Three-Level Anterior Cervical Discectomy and Fusion
advertisement

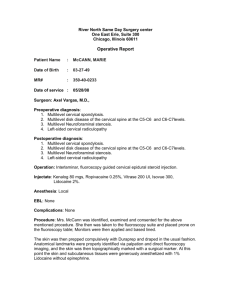
Le Rachis, May 2008 Three-Level Anterior Cervical Discectomy and Fusion with a monobloc Cage-and-plate device. Clinical and Radiographic Results Cédric BARREY1,2, MD ; Eduardo PIASSI1, MD, Hélene BELLIARD1, MD ; Gilles PERRIN1,2, MD 1 Department of Neurosurgery, P. Wertheimer Neurosurgery Hospital, Lyon, France 2 Claude Bernard Lyon I University, Lyon, France Corresponding author: Cédric Barrey, MD Service de Neurochirurgie C 59 Boulevard Pinel, Hôpital P Wertheimer, 69003 Lyon, France Email: c.barrey@wanadoo.fr or cedric.barrey@chu-lyon.fr Fax: (33) 4 72 35 72 62 Tel: (33) 4 72 35 70 43 None of the authors or their divisions or departments received anything of value for this study. Three-level anterior cervical discectomy….. 2 TEXT Introduction Anterior cervical discectomy and fusion (ACDF) using bone graft and anterior plate has become the gold standard procedure in cases of radiculopathy and myelopathy consecutive to cervical spondylosis 4,7,9,23 Robinson and Smith22introduced the procedure of anterior discectomy and fusion in 1955, and Cloward3 described his alternative technique in 1958. ACDF allows ventral decompression, maintenance of intervertebral height, restoration of lordosis and arrest of osteophytes formation23 while the use of an anterior cervical plate provides better stabilization resulting in increased fusion rates and less graft collapse and migration. The introduction of interbody cages reduced donor site morbidity and avoided bone graft collapse11,12,24. Good and excellent outcomes following instrumented ACDF involving one or two levels has been widely reported in the literature14,16. In contrast, multilevel ACDF with plate and cage has demonstrated rates of heterogeneous results for treatment of multilevel cervical spondylosis, i.e. involving more than two intervertebral levels1,2,6,10,16,14,25. The overall mechanical failure is significantly higher as the number of involved levels increased. Particularly, non-union of the fusion is a significant problem and the rate of pseudarthrosis for three-level or more procedures has been reported as high as 20-50 % in the literature.5-7 Some authors assess that the high rate of pseudarthrosis is related to the increased number of bone graft-endplate interfaces13. Therefore, recommendations for alternative methods to increase fusion rates have been proposed. This prompted the modification of burring the endplates down to subchondral bone; causing a 4.4% decrease in the pseudarthrosis rate per level5. An other alternative is to perform corporectomy instead of multilevel discectomy resulting in less bone graft-endplate interfaces. However reconstruction procedure following corpectomy may be challenging with significant mechanical complications21,25. Finally some authors advocate the need for supplemental stabilization by posterior approach14. Although multilevel cervical spondylosis is not a rare issue, few reports have recently focused on the results of multilevel discectomy with interbody cage fusion2,8,10,18. The purpose of this study 2 Three-level anterior cervical discectomy….. 3 was to evaluate the clinical and radiographic outcomes of a group of patients undergoing three-level ACDF with a monobloc cage-and-plate construct. Methods From March 1998 to May 2007, there were 35 surgical cases of multilevel (= or > 3) cervical degenerative disease in our unit, over a total of 632 cases of ACDF during the same period. We reviewed the 21 cases who underwent ACDF with a monobloc cage-and-plate device for three-level cervical degenerative diseases, and who had a minimum of 12 months’ follow-up. Excluded were patients who received autogenous bone graft, or underwent additional posterior procedures, or had inadequate follow-up, and other different surgical techniques. No patient had a history of previous cervical spine surgery. The average age of the patients was 50.46 years [43-66]. There