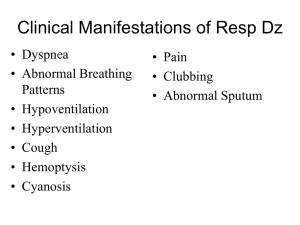
Physical examination of the chest
advertisement

Physical examination of the chest The chest indicates the region that lies under the neck and above the abdomen. Chest wall is composed of sternum, ribs, and vertebras. The anterior part is a little shorter than the posterior part. Chest examination includes many components: chest shape, chest wall, breasts, vessels, mediastinum, bronchus, lung, pleura, heart, and lymph nodes, etc. In addition to general physical examination, the following check methods have been widely used in clinical work: X-ray topography, lung function test, blood-gas analysis, aetiology, histology, and relevant bio-chemical tests. These methods can provide early stages of abnormality and pathogens, even give out exact diagnosis on pathology and pathogenesis, but, many changes in palpation, percussion and auscultation for all kinds of rales, can not be detected through these methods so they can’t completely replace the basic physical examinations till now. The basic physical examination has long been used clinically, which doesn’t need high-quality equippment, handy for use to provide important information and signs for the diagnosis of the chest diseases. Of course, a correct diagnosis depends not only on the basic physical examination, but also other supplementary examinations and the ill history should be emphasized in synthetical consideration. Traditional physical examination of the chest includes four methods, inspection, palpation, percussion and auscultation. The examination should be performed in warm circumstance with well light. The patient should expose the chest to the full, in sitting or supine position according to the need for the examination or the ill condition, and be examined thoroughly with the sequence of inspection, palpation, percussion and auscultation. In general, the anterior and the lateral part is examined first, then the posterior part, this may overcome the tendency that only percussion and auscultation be cared but inspection and palpation be overlooked and avoid omission of any significant sign. A.. Landmark on chest wall The chest contains important organs such as lung and heart. Examination of chest aims to determine the physiologic and pathophysiologic situations of these organs. The position of each organ inside the chest can be determined by examining the surface of the chest. To mark the underlying organ, and detect the position and range of the abnormalities, it is quite important to make well aquaintance with the natural landmarks and artificial lines, with which the underlying structure and abnormalities can be exactly located on the chest wall. I Bone landmark Suprasternal notch: Above the manubrium sterni. In normal condition trachea is in this notch. Manubrium sterni: a piece of hexagon bone at the top of the sternum. Its upper part connects bilaterally to the sternal end of each clavicula, while its base part connects to the sternum. Sternal angle: Also termed Louis angle. It is formed by the protrusion of the conjunction composed of sternum and manabrium sterni. It connects bilaterally to each of the right and left second costal cartilage. It acts as an important landmark for counting rib and interspace, and indicates the bifurcation of the trachea, the upper level of the atria of heart, the demarcation of upper and lower part of mediastinum, and the fifth thoracic vertebra as well. Suprabdominal angle: also termed infrasternal angle, denotes the angle formed by the bilateral rib rows (composed of the seventh to tenth costal cartilage joining bilaterally) which meet at the lower end of the sternum. It corresponds to the dome part of the diaphragm. Normally this angle is approximately 70°- 110°,narrower in slender and wider in dumpy persons, and it also widens slightly during deep inspiration. The underlying region contains the left lobe of liver, stomach and pancreas. Xiphoid process: the protrusive triangular part of the lower end of the sternum with its base connects to the sternum. The length of xiphoid process in normal subject varies widely. Rib: a total of 12 pairs. Each connects to the corresponding thoracic vertebra with its posterior end. The ribs run obliquely to the lateral and then to the anterior direction, with smaller oblique angle above and larger angle lower. Each of the 1-10 rib connects to the relevant cartilage and the sternum, constructing the bony framework of the chest. The eleventh and the twelfth rib do not connect to the sternum and thus are called free ribs. Intercostal space (interspace): The space between two adjacent ribs, used to mark the position of any lesion. Beneath the first rib is the first interspace, beneath the second rib the second interspace, and so forth. Most ribs are palpable over the chest wall except for the first one because its anterior portion is overlapped by the clavicula and usually unpalpable. Scapula: lies between the second and the eighth rib on the posterior chest wall. The hillock and shoulder ridge of the scapula is palpated easily. Its inferior end is called inferior angle. When the patient is in standing position with his arms hanging naturally, the inferior angle acts as the mark of the seventh or the eighth rib, or corresponds to the eighth thoracic vertebra. Spinous process: marks the posterior midline. The seventh cervical spinal process at the base of the neck is most prominent, usually serves as the hallmark for counting the thoracic vertebrae which start just following it. Costolspinal angle: constructed by the twelfth rib and the spine. The kidney and ureter lies in the region in front of this angle. II Vertical line landmarks Anterior midline: namely midsternal line, a vertical line through the middle of the sternum running from its top at the middle point of the upper ridge of the manubrium sterni and running down vertically through the middle of the xiphoid process. Midclavicular line (left, right): vertical line drawn through the middle point of each clavicula, e.g. the vertical line running through the middle point of the clavicula between its shoulder end and sternal end. Sternal line (L, R): vertical line runs along the vertical edges of the sternum and parallels to the anterior midline. Parasternal line (L, R): Vertical line at the middle of sternal line and midclavicular line. Anterior axillary line (L, R): vertical line drawn downward through the anterior axillary fold along the anteriolateral aspect of the chest. Posterior axillary line (L, R): vertical line drawn through the posterior axillary fold along the posteriolateral wall of the chest. Midaxillary line (L, R): running downward vertically