Preoperative Learning Guide
advertisement
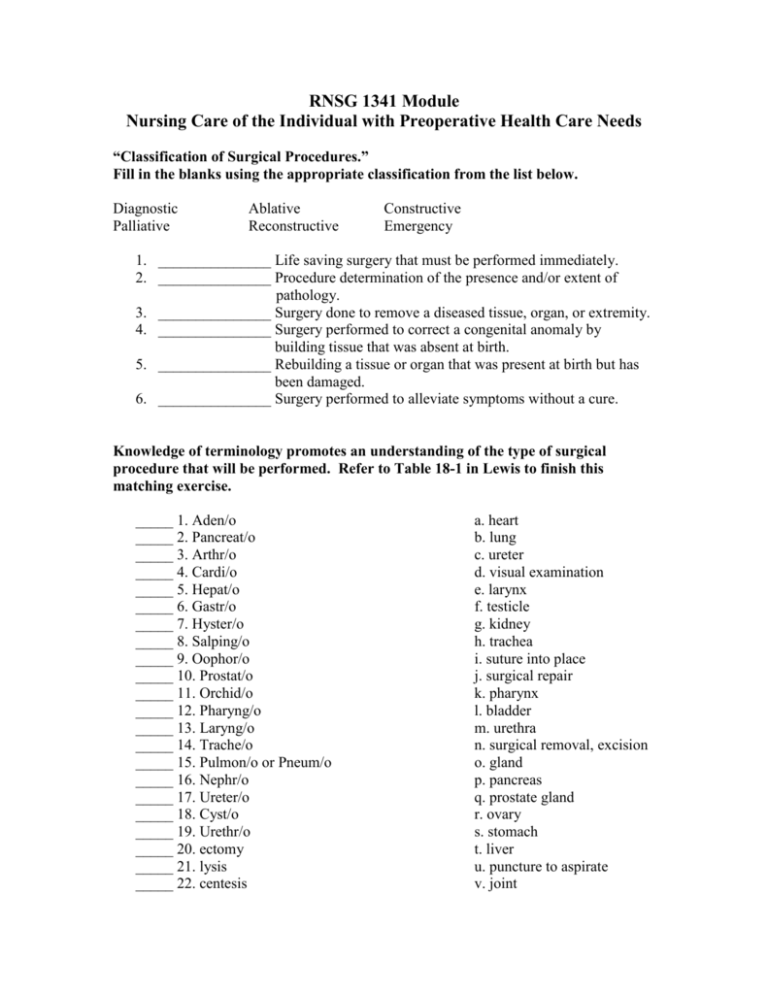
RNSG 1341 Module Nursing Care of the Individual with Preoperative Health Care Needs “Classification of Surgical Procedures.” Fill in the blanks using the appropriate classification from the list below. Diagnostic Palliative Ablative Reconstructive Constructive Emergency 1. _______________ Life saving surgery that must be performed immediately. 2. _______________ Procedure determination of the presence and/or extent of pathology. 3. _______________ Surgery done to remove a diseased tissue, organ, or extremity. 4. _______________ Surgery performed to correct a congenital anomaly by building tissue that was absent at birth. 5. _______________ Rebuilding a tissue or organ that was present at birth but has been damaged. 6. _______________ Surgery performed to alleviate symptoms without a cure. Knowledge of terminology promotes an understanding of the type of surgical procedure that will be performed. Refer to Table 18-1 in Lewis to finish this matching exercise. _____ 1. Aden/o _____ 2. Pancreat/o _____ 3. Arthr/o _____ 4. Cardi/o _____ 5. Hepat/o _____ 6. Gastr/o _____ 7. Hyster/o _____ 8. Salping/o _____ 9. Oophor/o _____ 10. Prostat/o _____ 11. Orchid/o _____ 12. Pharyng/o _____ 13. Laryng/o _____ 14. Trache/o _____ 15. Pulmon/o or Pneum/o _____ 16. Nephr/o _____ 17. Ureter/o _____ 18. Cyst/o _____ 19. Urethr/o _____ 20. ectomy _____ 21. lysis _____ 22. centesis a. heart b. lung c. ureter d. visual examination e. larynx f. testicle g. kidney h. trachea i. suture into place j. surgical repair k. pharynx l. bladder m. urethra n. surgical removal, excision o. gland p. pancreas q. prostate gland r. ovary s. stomach t. liver u. puncture to aspirate v. joint _____ 23. orrhaphy _____ 24. oscopy _____ 25. ostomy _____ 26. otomy _____ 27. plasty _____ 28. pexy _____ 29. cholecyst/o _____ 30. herni/o w. uterus x. fallopian tube y. incision, cutting into z. making an artificial opening a2. setting free, relief of b2 abnormal protrusion c2. suturing, repairing d2. gallbladder Based on your review of the common surgery related suffixes, prefixes, and word roots provided, write a simple definition of the following surgical procedures. 1. Hysteropexy – 2. Gastroscopy – 3. Nephrostomy – 4. Arthroplasty – 5. Prostatectomy – 6. Tracheotomy – 7. Herniorrhaphy – 8. Cholecystectomy 9. Lysis of adhesions 10. Thoracentesis - Place a check mark beside each item that correctly addresses the statement provided. 1. Items that describe Outpatient Surgery: _____ a. Site where most minor surgical procedures are performed _____ b. Ability to return home the day of the procedure reduces stress for many patients _____ c. Procedures performed cause less disruption of family and work schedules _____ d. The most common complication resulting from surgery at these locations is infection _____ e. There is more time for assessments and patient teaching because the procedures are less complex 2. Items that describe Inpatient Surgery: _____ a. The site where more complex surgeries are performed _____ b. Procedures performed here are more expensive due to the need for complex equipment and supplies, staff trained to perform more complex skills and varied tasks, and extended stay in the facility _____ c. Prolonged stay decreases the patient’s risk for complications such as infection _____ d. Procedures performed here are more likely to be classified as major, urgent or emergency in nature _____ e. Patients having surgery here are more likely to need IV therapy, blood transfusions, physical and respiratory therapy, referral for assistance with home care, or detailed postoperative teaching 3. Items necessary for informed consent for a surgical procedure: _____ a. Have a family member or friend witness the patient’s signing of the consent form even if this occurs after the patient has been transported to surgery. _____ b. The patient may sign the form anytime prior to the performance of the procedure. _____ c. If the patient is a minor, is unconscious, or is mentally incompetent to sign the permit, the written permission may be given by a legally appointed representative or responsible family member. _____ d. For consent to be informed, the patient must have been informed and must understand the nature of the surgery, the qualifications of the surgeon, the risks of the procedure, the chances for success, alternate methods available for treatment of the problem, as well as the right to refuse or withdraw consent at anytime. _____ e. There