were 14 men and 7 women. The average follow-up period was 18 months [12-114]. The levels involved were C3-C6 in 3 patients (14.3%), C4-C7 in 16 (76.2%), and C5-T1 in 2 (9.5%). A total of 63 levels were fused. Demographic data are shown in Table 1. Preoperative symptoms were recorded and categorized (Table 2). The group underwent multilevel anterior discectomy according to Smith-Robinson22procedure. Gardener-Wells tongs were used with 7 lb of axial traction. Following control X-ray, we performed right-sided longitudinal skin incision and then exposure of the cervical spine was basically carried out by anterior approach. Each level could be exposed by using a static retractor which was replaced at each level during the surgey to avoid excessive esophagus retracting. Following discectomy, we typically opened the posterior longitudinal ligament under microscopic control and we resected osteophytes. Cartilaginous endplates were gently drilled using diamond-burr under permanent irrigation, with respect of subchondral bone. A Cloward distraction device enlarged the disc space during the decompression step. Stabilization was performed using a monobloc cage-and-plate device at each decompressed level. The PCB® implant, Scient’x, Guyancourt, France, consists of a titanium-made one-piece cervical device 3 Three-level anterior cervical discectomy….. 4 with an hollow intradiscal spacer and an integrated plate (fig 1). The plate is gently angled to restore lost cervical lordosis and plate’s wings are arranged obliquely to permit application to adjacent levels in multilevel fusion. Three sizes of PCB® implants are currently available: 12mm (Width) x 5.5mm (Height), 12 x 7.0 mm and 15 x 7.0 mm. The appropriate size of cage was impacted through the disc space resulting in segmental intervertebral distraction. The upper borders of the spacer’s lateral surfaces have a convex configuration for optimal contact with the concave lower surface of the vertebra above Two screws, one cranial and one caudal, were then inserted in adjacent vertebral bodies. Finally, following insertion of the device, the cage was filled with porous biphasic ceramic, composed of tricalcium phosphate and hydroxyapatite granules, for fusion. Blood loss and operation time were recorded. All patients wore a soft cervical collar for about 8 weeks post-operatively. In all patients in this series follow-up exams were done at 2, 6, 12 months and more after surgery with clinical and radiographic examinations of cervical spine. VAS and Odom’s criteria were used at the latest followup to assess the clinical outcome (Table 3). All 21 patients had been examined radiographically by Xray imaging, i.e. anterior-posterior, lateral, flexion, extension films whereas 17 (81%) patients out of 21 also underwent computerized tomographic imaging (CT) with multiplanar reconstructions (fig 2 and 3). X-ray radiographic assessment of fusion was defined according to the following criteria : the absence of motion (less than 2 mm) between the spinous processes of the fused levels on flexion and extension views, absence of any dark halo around a cage on both anterior-posterior and lateral radiographs. A level was considered as fused on the CT-scan when the three following criteria were presents: 1- Absence of radiolucencies surrounding the implants; 2- Absence of cyst formation; 3Trabecular bone formation across the interspace.17 We checked the lateral view of X-ray to evaluate the spinal curve. The sagittal alignment of the cervical spine (C2-C7) as well as the segmental alignment of the three operated levels was measured with the Cobb method both before, after surgery and at last follow-up. Changes in sagittal alignment were calculated and averaged for the entire group. Radiographic measurements were 4 Three-level anterior cervical discectomy….. 