from the apex of the axillary and between anterior axillary line and posterior axillary line. Scapular line (L, R): vertical line drawn through the inferior angle as the arm hanging naturely, parallels to the spine. Posterior midline (L, R): namely midspinal line, running vertically downward through the posterior spinal process, or along the middle of spine. III Natural fossa and anatomic region Axillary fossa (L, R): the depressed region formed from the inside aspect of the upper arm connecting to the chest wall. Suprasternal fossa: a depressed region above the manubrium sterni, behind it lies the trachea in normal condition. Supraclavicular fossa (L, R): the depressed region above the clavicula, corresponds to the upper part of each lung apex. Infraclavicular fossa (L, R): a depressed region beneath the claviculae with its lower margin at the third rib, corresponds to the lower part of each lung apex. Suprascapular region (L, R): the region above the scapular hillock with the upper lateral margin at the ridge of the trapezius, corresponds to the lower part of the lung apex. Infrascapular region (L, R): the region that between the line through two inferior angles and the horizontal line through the twelfth thoracic vertebra. The posteriormidline departs it into two parts. Interscapular region (L, R): The region between the inside ridges of both scapulae, is departed by the posteriormidline into two parts.` IV The boundary of lung and pleura Trachea runs down along the anterior part of the neck into the thorax at the front of esophagus, bifurcates into the left and the right primary bronchus at the sternal angle level, then enters into the left and right lungs, respectively. The right primary bronchus is wider, shorter and steeper, while the left one is slender and oblique. Right primary bronchus departs into three branches, enter the upper, middle, and lower lobe of the right lung, respectively. Left primary bronchus bifurcates and enters the upper and lower lobes, respectively. Two lungs resemble in shape, except for that the anterior part of the left lung is occupied by the heart. Each lobe has a topographic position on chest wall. To know the topographic position is of importance for location diagnosis of lung diseases. Lung apex: protrudes about 3 cm above the upper edge of the clavicula with its apex point near the sternal end of the clavicula, approaches the level of the first thoracic vertibra. Upper boundary of the lung: its projection on the anterior chest wall forms an upward arc. It begins at sternal-clavicular junction, runs upward and outward to the level of the first thoracic vertebra, then downward and outwardly, ends at the border point of middle and inner one third of the clavicula. Outer boundary of the lung: runs downward from the upper boundary, quite approaches the inner surface of lateral chest wall. Inner boundary of the lung: runs down from the sternal-clavicuar junction, the two sides nearly meet each other at the sternal angle, then runs down along each side of the anterior midline, then separates at the fourth costal cartilage level. The right boundary continues almost vertically downward, turns rightward at the sixth costal cartilage, runs down to meet the lower boundary. The left boundary turns leftward to the anterior end of the fourth rib, along the anterior ends of 4-6 ribs downward, then turns left again to meet the lower boundary. Lower boundary: two sides of the lower boundary are in analogy position. The anterior part begins from the sixth rib, runs downward and laterally to the midclavicuar line at the level of the sixth interspace, and to the midaxillary line at the level of the eighth interspace. The posterior part of the lower boundary approaches horizontal at the tenth rib level by the inferior angle line. Boundaries between lobes: called fissure. Lobes of the two lungs are separated by visceral pleura between lobes. The fissure between the upper lobe and the middle and lower lobes of the right lung, and that between the upper and lower lobe of the left lung, is called oblique or diagonal fissure. Both begin from the third thoracic vertebra at posterior midline, run outward and downward, meet the fourth rib at posterioraxillary line, then run downward anteriorly, end at the sixth chondrocostal junction. The anterior upper aspect of the right lower lobe attaches to the lower aspect of the middle lobe. The boundary between the upper and middle lobe is horizontal, called horizontal fissure, begins from the forth rib at posterior axillary line, ends at the right edge of sternum at the level of the third interspace. Pleura: the pleura covering the surface of the lung is termed visceral pleura, and that covering the inner surface of the chest wall, the diaphragm, and the mediastinum, is called parietal pleura. The visceral part and the parietal part of pleura turn over each other successively, make up the right and the left thoracic cavity two wholly closed spaces. Intrathoracic pressure is negative, which makes the two layer of pleura adhere closely together, forming a latent cavity. In the cavity there is a little plasma, which lessons the rub between pleura during respiration. At each side, the costal part and the diaphragmatic part of the parietal pleura beneath the lower boundary of lung turns over and compose a place about 2-3 interspace height, called sinus phrenicocostalis. Because of its lowest position, even at deep inspiration, it can't be brimmed by the expanded lung. B. Chest wall, chest framwork, and breast I Chest wall In examining chest wall, the examiner should pay attention to the following aspects in addition to the nutrition, skin, lymph nodes, and the development of skeleton muscle: 1. Vein: Normally the vein on chest wall is not obvious. When superior or inferior vena cava and their branches are blocked, collateral circulation will be built up, veins on chest wall become full form varicose. The blood flow in the varicose vein is downward when superior vein is obstructed, and upward when inferior vein obstructed. 2. Subcutaneous emphysema: Indicates the condition when air enters and stores in subcutaneous tissue. Pressing the skin with fingers will lead to motion of stored air in the subcutaneous tissues, and produce crepitation, a sensation like rolling a lock of hair between the thumb and fingers or grasping snow. When pressing the stethoscope on the involved skin, the sound can be heard that resemble to rolling hair, called crepitus. Subcutaneous emphysema at chest is commonly the result of injuries of lung, trachea or pleura, free air escapes from injured part into subcutaneous tissues. Occasionally subcutaneous emphysema can be caused by local infection of bacillus aerogenes. In severe cases air may spread to neck, abdomen and other position of subcutaneous tissues. 