Coroners report PICC line AR summary Feb 10
advertisement
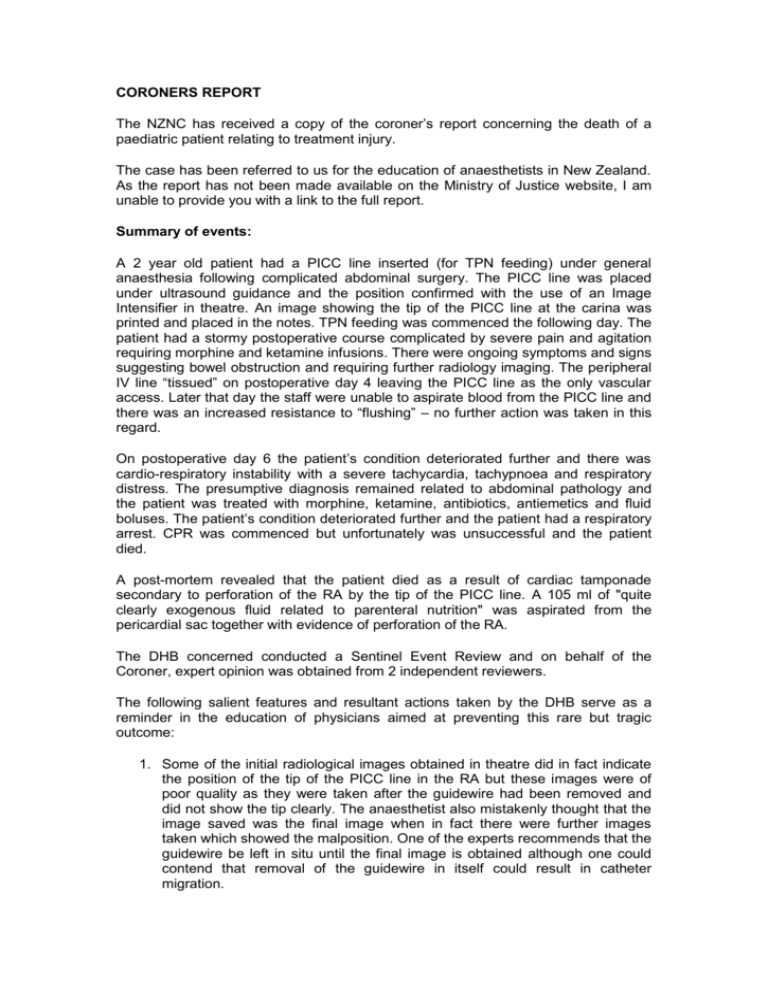
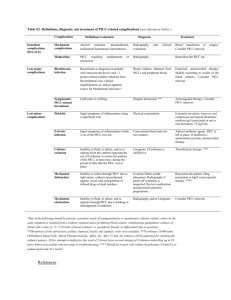
CORONERS REPORT The NZNC has received a copy of the coroner’s report concerning the death of a paediatric patient relating to treatment injury. The case has been referred to us for the education of anaesthetists in New Zealand. As the report has not been made available on the Ministry of Justice website, I am unable to provide you with a link to the full report. Summary of events: A 2 year old patient had a PICC line inserted (for TPN feeding) under general anaesthesia following complicated abdominal surgery. The PICC line was placed under ultrasound guidance and the position confirmed with the use of an Image Intensifier in theatre. An image showing the tip of the PICC line at the carina was printed and placed in the notes. TPN feeding was commenced the following day. The patient had a stormy postoperative course complicated by severe pain and agitation requiring morphine and ketamine infusions. There were ongoing symptoms and signs suggesting bowel obstruction and requiring further radiology imaging. The peripheral IV line “tissued” on postoperative day 4 leaving the PICC line as the only vascular access. Later that day the staff were unable to aspirate blood from the PICC line and there was an increased resistance to “flushing” – no further action was taken in this regard. On postoperative day 6 the patient’s condition deteriorated further and there was cardio-respiratory instability with a severe tachycardia, tachypnoea and respiratory distress. The presumptive diagnosis remained related to abdominal pathology and the patient was treated with morphine, ketamine, antibiotics, antiemetics and fluid boluses. The patient’s condition deteriorated further and the patient had a respiratory arrest. CPR was commenced but unfortunately was unsuccessful and the patient died. A post-mortem revealed that the patient died as a result of cardiac tamponade secondary to perforation of the RA by the tip of the PICC line. A 105 ml of "quite clearly exogenous fluid related to parenteral nutrition" was aspirated from the pericardial sac together with evidence of perforation of the RA. The DHB concerned conducted a Sentinel Event Review and on behalf of the Coroner, expert opinion was obtained from 2 independent reviewers. The following salient features and resultant actions taken by the DHB serve as a reminder in the education of physicians aimed at preventing this rare but tragic outcome: 1. Some of the initial radiological images obtained in theatre did in fact indicate the position of the tip of the PICC line in the RA but these images were of poor quality as they were taken after the guidewire had been removed and did not show the tip clearly. The anaesthetist also mistakenly thought that the image saved was the final image when in fact there were further images taken which showed the malposition. One of the experts recommends that the guidewire be left in situ until the final image is obtained although one could contend that removal of the guidewire in itself could result in catheter migration. 2. Even though the tip is considered to be adequately positioned when at the SVC/RA junction this position is still within the pericardial reflection and erosion could still result in tamponade. As mentioned by one of the independent experts, the ideal position is above the pericardial reflection in the SVC which in most patients would be at the level of the tracheal bifurcation. This position presumes that there is no error of parallax during radiological imaging and does not account for movement of the tip which occurs with movement of the upper limb in the post-insertion period. 3. This malposition (tip of PICC in RA) was consistently present on the subsequent postoperative radiology films but not mentioned in the radiology reports as the indication for this imaging was investigation of abdominal pathology related to presumptive surgical complications. This DHB now recommends that all patients having a PICC line inserted should have this reported on by a Radiologist within 24 hrs of insertion. In addition, all films showing a PICC line in situ must have the position reported. Both these recommendations are part of an ongoing audit process. 4. There has been an education drive to increase awareness of the complications of PICC lines and their treatment as well as more stringent monitoring of these lines on the ward. 5. Policies regarding the credentialing of operators for insertion of PICC lines and the taking of blood samples from these catheters are also being reviewed. 6. A regular audit process has been established to assess adherence to these recommendations. 7. PICC lines are more prone to movement than central lines and the position of the tip is a contentious issue. Too proximal a position is also associated with serious complications and some authorities have in fact recommended a more distal placement. A case report published in the BJA [BJA 99(3): 384-8 (2007)] has a discussion and references outlining these controversies. CORONER’S RECOMMENDATIONS: 1. The DHB consider Radiology support in theatre at the time of insertion or an immediate follow up CXR to confirm position as standard practise. 2. That when a PICC line is used for TPN administration an alternative intravenous line be obtained for blood sampling and other drug administration. This is often impractical, and could result in significant morbidity in some cases, as the reason for PICC line insertion is often due to impossible peripheral IV access. As with many of these cases involving tragic outcomes we must caution against overly stringent guidelines and regulations which often don’t decrease the inherent procedural risk to the patient but do act to decrease patient access to procedures and treatment.