5 performed preoperatively, 2 months after surgery and at final follow-up. Statistical differences between preoperative and postoperative parameters were sought using the Mann-Whitney test (ordinal data). All statistical analysis was performed using InStat 3.05 (GraphPad Software Inc., San Diego, CA). The p value was considered significant when p < 0.05. Results Data on 21 consecutive patients undergoing a three-level ACDF with the monobloc cage-andplate device between 1998 and 2007 were included into the study. There were no hardware complications in this series of patients. There was no loosening, migration, telescoping or failure of the instrumentation. There were no infections, incidences of pneumonia, or other medical complications. There were no patients with increased neurological deficit. A patient presented with prevertebral hematoma and required an additional surgery for drainage, without sequelae. The blood loss and operation time in the group were 325 ± 163 ml [125-600] and 159 ± 80 minutes [68-330], respectively. Patient outcomes graded by Odom’s criteria are presented in Table 4. According to Odom’s criteria, 13 patients had an excellent outcome, 7 good, 1 fair and none poor. Satisfactory outcome (excellent + good) was found in 95.2% of patients in this series. Sixteen (100%) of the 16 patients with radiculopathy and 4 (80%) of the 5 patients with myelopathy had a satisfactory result. Overall, fusion was achieved in 51 of 63 levels in 17 of 21 patients within the first 6 months after surgery, and in 58 of 63 levels before the 12-month follow-up visit. In four patients who did not undergo CT examination, fusion criteria were checked based on static and dynamic X-rays according to the aforementioned protocol. Analysis of radiographs (table 5) demonstrated that the preoperative global cervical lordosis (C2-C7) was 9 ± 3° [-15-20], whereas it was 19 ± 2° [10-30] at the final follow-up; p = 0.023. According to preoperative versus final follow-up measurements, the average increase in cervical lordosis was 10 ± 6° [3-25]. The preoperative segmental instrumented lordosis was 6 ± 2° [-5-10] whereas it was 15 ± 4° [3-33] at the final follow-up; p = 0.013. According to preoperative versus final 5 Three-level anterior cervical discectomy….. 6 follow-up measurements, the average increase in segmental instrumented lordosis was 9 ± 8° [0-26]. A loss of cervical lordosis correction between first postoperative control at 2 months, 22 ± 5° [17-30], and final follow-up control, 15 ± 7° [10-25], was observed in 5 patients (27.8 %) according to X-ray measurements. The average loss of correction in these patients amounted 7 ± 2.5° [5-10], however the difference was not significant, p = 0.172. Discussion First of all,. we have to keep in mind that three or more levels ACDF is a relatively rare procedure representing less than 5 % of all anterior cervical surgical procedures performed for degenerative cases in our unit (31/632 cases). Surgical stabilization after multilevel discectomy procedure may be challenging with a high rate of pseudarthrosis or mechanical failure in comparison to 1 or 2-level procedure5-7,25. Emery et al.6 specifically reported three-level procedures in 16 patients, noting primary arthrodesis of all the three levels in 9 (56%) patients. Wang et al.24 reported the pseudarthrosis rate for non plated 3-level discectomy as high as 37% whereas 18% (7 of 40) of patients had pseudarthrosis after 3-level plated ACDF. Graft collapse with autogenous bone is also reported in 20 to 30% of cases after multilevel fusion procedures. Even in Bolesta’s report1, the nonunion rate was as high as 47% (7 of 15) of patients for 3-and 4-level discectomy with plate fixation. With recent progresses of instrumentation, interbody cages and plates, recent studies reported improvement of fusion success rates. Samartzis et al.20 reported a 94.7% fusion rate after three-level discectomy and fusion with a plating device and Khoueir et al.13 showed 100% fusion in 38 patients with 2- and 3-level discectomy and fusion using a collagen-hydroxyapatite matrix with iliac crest bone marrow aspirate. Our findings were consistent with the two last cited studies. The higher rates of fusion reported in most recent papers is probably relative to the development of efficient fixation systems and adequate bone substitutes. Interbody cages provide initial segmental stability by tensioning the ligamentous apparatus through as initial distraction and supports axial load and without risk of collapse. 