3.Tenderness: Normally there is no tenderness on chest wall. In intercostal neuritis, costal cartilagitis, chest wall soft tissue inflammation and rib fractures, the involved portion may be tender. Tenderness and pain on percussion on sternum usually exist in leukemia patients when myelodysplasia occurs. 4.Interspace: It must be mentioned whether there is any retraction or bulging of interspace. Retraction of the interspace during inspiration indicates the obstruction of free air flowing into the respiratory tract. Bulging of interspaces may be seen in patients with massive pleural effusion, tension pneumothorax, or severe emphysema. In addition, the corresponding interspace bulging may be noted in the thoracic wall as the result of tumor, aortic aneurysm, or marked cardiac enlargement in infancy and childhood. II Chest framwork In normal subjects, there is some variation in size and shape of the thorax. In general, the two halves of the thorax are grossly symmetric, present elliptical shape. Shoulders are at nearly horizontal level. The clavicula is a little prominent and there is a little depression of both the supraclavicular and infraclavicular areas. Though, in right-handed person, the greater pectoral muscle at the right side is usually more developed than that of the left side. The opposite would apply for those who are left-handed. In adult, the anterioposterior(AP) diameter of the thorax is shorter than the transverse diameter, present a ratio of 1:1.5. In elder and childhood, the AP diameter is a little shorter than or nearly equals to the transverse diameter, makes the thorax cylindric. 1. Flat chest: The thorax framework is flat, the AP diameter is less than half of the transverse diameter. This can be seen in slender adult, and in patients with chronic hectic diseases as well, such as tuberculosis. 2. Barrel chest: The AP diameter is increased to as large as, or even greater than the transverse diameter, resulting in cylindric thorax. The oblique degree of the rib becomes small, the rib angle with spine is larger than 45°. Interspace becomes wider and full. The infrasternal angle becomes wider with less respiratory variation. This situation can be seen in severe emphysema patient, or elderly or obese subject. 3. Rachitic chest: a deformed chest caused by rachitis, seen mostly in childhood. Along each side of the sternum, chondrocostal junctions usually bulge like rosary, termed rachitic rosary. The lower anterior part of ribs turns outward, the part of chest wall attaching with diaphragm depress, form a sulciform band, called Harrison groove. The xiphoid process is depressed, making the thorax funnel-like, called funnel chest. If the AP diameter is a little longer than the transverse diameter, the vertical span is smaller, the lower part of the sternum bulges, and the adjacent ribs depress, the resultant deformed chest is called pigeon chest. 4. Unilateral deformation of the thorax: Bulging of hemithorax is noted most in massive effusion, pneumothorax, or unilateral severe compensatory emphysema. Unilateral flat or retraction of the thorax is usually seen in atelectasis, pulmonary fibrosis, extensive thickening fibrotic pleura, etc. 5. Local bulge of chest wall: Seen in obvious heart enlargement, massive pericardial effusion, aortic aneurysm and tumors inside or on the chest wall. Besides, bulging can also be noted in costal cartilagitis and rib fracture, the former usually has tenderness on the bulged cartilage, the latter often reveals severe pain as the chest wall being pressed, in addition to bone fremitus of the broken ends of ribs. 6. Thoracic deformation caused by deformed spine: Severe kyphoscoliosis, kyphosis, or protrusion of spine, can lead to asymmetric thorax, with widened or narrowed interspaces. The relation between the landmark and the position of underling organ changes. In severe cases of spine deformation, the deformed thorax may cause respiratory and circulatory dysfunction. This is common in spinal tuberculosis. III Breast Normally the breast is not obvious in childhood and man, with the nipple located in the fourth interspace at midclavicular line. In normal female the breast begins to develop during adolescence, assumes hemispherical. The nipple also develops to cylidric shape. Breast examination should be conducted in systemic sequence rather than only the position complained by patient, lest any misdiagnosis. Besides breast, the lymphatic drainage sites must be examined as well. When examined, the patient should stripped to waist for adequate exposure of the chest, and plenty of light is essential. The patient is usually in sitting or supine position. Normally the first step is inspection, then palpation. 1.Inspection 1) Symmetry: two breasts are generally symmetrical in healthy female in erect sitting position. Mild asymmetry can also be seen as the result of difference in development of two breasts. Obvious enlargement of one breast may denote congenital deformation, cyst formation, inflammation, or tumor. Shrinkage of one breast usually indicates maldevelopment. 2) Superficial appearance: Skin erythema of the breast may indicate local inflammation, or breast cancer involving the superficial lymphatic tube and causing carcinous lymphadenitis. The former is commonly associated with local swelling, hotness, and pain, whereas the latter presents scarlet skin without pain, this provides a differentiation. When breast tumor is present, the superficial vessels are usually visible. Moreover, ulceration, pigmentation and scars on the breast skin should be mentioned. Edema of the breast makes the hair follicles and follicular openings easily seen, which may be obvious in breast carcinoma and inflammation. The edema associated with carcinoma is caused by mechanical blockage of cancer cells in the lymphatic channels beneath the skin, termed lymphoedema. In this situation, the hair follicles and follicular opening depress obviously, so that theinvolved skin looks like “ orange peel” or “ pig skin”. Inflammatory edema is caused by inflammatory irritation, which increases the capillary permeability, results in the extravation of plasma into the intercellular space, usually associated with skin redness. Notations should be given as to the exact location and range of the edema on the breast skin. During pregnancy and lactation period, the breast will enlarge obviously, protrude and prollapse, with larger areola and more pigmental. The axillae becomes full, superficial vein in breast skin can also be seen. In some instances the breast tissue extends to the apex of the axillae, because of the hypertrophy of the breast tissue in preparation for lactation. 