follow back up with Dr. King in 4 weeks for reevaluation. </BODY> <BODY> DATE OF ADMISSION: July 15, 2009 REASON FOR ADMISSION: Left knee diagnostic and operative arthroscopy with partial lateral meniscectomy as well as anterior cruciate ligament reconstruction with allograft as indicated. CHIEF COMPLAINT: Left knee pain. HISTORY OF PRESENT ILLNESS: This is a 49-year-old female who has had left knee injury, April 22, 2009. She had some instability episodes. She was initially seen by Dr. Ted Omura who had referred her in to be seen by Dr. King. She had an MRI which showed a complete tear of the anterior cruciate ligament with a torn lateral meniscus. Options were discussed with her, surgical and nonsurgical, as well as the risks and complications. At this time she would like to proceed with surgical intervention undergoing a left knee diagnostic and operative arthroscopy with anterior cruciate ligament reconstruction with allograft with partial lateral meniscectomy as indicated. CURRENT MEDICAL PROBLEMS: Patient has a history of hypothyroidism. Denies any history of hypertension, diabetes, seizures, or heart murmurs or asthma. CURRENT MEDICATIONS: ALLERGIES: Multivitamins. None. SURGICAL HISTORY: Tobacco use, none. Jaw surgery 15 or 20 years ago. Alcohol use, occasional. 13-point review of systems contributory towards sinus, hemorrhoids, and premenopausal. PHYSICAL EXAMINATION: 49-year-old, left-hand dominant female who stands 5 feet 2 inches, weighs 123 pounds. She is ambulatory with no assistive devices. Her chest was clear. There were no wheezes or rales appreciated, and her heart had a regular rate and rhythm. There were no murmurs, rubs, or gallops noted. Examination of her left lower extremity of her left knee, shows that she is neurovascularly intact. No erythema or ecchymosis. She has motion zero degrees extension, 135 degrees of flexion, 2+ anterior drawer, 2+ Lachman’s, 1+ lateral joint line tenderness, no medial joint line tenderness. MRI shows a complete tear of the anterior cruciate ligament with a torn lateral meniscus. ASSESSMENT: Left knee torn lateral meniscus, torn ACL. RECOMMENDATION AND PLAN: Options, surgical and nonsurgical, were discussed as well as the risks and complications. At this time she would like to proceed with surgical intervention undergoing a left knee diagnostic and operative arthroscopy with partial lateral meniscectomy, ACL reconstruction as indicated. The patient was told of the diagnosis and was given a choice of the treatment options available. The patient was told of the surgical and the nonsurgical treatment options as well as the risks and benefits associated with each of the treatment options. Prior to the patient giving consent, the patient expressed an understanding of the diagnosis and the treatment options, both surgical and nonsurgical. The patient's questions were answered. With an expressed understanding of the diagnosis and the treatment alternatives, the patient requests surgical intervention. </BODY> <BODY> CHIEF COMPLAINT: Right knee pain. New patient. HISTORY OF PRESENT ILLNESS: 50-year-old, right-hand-dominant female comes in with right knee pain that began June 1998 playing basketball, fell. Told that she had torn meniscus. She elected no surgery at that time. She states that now she has some swelling and some clicking in her knee. Comes in today for opinion and treatment and care. CURRENT MEDICAL PROBLEMS: Patient denies any history of hypertension, diabetes, seizures, heart murmurs, or asthma. CURRENT MEDICATIONS: SURGICAL HISTORY: ALLERGIES: Allegra. Negative. NONE. TOBACCO USE: None. ALCOHOL USE: None. 13-point review of systems is negative. PHYSICAL EXAMINATION: 50-year-old right-hand-dominant female who stands 5 feet 2 inches, weighs 155 pounds, ambulatory, no assistive devices. Examination of the right lower extremity shows trace effusion. Neurovascular status intact. No erythema or ecchymosis. She has motion 0 degrees extension, 130 degrees of flexion. No anterior or posterior drawer. No Lachman's or pivot. 2+ medial joint line tenderness. 1+ lateral joint line tenderness. No varus or valgus instability. 1+ patellofemoral crepitation. ASSESSMENT: Right knee probable chondromalacia, possible meniscal tear. RECOMMENDATION AND PLAN OPTIONS: Options and treatment alternatives were discussed. At this time, would like to proceed with an MRI. She will have an MRI performed to rule out possible meniscal tear and will then follow up for reexamination and reassessment. In the meantime, activity modifications, pain-free, were recommended. She was given brochures and information about the meniscus and will follow up with us for MRI. </BODY>