6 Three-level anterior cervical discectomy….. 7 In comparison to multilevel ACDF and plating, multilevel corpectomy decreased the number of bone graft/endplates interfaces as demonstrated in figure 4. Therefore some authors advocated realisation of 2-level corpectomy rather than 3-level discectomy and fusion. However, corpectomy with strut graft reconstruction generates a large moment arm at the ends of the construct, potentially leading to plate migration or dislogement. Singh et al21 carried out an in vitro biomechanical study comparing the stability of anterior plate fixation following 3-level discectomy and two-level corpectomy. Segmental plate fixation was significantly more rigid in flexion-extension and lateral bending than end-construct plate fixation with a mean gain of rigidity around 10-15 % in flexionextension and 40 % in axial rotation under the testing conditions. In addition, the increase number of bone-graft interfaces with multilevel ACDF provides a load-sharing effect at each level with less risk of implant telescoping, as observed in our study. Otherwise, multilevel ACDF and plating provides segmental intervertebral distraction (figure 4) which results in restoration of intervertebral and foraminal height at each level. More importantly, we can control the amount of distraction effect at each level during the procedure. In contrast, Global distraction following corpectomy and strut graft reconstruction may lead to asymetrical distraction with potential radicular damage. In our series, we noted no radicular deficit in particular no C5 or deltoid deficit whereas this is a classical complication following anterior corpectomy and reconstruction procedure. Also, multilevel ACDF and plating demonstrated its efficacity to improve the sagittal balance. Indeed, in our series the mean cervical lordosis was significantly increased after surgery and maintained at the last follow-up in most cases. Lordosis can be optimally restored and maintained at the instrumented spinal segment because the device provide multiple points of distraction and fixation (fig2). The interbody space shape and the possibility to increase angulations of plate’s wings are also helpful to restore segmental lordosis. Some studies reported that multilevel ACDF was more efficient in restoring lordosis than multilevel corpectomy. According to us multilevel ACDF and plating has the following advantages over multilevel corpectomy : - segmental intervertebral distraction 7 Three-level anterior cervical discectomy….. 8 - more rigid construct - more simple decompression and reconstruction procedures Obviously, in some cases multilevel corpectomy cannot be avoided (vertebral body deformity, retrolisthesis, severe fixed kyphosis). However we do not recommend multilevel corpectomy just to decrease the number of bone/graft interfaces. In our study, the use of a cage-and-plate construct with biphasic ceramic after discectomy provided several advantages, including the absence of donor site complications, an easier implantation technique, minor tracheal, vascular, or esophageal injures, and good immediate and long-term stabilization. In addition both blood loss and operation time in group were comparable to data reported in the literature. An other significant advantage is that the device is spontaneously retained within the disc space thus avoiding a potentially disastrous consequences of posterior implant’s migration. In conclusion, Multilevel ACDF using a monobloc cage-and-plate construct appeared to be a safe and effective device for interbody fusion in multilevel cervical degenerative diseases through this preliminary experience. It restored cervical stability and cervical lordosis, while providing solid fusion and satisfactory clinical and radiographic outcomes. Further prospective comparative studies with the gold standard surgical technique are now required to confirm the findings of the present study. 