3) Nipple: The size, location, symmetry of two sides and whether or not inversion of the nipple must be noted. Nipple retraction since childhood indicates mal-development; if it appears recently, it may implies malignancy. Secretion appearing at the nipple indicates abnormality along ductal system. The secretion may be serous, purple, yellowish, greenish or sanguineous. Bleeding is most often caused by the presence of benign infraductal papilloma, but also by the presence of breast carcinoma. Clear nipple secretion becomes purple, green, or yellow, usually indicates chronic cystic mastitis. During pregnancy the nipples become larger and more mobile. In condition with hypoadrenocorticism, there may be obvious pigmentation on areola. 4) Skin retraction: Breast skin retraction may be due to trauma or inflammation which cause local fat necrosis and fibroblastic proliferation, leading to shortening of the ligamentous fibers between the superficial layer and the deep layer in the involved area. It should be mentioned that if there isn't any definite evidence of acute breast inflammation, skin retraction often indicates the presence of a malignant tumor. Especially when advanced appearance of carcinoma such as tumor mass, skin fixation or ulceration does not appear, the mild degree of skin retraction may be the physical sign of early stage of breast carcinoma. In order to find skin or nipple retraction, the patient should be instructed to do such upper limb movements that cause the contraction of anterior chest muscles to stretch the breast ligament, such as raising arms over head, pressing palms together, or exerting pressure on both hips with her hands. 5) Axilla fossa and supraclavicular fossa: Thorough inspection of the breasts includes observation of the most important lymphatic drainage areas. Detailed observation of the axillary and supraclavicular regions must be conducted to find if there are any bulging, redness, mass, ulceration, fistula or scars. 2. Palpation: The upper margin of the breast is at the second or the third rib, its lower margin at the sixth or seventh rib, the inner margin at the sternal ridge, and the outer margin ends at anterioaxillary line. When the breast is palpated, the patient may take sitting position, with her arms at side first, then overhead or pressed on both hips. In supine position, the shoulders can be elevated by a small pillow putted under them to allow the breasts rest more symmetrically on the chest wall for more detailed and convenient examination. Take the nipple as the central point, a horizontal line and a vertical line through the central point departs the breast into four quadrants. This makes it convenient to locate the lesion. The palpation should begin from the healthy breast, then the ill one. The examiner should place his palm and fingers flatly on the breast, press gently with the palmar aspect of fingertips, with a rotary or to-and-fro motion. The left breast should be palpated from the upper lateral quadrant, with a procedure of clockwise direction for thorough examination, each quadrant is palpated superficially and then deeply, and the nipple is palpated finally. The same procedure is adopted for palpation of the right breast with anti-clockwise direction. Attention must be paid to any redness, swell, hotness, tenderness and lump while palpation being performed, as well as induration, mis-elasticity and secretion. The normal breast is felt like vague granular and pliable. The amount of subcutaneous fatty tissue will affect the “feel” of the breast. The breast of younger woman is softer and more homogeneous, whereas in older woman it will be more stringy and nodular. The breast is made up of lobules of glandular tissue, which should not be misconstrued as tumor mass when palpated. During menses the breast becomes tight with congestion and the loose with decongestion thereafter. During pregnancy the breast becomes larger and more pliable, whereas during lactation period it is more nodular. Upon palpation of the breast the following physical qualities should be noted: 1) Consistency and elasticity: Increase in firmness and lost of elasticity suggests infiltration of the subcutaneous tissue by the presence of an inflammation or neoplasm. In addition, the consistency and elasticity of the nipple must be noted. When subareolar carcinoma exist, the elasticity of the skin of involved region is usually lost 2) Tenderness: The presence of tenderness in a position of the breast usually indicates an underling inflammatory process. The breast is prone to be sensitive during menstruation, however, tenderness is seldom in present with malignant lesions. 3) Mass: If a mass exist, it should be characterized as the following features: ① Location: The exact location of the mass must be designated. General method is to take the nipple as the central point, describe the mass according to the clock numbers and axis. Furthermore, the distance of the mass from the nipple must be recorded for the sake of accurate location of the mass. ② Size: The mass must be described in length, width and thickness, for the comparison in the future to determine if it progresses or regresses. ③ Contour: pay attention to whether the mass is regular or irregular, the margin is dull or acute, and whether it adheres to surronding tissue or not. Most benign tumors have a smooth, regular contour, whereas most malignant masses are convavoconvex, with firmed margin. However, it must be mentioned that inflammatory lesions may also have an irregular contour. ④ Consistency: The hardness must be described clearly. It may be described generally as soft, cystic, moderately firm or extremely hard. A benign tumor is usually felt soft, cystic; while a firm consistency mass with irregular contour usually denotes a malignant lesion. However, a hard region may also be caused by inflammation. ⑤ Tenderness: It should be ascertained whether or not the lesion is tender, and, if so, to what degree. An inflammatory process is usually moderately or markedly tender, whereas most malignant lesions are not obviously tender. ⑥ Mobility: The examiner should determine whether the lesion is freely movable. If it is movable in certain directions, or fixed, he must determine wether the mass is fixed to the skin, to the deep structures, or to the surrounding breast tissue. Most benign lesions have a large mobility, inflammatory lesion is considerably fixed, and a malignant lesion in early stage is movable, however, as the process developes, it becomes fixed because other structures are invaded. After palpation of the breast, the axilla, supraclavicular region and neck should be palpated carefully, to detect any enlargement of lympho nodes or other abnormalities, because these areas are usually involved in inflammatory lesion or invaded by inalignancy. 