is no circumstance in which a physician can perform surgery without the signature of the patient or next of kin. 4. Responsibilities of the nurse related to obtaining informed consent: _____ a. Describing the steps of the procedure that the surgeon will perform, the exact organs that will be removed or endangered as a result of the procedure, and the potential complications. _____ b. Obtaining the patient’s signature and the signature of the person actually seeing the patient sign the form.. _____ c. Signing as a witness to the patient’s signature if no family member is available. _____ d. Clarifying simple issues of misunderstanding that the patient or family may have prior to the signing of the consent form. _____ e. Encouraging the patient to not sign the form if there are many or major misunderstandings about the procedure, risks, benefits, and expected outcomes of the surgery or anesthesia. _____ f. Notifying the surgeon and/or anesthesiologist about major concerns expressed by the patient or family members so that additional teaching and clarification can be completed prior to signing the form. 5. Current beliefs about preoperative fasting provided by the American Society of Anesthesiologists in regard to healthy patients preparing for elective surgery: _____ a. all patients must be NPO after midnight prior to any surgical procedure. _____ b. clear liquids and appropriate oral medications may be taken 2 hours prior to surgery. _____ c. tea and toast may be taken 6 hours prior to surgery and a heavier meal 8 hours prior to surgery. _____ d. aspiration is no longer considered a risk associated with general anesthesia. 6. The preoperative cardiovascular nursing assessment must include: _____ a. history of known cardiovascular disorders _____ b. assessment of vital signs, heart sounds, and pulses _____ c. assessment for edema and JVD _____ d. identification of prescription and non-prescription preparations that impact cardiovascular function and risk for bleeding. _____ e. review of the diagnostic test findings 7. Prior to surgery, the routine respiratory data collection should include: _____ a. assessment for signs and symptoms of infection and history of previous serious and chronic respiratory illnesses. _____ b. use of prescription and non-prescription medications as well tobacco products. _____ c. assessment of rate and character of respirations _____ d. assessment of breath sounds, shape of the chest, and use of accessory muscles. _____ e. review of the available diagnostic test findings addressing respiratory function. _____ f. collection of sputum to test exposure to TB and other pathogens. 8. The preoperative assessment of the integumentary system and nutritional status includes: _____ a. assessment of skin and mucosa for lesions, color, moisture, hydration, temperature, and makeup that would hinder assessment of circulation. _____ b. assessment of boney pressure points for redness and ulcers. _____ c. completion of skin scrub and shaving of the surgical site by the patient prior to admission. _____ d. assessment of oral cavity for dentures, loose teeth, and infection. _____ e. presence of gag and swallow reflexes _____ f. NPO status and time that last food and liquids were consumed. _____ g. intake of own medications and dietary supplements in the last 3 weeks as well as the AM of surgery. _____ h. patient’s recall of his/her height and weight. 9. The preoperative neurological and muscular assessments should include: _____ a. orientation to person, place and time. _____ b. checking for indications of confusion, disorderly thinking, and inability to follow simple two part commands. _____ c. assessment for abuse of alcohol and other substances. _____ d. history of hearing and/or visual impairment. _____ e. determination of muscle strength and joint function _____ f. determination of ability to ambulate, ambulatory aids, gait, balance, and usual activity level. _____ g. determination of the patient’s ability to drive himself/herself home after the procedure or hospital stay. 10. Each patient’s preoperative bowel and bladder preparation includes: _____ a. assessment of ability to void and history of urinary track infections. _____ b. checking usual bowel patterns including date and type of last bowel movement. _____ c. abdominal assessment for shape, lesions, presence and character of bowel sounds in each quadrant, and palpation for firmness and discomfort. _____ d. administration of antibiotics such as neomycin for several days prior to surgery. _____ e. administration of enemas until clear the night prior to surgery. _____ f. administration of a bowel prep drink such as Go-Lytely the night prior to surgery. _____ g. insertion of a Foley catheter for all patients having general anesthesia. 