8 Three-level anterior cervical discectomy….. 9 References 1. Bolesta MJ, Rechtine GR, Chrin AM (1999) Three- and Four-level anterior cervical discectomy and fusion with plate fixation: a prospective study. Spine 25:2040-2046 2. Cho DY, Lee WY, Sheu PC(2004) Treatment of multilevel cervical fusion with cages. Surg Neurol 62:378-386 3. Cloward RB. The anterior approach for removal of ruptured disks (1958) J Neurosurg 15:602-614 4. Edwards CC, Riew KD, Anderson PA, Hilibrand AS, Vaccaro AR (2003) Cervical myelopathy: current diagnostic and treatment strategies. Spine J 3:68-81 5. Emery SE, Bolesta MJ, Banks MA, Jones PK (1994) Robinson anterior cervical fusion comparison of the standard and modified techniques. Spine 19:660-663 6. Emery SE, Fisher JR, Bohlman HH (1997) Three-level anterior cervical discectomy and fusion: Radiographic and clinical results. Spine 22:2622-2685 7. Emery SE. Cervical spondylotic myelopathy: diagnosis and treatment (2001) J Am Acad Orthop Surg 9:376-88 8. Hacker RJ, Cauthen JC, Gilbert TJ, Griffith SL (2000) A prospective randomized multicenter clinical evaluation of an anterior cervical fusion cage. Spine 25:2646-2655 9. Hillard VH, Apfelbaum RI (2006) Surgical management of cervical myelopathy. Indications and techniques for multilevel cervical discectomy . Spine J 6:242S-251S 10. Hwang SL, Lin CL, Lieu AS, Lee KS, Kuo TH, Hwang YF, Su YF, Howing SL (2004) Threelevel and four-level anterior cervical discectomy and titanium cage-augmented fusion with and without plate fixation. J Neurosurg Spine 2:160-167 11. Kaiser MG, Haid RW Jr, Subach BR, Barnes B, Rodts GE Jr (2002) Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurg 50:229-238 12. Katsuura A, Hukuda S, Imanaka T, Miyamoto K, Kanemoto M (1996) Anterior cervical plate used in degenerative disease can maintain lordosis. J Spinal Disord 9:470-476 9 Three-level anterior cervical discectomy….. 10 13. Khoueir P, Oh BC, DiRisio DJ, Wang MY (2007) Multilevel anterior cervical fusion using a collagen-hydroxyapatite matrix with iliac crest bone marrow aspirate : An eighteen-month follow-up study. Neurosurg 61:963-70 14. Koller H, Hempfing A, Ferraris L, Maier O, Hitzl W, Metz-Stavenhagen (2007) 4- and 5-level anterior fusions of the cervical spine: review of the literature and clinical results. Eur Spine J 16:2055-2071 15 Lopez-Espina CG, Amirouche F, Havalad V (2006) Multilevel cervical fusion and its effect on disc degeneration and osteophyte formation. Spine 31:972-978 16 Papadopoulos EC, Huang RC, Girardi FP, Synnott K, Cammisa FP (2006) Three-level anterior cervical discectomy and fusion with plate fixation: radiographic and clinical results. Spine 31:897-902 17 Ploumis A, Mehbod A, Garvey T, Gilbert T, Transfeldt E, Wood K (2006) Prospective assessment of cervical fusion status: plain radiographs versus CT-scan. Acta Orthop Belg 72:342-346 18 Profeta G, de Falco R, Ianniciello G, Profeta L, Cigliano A, Raja AL (2000) Preliminary experience with anterior cervical microdiscectomy and interbody titanium cage fusion in patients with cervical disc disease. Surg Neurol 53:417-426 19 Samandouras G, Shafafy M, Hamlyn PJ (2001) A new anterior cervical instrumentation system combining an intradiscal cage with an integrated plate: an early technical report. Spine 26:1188-1192 20Samartzis D, Shen FH, Matthews DK, Yoon ST, Goldberg EJ, An HS (2003) Comparison of allograft to autograft in multilevel anterior cervical discectomy and fusion with rigid plate fixation. Spine J 3:451-459 21. Singh K, Vaccaro AR, Kim J, Lorenz EP, Lim TH, An HS (2004) Enhancement of stability following anterior cervical corpectomy: a biomechanical study. Spine 29:845-849 22.Smith GW, Robinson RA (1958) The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 40:607-624 23 Stewart TJ, Schlenk RP, Benzel EC (2007) Multiple level discectomy and fusion. Neurosurg 60:S143-S148 24 Wang JC, McDonough PW, Kanim LE, Endow KK, Delamarter RB (2001) Increased fusion rates with cervical plating for three-level anterior cervical discectomy and fusion. Spine 26:643-647 10 Three-level anterior cervical discectomy….. 