3. Common breast lesions: 1) Acute mastitis: The breast is red, swollen, hot and painful, inflammation is usually restricted in one quadrant of one breast. Induration or mass is palpable, associated with general toxic symptoms such as shiver, fever, and sweat. This disease occurs commonly in lactation women, sometimes also in young women and men. 2) Breast tumors: One must differentiate benign from malignancy. Breast carcinoma is lack of inflammatory appearance, most are solidate and adherent to subcutaneous tissue, the local skin appear as orange peel, the nipple is usually retracted. It is most seen in female of middleaged or older, usually associated with axillary lymphatic metastasis. Benign lesions are soft, clear of margin, and somehow movable, usually seen as cystic mastoplastia, intracanalicular fibroma, etc. Gynecomastia in male usually occurs with endocrine disorders, such as estrogen intak, hyperadrenocorticism, and liver cirrhosis, etc. C. Lung and pleura When chest is examined, the patient is generally in sitting or supine position with upper garment stripped off for adequate exposure of the chest. The room should be comfortably warm, because shivering of the muscle caused by cold may lead to unsatisfactory inspection, or make auscultation misunderstood. Good lightening is quite important. When the patient is supine for the examination of the anterior thorax, the light should be above and directly in front of the anterior thorax, above and behind when the posterior thorax being examined. The lateral walls can be examined with the same light, if the examiner rotates the patient from front to back. The examination of lung and pleura routinely includes inspection, palpation, percussion, and auscultation. I Inspection 1. Breath movement: The breath movement in healthy subject at rest is steady and regular. This is controlled by the breath center and regulated by the nerve reflex. Some serum factors, such as hypercapnia, may directly inhibit the breath center and make the breath shallow. Hypoxemia can stimulate the carotid sinus and the aortic body chemo-receptor, thus quicken the respiration. In condition of metabolic acidosis, the blood PH drops, and respiration become deeper and slower to remove CO2 out of the lungcompensately. In addition, pulmonary stretch reflex can also change the rhythm of respiration, seen in conditions like pneumonia or pulmonary congestion caused by heart failure, thus breath becomes superficial and quick. Furthermore, the breath rhythm can also be controlled by consciousness. The respiratory movement is accomplished through the contraction and relaxation of the diaphragm and intercostal muscles. The thorax expands and relaxex with the respiratory movement to bring about the expansion and collapse of the lung. In normal condition, inspiration is an active movement, leading to the expansion of the thorax, increasing the intrathoracic negative pressure and expansion of the lung, resulting in the air flowing into the lung from the upper respiratory tract. The average tidal volume in adult with quiet breath at rest is about 500 ml. Expiration is a passive movement depending on the elastical recoil of the lung and chest, accompanied by the decretion of negative intrapleural pressure, then the air in the lung is exhaled accordingly. Therefore, inspiration and expiration are closely related to the negative intrapleural pressure, the air flow into and out of the lungs, and the changes of intrathoracic pressure. During inspiration, the anterior parts of the ribs move outward and upward, while the contraction of diaphragm leading to bulging of the abdomen, whereas during expiration, the anterior parts of ribs move inward and downward, while the relaxation of the diaphragm leading to retraction of the abdomen. Respiration in healthy males and children tends to be predominantly diaphragmatic, the lower part of thorax and the upper abdomen move up and down substantially, and form abdominal respiration. Whereas in female, the respiration is mainly dependent on intercostal muscles, this is thoracic respiration. Actually, both forms of respiration exist simultaneously with different degrees. Some diseases can change respiratory patterns. Pulmonary or pleural diseases such as pneumonia, severe tuberculosis and pleurisy, or chest wall diseases such as intercostal neuralgia, rib fracture, can all weaken the thoracic respiration and strengthen the abdominal respiration. Peritonitis, massive peritonal effusion, extreme enlargement of the liver or spleen, tremendous intraperitonal tumor and advanced pregnancy, can all limit the downward movement of the diaphragm, resulting in weakened abdominal respiration and compensatory strengthened thoracic respiration. In patients with partial obstruction of the upper breathing tract, air flow into the lung is impedent, thus the inspiratory muscle contraction may lead to extremely high negative intrathoracic pressure and cause the depression of supersternal fossa, superclavical fossa and interspaces, termed “ three depression sign”. On such occasions inspiration is prolonged, hence called inspiratory dyspnea. It usually occurs when trachea is obstructed, by foreign body, for example. On the contrary, in patients with lower respiratory tract is obstructed, because the airflow out of the lung is impedent, exhalation with exertion may lead to bulging of the interspaces. This is associated with prolonged expiration, called expiratory dyspnea, it usually occurs in asthma and obstructive emphysema. Litten Phenomenon: Also named as wavy diaphragmatic shadow, a phenomenon of diaphragm movementdemonstrated by the oblique projection of light. When the phenomenon is detected, the light should be placed at head or foot side, the examiner is in front of or at the side of the light with his vision line at the upper abdomen level. During inspiration, a narrow shadow begins from the anterioaxillary line in the seventh interspace and shifts to the tenth interspace, whereas during expiration, the shadow regresses upward to the original position. This phenomenon is due to the diaphragmatic movement corresponding to respiration. The normal shift range of the diaphragm is 6cm, which has the same clinic significance as the lower margin of lung. 1. Respiratory rate: In the normal adult at rest, the respiratory rate is 16 to 18 per minute. The ratio of respiratory rate to pulse rate is 1:4. The respiratory rate in newborn is about 44 per minute, and decreases gradually upon growing up. 1) tachypnea: Indicates the increased respiratory rate that over 24 per minute, usually seen in fever, pain, anemia, hyperthyroidism and heart failure. Usually the respiratory rate increases approximately four additional cycles per minute for each 1°above the normal temperature. 