11. Preoperative teaching relating to pain management: _____ a. should be avoided because it frightens the patient and increases the pain / anxiety cycle. _____ b. informs the patient that the nurses will administer doses of pain medication based on his pulse rate and blood pressure. _____ c. stresses the need for early medication before the pain becomes too severe. _____ d. emphasizes that the patient should not be expected to experience pain greater than 3 on the 0 to 10 rating scale. _____ e. includes the fact that the patient will be expected to rate and describe his pain each time vital signs are measured, each time he requests a pain medication, and after each intervention to relieve his pain. _____ f. informs the patient not to worry about addiction until pain control is achieved and the wound is healed. 12. Teaching preoperative exercises will help the surgical patient by: _____ a. allowing time to learn them prior to administration of pain medications and discomfort that focuses the patient’s attention away from learning. _____ b. providing a means by which the patient can participate in the prevention of complications. _____ c. increasing his strength, joint function, and weight reduction. _____ d. decreasing the need to assess for a positive Homan’s sign. Write the name(s) of the common preoperative diagnostic test(s) on the line next to the purpose for performance. RBC, H & H Blood Sugar BUN, Creatinine Pregnancy WBC Platelets Serum Electrolytes ECG Chest X-ray PT/INR & PTT AST/ALT Type & Crossmatch ABG’s & Pulse ox. Cholinesterase Urinalysis 1. _______________ determines the patient’s ability to combat infection. 2. _______________ measures the patient’s ability to transport oxygenate to the tissues. 3. _______________ determines the patient’s ability to metabolize drugs administered to paralyze muscles thus his ability to regain movement and respiratory function after surgery. 4. _______________ indicates the level of kidney function. 5. _______________ indicates effectiveness of respiratory function. 6. _______________ indicates the need for insulin & predicts wound healing problems. 7. _______________ helps to identify risk for cardiac malfunction which would make the patient more likely to experience complications such as shock or cardiac arrest. 8. _______________ indicates the liver’s ability to metabolize many medications given during the surgical procedure. 9. _______________ indicates the patient’s risk for hemorrhage. 10. _______________ helps to identify if certain procedures can be performed or if certain medications can be safely administered in order to protect an unborn child. 11. _______________ prepares blood or blood products that may be needed to replace loss prior to, during, or after surgery. Match the following NANDA Stems with the assessment data, related to statements, and interventions provided. Hint – some items may have more than one answer. A. B. C. D. E. Knowledge deficit Anxiety &/or fear Anticipatory grieving Coping, ineffective Family process, interrupted PERSON Data _____ 1. Shy, 15 year old female, first admission to a hospital and first surgical experience, in bed fully dressed in her street clothes with covers pulled up to her chin, parent shouting at the patient stating that her behavior is ridiculous _____ 2. History of chronic lung disease, smoked 2 packs a day for the last 44 years, joking about already missing his cigarettes, respirations increased from 22 at rest to 30 / minute when assisted to the bathroom to void, wheezing with course crackles noted on auscultation, unable to effectively deep breathing and cough _____ 3. Tense facial expression, eyes red with tears evident when speaks about the need to be separated from her 3 year old daughter and 7 month old son, verbalizes concern about care that will be provided at her in-laws home _____ 4. States, “I feel like I will no longer be considered attractive by my spouse after this surgery is performed. This will be a very hard thing to face in our home.” _____ 5. “When I had my last surgery in 1953, I wasn’t allowed to get out of bed for about 6 days. Why isn’t rest needed anymore? How can a wound heal if I have to exercise and walk around. Won’t the wound open up?” Related to statements _____ 1. related to lack of previous experience with a