11 25 Wang JC, Hart RA, Emery SE, Bohlmann HH (2003) Graft migration or displacement after multilevel cervical corpectomy and strut grafting. Spine 28:1016-1021 11 Three-level anterior cervical discectomy….. 12 Fig 1 12 Three-level anterior cervical discectomy….. 13 Fig 2 13 Three-level anterior cervical discectomy….. 14 Fig 3 14 Three-level anterior cervical discectomy….. 15 3-level ACDF Multilevel cervical spondylosis Bone-graft interfaces: n = 6 Segmental Intervertebral distraction +++ Hybrid construct Or 2-level corpectomy Bone-graft interfaces: n = 2 Global Intervertebral distraction +++ Fig 4 15 Three-level anterior cervical discectomy….. 16 Figures legend Figure 1 Monobloc PCBTM cage-and-plate device Figure 2. Illustrative case of radiculopathy. A: Lateral X-Ray film revealing C5 –T1 DDD with loss of physiological cervical lordosis. B: CT sagittal slice. C: Sagittal MR image revealing multilevel spondylosis. D and E: Postoperative lateral and AP x-ray films revealing restoring of segmental lordosis. F: Postoperative computed tomography scan obtained at 1 year demonstrating segmental fusion at the three operated levels. Figure 3. Illustrative case of myelopathy. A: Lateral X-Ray film revealing C4-C7 DDD with loss of physiological cervical lordosis. B: Sagittal MR image demonstrating multilevel spondylosis with spinal cord compression. C: Sagittal postoperative MR image demonstrating satisfying cord decompression. D: Postoperative CT scan obtained at 1 year demonstrating intervertebral fusion at all the instrumented levels. E and F: Extension and flexion radiographs obtained at 6 months revealing no motion at the fusion segment, with the correct positionning of cage-and-plate devices. Figure 4 Surgical treatment altenatives by anterior approach in presence of mulilevel cervical spondylosis. Abbreviations ACDF - anterior cervical discectomy and fusion CT - computerized tomography DDD - degenerative disc disease MR - Magnetic resonance 16 Three-level anterior cervical discectomy….. 17 Table1. Demographic Data in Patients Group n° of patients 21 Age, mean (yr) Range (yr) Sex (M) 50.46 [43-66] 14 (66.6%) Sex (F) 7 (33.3%) Levels Evaluated C3-4 3 (4.8%) C4-5 19 (30.2%) C5-6 C6-7 C7-D1 Total operated levels 21 (33.3%) 18 (28.6%) 2 (3.2%) 63 Clinical Presentation Radiculopathy Myelopathy 16 (76.2%) 5 (23.8%) Table 2. Symptoms and Findings in Patients Group Radiculopathy Patients (n=16) Myelopathy Patients (n=5) Symptoms Arm and neck pain Arm pain only 13 2 3 2 Neck pain only No pain Subjective weakness Numbness 0 0 2 5 0 1 1 3 Neurological findings 7 4 Gait disturbances Lumbar spine symptoms 0 3 1 4 17 Three-level anterior cervical discectomy….. 18 Table 3. Odom's Criteria Excellent All preoperative symptoms relived; abnormal findings improved. Good Minimal persistence of preoperative symptoms; abnormal findings unchanged or improved. Fair Definite relief of some preoperative symptoms; other symptoms unchanged or slightly improved. Poor Symptoms and signs unchanged or exacerbated. Table 4. Clinical Outcome Evaluated by Odom's Criteria in Group Radiculopathy, n=16 Myelopathy, n=5 Excellent 10 (62.5%) 3 (60%) Good 6 (37.5%) 1 (20%) Fair 0 1 (20%) Poor 0 0 Satisfactory outcome 16 (100%) Satisfactory outcome: Excellent + Good 4 (80%) Table 5. Radiographic Results Cervical Lordosis (°) Segmental Instrumented Lordosis (°) Patients With Loss of Lordosis, n = 5 (°) Preop. 2 months Final follow-up 9±3 20 ± 4 19 ± 2 (p=0.033) (p=0.023) 18 ± 8 15 ± 4 (p=0.007) (p = 0.013) 22 ± 5 15 ± 7 (p=0.028) NS (p=0.373) 6±2 8±4 Segmental Instrumented Lordosis = Cervical lordosis to level of the setting op. = operation 18