2) bradypnea: Indicates the decreased respiratory rate that less than 12 per minute. The respiration becomes superficial, seen in over dose of anesthetics or sedatives and elevated intracranial pressure. 3) Change of the breath depths: Hypopnea (fig.3-5-8),could be seen in respiratory palsy, ascites and fatness, etc. And also could be seen in pneumonia, pleurisy, pleural effusion and pneumothorax. Hyperpnea (fig.3-5-8), could be found during strenuous exercises, for increased body oxygen supply needs more air exchange through the lung. It can also appear when one is excited or nervous, because of over ventilation. Decreased PaCO2 ensues and could induce respiratory alkalosis. Patients often feel numbness around the mouth and at the tips of the limbs. Tetany and apuea may happen in severe cases. Deep and slow breath could appear during serious metabolic acidosis. This is because the HCO3 in the extracellular fluid is not enough, and PH is lower, for compensation, CO2 is eliminated by the lung to maintain the acid-base balance. This kind of deep and slow breath is also named as Kussmaul breath, seen in diabetic ketoacidosis and uremic acidosis. (3) Rhythm of the breath Normal adult respiration is basically regular and smooth in testing status. The rhythm of the breath usually changes in diseases. 1. Tidal breathing Also called as cheyne-stokes respiration. Respiration waxes and wanes cyclically so that periods of deep breathing alternate with periods of apnea(no breathing). The periods of the tidal breath can last from 30s to 2min. The periods of apnea can persist 5-30s. So only through carefully and long enough observation, the whole process could be realized. 2. Ataxic breathing Also called Biot’s breahting. Ataxic breathing is characterized by unpredictable irregularity. Breaths may be shallow or deep, and stop for short periods (fig. 3-5-0). The mechanism of the upper two rhythm is that the respiratory central excitability is depressed, the feedback system of the breath can’t work normally. The respiratory center can only be excited when anoxia is severe, and CO2 concentration in the blood reaches a certain degree; when the CO2 is exhaled, the center lost the effective excitability again, the breath weakened and suspended. Causes include heart failure, uremia, drug induced respiratory depression and brain damage(typically on both sides of the cerebral hemispheres or diencephalon). Ataxic breathing is more severe than the tidal breathing, the prognosis is worse, often happening before demise. Aging people normally may show tidal breathing in sleep, this is a sign of cerebrovascular sclerosis. 3.Inhibitory breath The inspiration is suspended while a severe pain in the chest happened, the respiratory movement restrained suddenly and momently. The expression of the patient is suffering, breath become shallow and frequent. Causes include acute pleurisy, tumor, costal fracture and severe trauma of the thorax. 4. sighing respiration Breathing punctuated by frequent sighs should alert you to the possibility of hyperventilation syndrome – a common cause of dyspnea and dizziness. Occasional sighs are normal. 2. PALPATION (1) Thoracic expansion It is the movement range of the thorax during respiration. Easy to obtain when examine the antero-inferior part of the thorax, where the respiratory movement is much obvious. Place your thumbs along each costal margin, and your hands along the lateral rib cage. When the patient inhales deeply, watch the divergence of your thumbs as the thorax expands, and feel the range and symmetry of respiratory movement. Causes of unilateral diminution of or delay in chest expansion include huge pleural effusion, pneumothorax, pleural thickening and atelectasis etc(fig. 3-5-10). (2) Vocal fremitus Also called tactile fremitus. Vocal fremitus refers to the palpable vibrations transmitted through the bronchopulmonary system to the chest wall when the patient speaks. Ask the patient to repeat the words “yi—“. If fremitus is faint, ask the patient to speak more loudly or in a lower voice. Palpate and compare symmetrical areas of the lungs using either the ball of your hand (the bony part of the palm at the base of the fingers) or the ulnar surface of your hand. In either case you are using the vibratory sensitivity of the bones in your hand to detect fremitus. Identify, describe, and localize any area of increased or decreased fremitus. Fremitus is typically more prominent in the interscapular area than in the lower lung fields, and is often more prominent on right side than on the left. It disappears below the diaphragm. Fremitus is decreased or absent when the voice is soft or when the transmission of vibrations from the larynx to the surface of the chest is impeded. Causes include an obstructed bronchus, chronic obstructive pulmonary disease, separation of the pleural surfaces by fluid (pleural effusion), fibrosis ( pleural thickening), air (pneumothorax) or an infiltrating tumor; and also a very thick chest wall. Fremitus is increased when transmission of sound is increased, as through the consolidated lung of lobar pneumonia. (2) pleural friction fremitus During acute pleurisy, the fibrin deposit between the two layers of the pleura, the visceral pleura and the parietal pleura rub with each other, this can be felt by the examiner’s hand, so it is called pleural friction fremitus. It can be palpated both in inspiration and expiration. It is most obvious at the lower part of the thorax for the movement range here is the greatest. When the air passing through the narrow trachea and bronchus or through thick exudate in the airway, a kind of fremitus could also be produced. Differentiated, usually the former could disappear after coughing while the latter will not. 3 PERCUSSION (1) The method of percussion 1) Mediate percussion Hyperextend the middle finger of your left hand(the pleximeter finger). Press its distal interphalangeal joint firmly o the surface to be percussed.Avoid contact by any other part of the hand, because this would damp the vibrations. Put your right forearm quite close to the surface with the hand cocked upward. The right middle finger should be partically flexed, relaxed, and poised to strike. With a quick, sharp, but relaxed wrist motion, strike the pleximeter finger with the right middle finger (the plexor). Aim at your distal interphalangeal joint. Use the tip of your plexor finger, not the finger pad. Your striking finger should be almost at right angles to the pleximeter. Withdraw your striking finger quickly to avoid damping the vibrations that you have created. Use the lightest percussion that will produce a clear note. A thick chest wall requires heavier percussion than a thin one. In comparing two areas, however, keep your technique constant. Thump about twice in one location and then move on. You will perceive the sounds better by comparing one area with another than by repetitive thumping in one place(fig.3-1-2). 