specific procedure _____ 2. related to serious concern about the outcome of the procedure _____ 3. related to concerns about family finances S/T cost of hospitalization and need for a prolonged recovery period _____ 4. related to embarrassment and reluctance to frankly discuss concerns with significant other Typical nursing interventions _____ 1. Use active listening and open ended statements to promote the patient’s ability to verbalize concerns _____ 2. Use simple or common terminology when stating the rational for tasks being performed and information being presented _____ 3. Offer to help the patient call a trusted friend or offer to call social services or the Hospital Chaplin for the patient _____ 4. Sitting at the bedside, demonstrate the postoperative exercises and have the patient perform a return demonstration _____ 5. Provide basic information about community services available to patients having the scheduled procedure _____ 6. Assess what the patient knows or understands about the scheduled procedure and the information to be taught _____ 7. Ask the client how he/she has managed difficult experiences in the past and identify what has been most helpful _____ 8. Inform the patient that you will explain each procedure again when it is time to perform it _____ 9. Acknowledge and value the patient’s feelings and if appropriate, ask the patient, “What do you hope for?” _____ 10. Communicate concern but avoid giving ‘false hope.’ Using Lewis, indicate the contributing factor(s) and appropriate intervention(s) for each of the following surgical risks. Contributing Factor(s) _______________ Surgical Complication 1. Delayed wound healing or dehiscence Nursing Intervention(s)_ _______________________ _______________ 2. Hemorrhage ________________________ _______________ 3. Shock ________________________ _______________ 4. Atelectasis and pneumonia ________________________ _______________ 5. Infection ________________________ _______________ 6. Formation of clots and emboli ________________________ Identify the preoperative drug described by the following actions. You may need to use your drug guide as a reference for this exercise. Bicitra Pepcid Reglan Versed Prevacid Atropine Morphine 1. Suppresses gastric acid secretion ___________________________________ 2. Reduces gastric acid volume and ______________________________________ concentration 3. Promotes gastric emptying ___________________________________________ 4. Decreases vomiting and aspiration _____________________________________ by drying the mouth and respiratory tract 5. Decreases anxiety but causes respiratory _______________________________ depression and hypotension 6. Causes both sedation and extrapyramidal _____________________________ or involuntary movements and changes in muscle tone 7. Increases the pH and reduces the volume ______________________________ of gastric fluid in patients with GERD 8. Induces amnesia, drowsiness and lack of ______________________________ coordination Indicate whether the following statements are true or false. _____ 1. Use of herbal “dietary supplements” is increasingly common in the United States and patients who use them often do not think of them as medicines to be reported prior to surgery. _____ 2. Patients may not be aware that herbal “dietary supplements” can cause serious complications during or after surgery. _____ 3. Herbal preparations are primarily used by preoperative patients from cultural groups that have recently entered the United States. _____ 4. It is best to administer the preoperative medication prior to describing the surgical risks and prior to asking the patient to sign the permit for surgery. _____ 5. Ambulating a preoperative patient to the bathroom after the administration of a narcotic or sedative may result in falls due to postural hypotension. _____ 6. The most common preoperative medications in current use include the IM administration of Morphine or Demerol. _____ 7. All preoperative patients are taught that they will have to cough and deep breathe every 2 hours while awake. _____ 8. Calf pumping and quadriceps setting are exercises that are considered essential for the prevention of blood clots in the lower extremities. _____ 9. Obtaining the patient’s baseline vital sign range helps the nurse to better evaluate his response to the multiple stressors experienced in the surgical and postoperative periods. _____ 10. Patients allergic to shellfish are at high risk for allergy to iodine based cleansers used for surgical scrub skin preparation.