Appendix A
advertisement

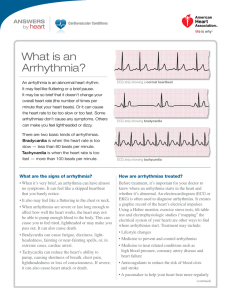
Appendix A. – Inclusion and Exclusion Criteria for Telemetry Monitoring INCLUSION: TELEMETRY UNIT: Indication for admission to a telemetry-monitored bed: a. Hemodynamically stable patient with unstable angina or non ST elevation myocardial infarction (NSTEMI). b. Syncope that is suspected to be cardiac in origin. c. Assessment, monitoring, and control of significant arrhythmias (e.g. ventricular or supraventricular tachycardia, bradycardia, atrial fibrillation with rapid ventricular response) requiring medical therapy. d. Assessment and monitoring of patients with drug or chemical toxicity known to cause cardiac arrhythmias (e.g. tricyclic antidepressants, phenothiazines, digitalis, antiarrhythmic drugs). e. Assessment and monitoring of patients post coronary intervention(s). f. Assessment and monitoring of patients waiting urgent revascularization (either PCI or CABG). g. Assessment and monitoring of patients pre and post-electrophysiology study that require control of arrhythmias. h. Assessment and monitoring of patients immediately post-pacemaker or AICD implantation. i. Assessment and monitoring of patients with suspected pacemaker or AICD malfunction. j. Assessment and monitoring of patients receiving I.V. inotropic agents (e.g. dobutamine in heart failure). k. Assessment and monitoring of patients with acute myocarditis. l. Patients transferred from a critical care unit who require continued arrhythmia monitoring. 1 EXCLUSIONS: Cardiac monitoring is not indicated for the following: Patients who have been stable and arrhythmia free for 48 hours of consecutive monitoring. Patients admitted with a diagnosis of “rule out acute coronary syndromes” who are pain free and who have a normal electrocardiogram or one that is unchanged form previous tracing and no elevation of cardiac biomarkers. Post operative patients who are at low risk for arrhythmia such as young patients after uncomplicated surgery that does not involve cardiopulmonary bypass. Patients who are terminally ill and not candidates for therapy of arrhythmias (e.g. patients with “do not resuscitate” orders). Patients undergoing routine, uncomplicated (diagnostic) coronary artery catheterization. Patients with chronic stable atrial fibrillation. Patients with asymptomatic ventricular ectopy who are hospitalized for non-cardiac causes Patients with pacemakers and/or AICD who are not suspected of having device malfunction. Patients with identified non-cardiac causes of syncope, near syncope or dizziness. Patients with stable congestive heart failure. Patients admitted for respiratory ailments such as asthma or pneumonia, without underlying heart disease. PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft; AICD, automated implantable cardioverter defibrillator; IV, intravenous 2 Appendix B. Criteria for Discharge from Telemetry Unit Discharge criteria may vary due to the complexities of the clinical population, but some suggestions for the timing of discharges include: 1. 2. 3. Clinical stabilization of acute decompensated heart failure. Stabilization or resolution of arrhythmias by medical therapy or device (pacemaker or AICD) Negative cardiac enzymes and a negative stress test in a patient with chest pain and a low or intermediate probability for angina. 4. No further chest pain in patients who have an uncomplicated myocardial infarction who have been observed for 2 to 4 days post MI in either the CCU or in one of the cardiac step down units. 5. Absence of arrhythmias after 48 hours of monitoring in patient’s with syncope or suspected arrhythmias. 6. 24 hours post insertion of a permanent pacemaker if there were no device problems and device has been evaluated post implantation. 3