2) Immediate percussion Percuss the thorax by the tip of your plexor finger or the united finger pad directly to show the changes of different places. When percussed the patient should be in a sitting or dorsal position, relaxed, and breathing homogeneously. First, examine the anterior chest, percuss each intercostal space one by one from supraclavicular fossa. Second, the lateral chest wall, ask the patient raise the arms and put them on the head, percuss from the axilla down to the costal margin. And last percuss the posterior chest. Ask the patient lower the head slightly, keep both arms crossed in front of the chest, shift their scapulae lateralwards as obviously as possible. The upper body leans slightly anteriolly, percuss from apices to the lung bases, after the width of apics be decided, then percuss each intercostal space from up to sown, until the movement range of the diaphragm be identified. (2) Influencing factors Dullness replaces resonance when fluid or solid tissue replaces air-containing lung or occupies the pleural space beneath your percussing fingers. Examples include: lobar pneumonia, in which the alveoli are filled with fluid and blood cells; and pleural accumulation of serous fluid (pleural effusion), blood (hemothorax), pus (empyema), fibrous tissue, or tumor. Generalized hyperresonance may be heard over the hyperinflated lungs of emphysema or asthma, but it is not a reliable sign. Unilateral hyperresonance suggests a large pneumothorax or possibly a large air-filled bulla in the lung. (3) Classification of the percussion notes 1) Resonance It is the normal sound of the lung, not very loud but could be heard easily , and have a long duration, shown as a low pitched sound. 2) Hyperresonance Lower and longer than the resonance, very loud and very easy to be heard. 3) Tympany The pitch is higher than resonance, the duration is moderate, intensity is moderately loud, e.g. percussion on a stomach filled with gas produces such a sound. 4) Dullness Opposite to resonance, duration is not so long, pitch and intensity are both of medium degree, senses of vibration beneath the pleximeter finger is not so obvious, but sense of resistance is increased. 5) Flatness It refers to the lacking of resonance, bery similar to the sound of knocking a water-filled container. It is also considered as the extreme dullness. It is high and soft in quality. Duration is short. (4) Normal percussion notes 1) Normal percussion notes of the lung: resonance is the normal notes of the lung. It is influenced by the air containing, the thickness of the chest wall, and the organs around. Influenced by muscle and skeleton, the sound is duller in the upper part of the anterior thorax than the lower part; duller in the upper part of the right thorax than of the left side; duller in the posterior chest than the anterior chest. And the sound of right infra-axilla is duller for the liver is near, though in the left side at the comparable part, the percussion soud is tympany for the gastic air bubble over there, this part is also called Tranbe tympany region. 2. Percussion of the pulmonary boundary (1) Upper pulmonary boundary, that is the width of the apics, posterior part of the cervical muscle is its inner side and shoulder girdle is at its lateral side. The method is: percuss from the middle trapezius muscle outwards to lateral side little by little, when the sound turns from resonance to dullness gradually, the lateral termination of the upper border is identified. And then, percuss from the same middle part to inner-side, when the resonance turn to dullness again, the inner termination of the border comes out. The width of this resonant boundary is the width of apics, 5-8cm regularly, it is also named as Kronig isthmus. The width of right side is narrower than left, for right apics is located lower and the muscle of right shoulder girdle is stronger. The boundary is narrowed or sounds dull when tuberculosis infiltrates the apics and fibrosis or atrophy is formed. The upper boundary widened or changed to hyperresonance when there is emphysema. (2) The anterior pulmonary boundary The heart normally produces an area of dullness to the left of sternum. The right anterior pulmonary boundary is at the sternal line, and the left one is at the parasternal line from 4th to 6th interspace. It is influenced by the size of heart, pericardial effusion, aortic aneurysm, enlarged lymph nodes of the pulmonary portal and also by the emphysema. (3) The inferior pulmonary boundary It is about the same of two sides, located at the 6th intercostal space at the midclavicular line, 8th interspace at the midaxillary line, 10th interspace at the scapular line. It is different in different body type. In fat person, the boundary could be elevated about one intercostal space and in thin person descended about one interspace. Pathologically, the boundary descends with emphysema, celiac organ declined. It elevates with a atelectasis, celiac hypertension. 3.movement range of the lower pulmonary boundary That is equal to diaphragmatic movement. Method is: identify the level of diaphragmatic dullness during quiet respiration. With the pleximeter finger held parallel to the expected border of dullness. Percuss in progressive step downward until dullness clearly replaces resonance. Diaphragmatic excursion may be estimated by nothing the distance between the levels of dullness on full expiration and on full inspiration, normally around 6-8cm. An abnormally high level suggests pleural effusion or a high diaphragm, as from atelectasis or diaphragmatic paralysis. 4.Percussion of thorax in a lateral decubitus. Influenced by the bed, we can percuss out a comparative dull zone alone the near –bed-side thorax. The diaphragm elevated caused by the celiac pressure. An the near-bed-side intercostal space, we can percuss out a comparative dullness region at the tip of the subscapular angle on the upper side, when pillow is removed, the spine stretched, this dull region then disappeared. Change the position, examine again to prove the influence of the posture(fig 3-5-13) 5. Abnormal percussion sound of the thorax The percussion sound can be changed at least the focus is larger than 3cm and the distance between the surface less than 5cm. The note will be dullness or flatness when air contain decreased, such as pneumonia, atelectasis, pulmonary infarction, pulnomary edema, tumor, pleural effusion, pleura thickening etc. The note will be hyperresonance when the pulmonary tension decreased and air contain increased. Such as emphysema. If the diameter of the cavity lesion is larger than 3-4cm, and close to the chest wall, such as cavernous lung tuberculosis, liquefacient pulmonary abscess and cysts, the note will be tympany. If cavity is very large and located shallow, or patient with hypertonic pneumothorax, the percussion note will be tympany locally. For its metalloid reecho, the note is also called Amphorophony. When pulmonary air contain decreased, such as atelectasis, congestion and dissolution stage of pneumonia, pulmonary edema, the local percussion note can be a mixed sound which has the character of both dullness and tympany, we name it as dulltympany Dullness replaces resonance when fluid or solid tissue replaces air-containing lung or occupies the pleural space beneath your percussing fingers. Examples include: pleural effusion. If the effusion is moderate, without pleural thickening or adhesion, patient in a sitting position, there will have a Damoiseau curve formed by the effusion, Show as figure 3-5-14. Also show as the same figure, there are Garland and Grocco triangle region of dulltympany formed by the effusion, spine, and pulmonary lower boundary. The size of this region is influenced by the quantity of effusion. 4. AUSCULATION Listen to the breath sounds with the diaphragm of a stethoscope as the patient breathes somewhat more deeply than normal through an open mouth. Using locations similar to those recommended for percussion and moving from one side to the other, compare symmetrical areas of the lungs. Listen to at least on full breath in each location. If the breath sounds seem faint, ask the patient to breathe more deeply. You may then hear them easily. (1) Normal breath sounds 1) vesicular breath sound It is soft and low pitched. They are heard through inspiration, continue without pause into expiration, and then fade away about one third of the way through expiraton(fig.3-5-15). The strength of the sound is associated with sex, age, respiratory deepth, pulmonary elasticity, and the thickness of the chest wall. 2). Bronchial breath sound: is the sound of turmoil flow produced by the inspirated air through glottis, trachea or major bronchi, similar to the sound of “ha” when one lift tongue to make the expiration through mouth. Its pitch is high, inspiration is shorter than expiration because inspiration is of active movement, the glottis widens, inflow is rapid, while expiration is of passive movement, the glottis gets narrower, and out flow is slow. Besides, the expiration is more exaggerated and higher pitched, there is a very slow silent pause between inspiration and expiration(Fig.3-5-15). In normal persons, bronchial breath sound could be heard over the laryngus suprasternal, notch the areas near the 6th and 7th cervical vertibra, and around the 1st and 2nd thoracic vertebra. The louder and the lower pitched is the sound, the nearer to the trachea one listca to. 3. Bronchovescicular breath sound: is a mixed sound composed of bronchial breath sound and vescicular breath sound, higher pitched and louder. While its expiratory component is similar to bronchial breath sound, with lower loudness and pitch, and sith less tubular characteristc and shorter expiratory phase, there is a very short gap between inspiratory and expiratory phase, durations of two phases are almost the same(Fig.3-5-15). Bronchovescicular breath sound could be heard in the 1st and 2nd intercostal space near the sternum, around the intrascapular region at the 3rd and 4th thoracic vertebrae, and around the lung apex. If such a sound is heard at other location than those mentioned above, it is usually abnormal, a disorder should be suspected of. (2) Abnormal breath sounds 1. abnormal vesicular breath sound 1) Decreased or absent vesicular breath sound: This is associated with decreased or slower air flowing ito the vesicls and also with impaired conduction of breath sound. This sign on the lung could appear localized, unilateral or bilateral, the causes may be the followings: a).restricted movement of the thorax due to chest pain, ossification of rib cartilages and resection of ribs etc. b) respiratory muscle diseases, such as myasthenia, grakis, diaphrmatic paralysis and diaphramatic muscular spasm etc. c) bronchial obstruction, like chronic bronchitis, bronchial stricture etc. d) oppressive under-expansion of the lungs, such as pleural effusion, or pneumothorax etc. e) abdominal disorders, like massive ascitis, huge tumor in the abdomen etc. 2) Increased alveolar breath sound: Alveolar breath sound accentuated on both sides is associated with exaggerated respiratory movement and vetilation, on such occasion, there is more and faster air flow into the lunge. The causes are as follows: a) body oxygen demand increases and makes respiration deep, long and faster, eg. Exercise, fever and high metabolism rate etc; b) anoxia stimulattes respiratory center, makes respiration accentuated, eg, anemia c) blood acidity increases. Stimulates respiratory enter, eg, acidosis; unilateral accentuated alveolar breath sound could been seen in patients with unilateral thoracic pulmonary diseases; then there is diminished alveolar breath sound on the involved side, and compensatory accentuated breath sound on the normal side. 3) Elongated expiratory breath sound. Occurs because of partial obstruction, spasm or stricture of the lower respiratory tract, happening in bronchitis, bronchial asthma etc. Leading go elevated expiratory impedence, or because of lowering elasticity of pulmonary tissue, resulting in decreased expiratory power, happening in COPD etc. 4) Interrupted breath sound: Segmental pulmonary inflammation or bronchial structure makes the air enter alveoli unharmoniously and thus results in interrupted breath sound. It is also called cogwheel breath sound because of short irregular pauses, often seen in pulmonary TB and pneumonia. It must be noticed that interrupted adventory sounds due to muscular contractions may be produced when one feels chilly, painful or nervous, but they are not related to respiration, and differentiation is easy. 5) Hoarse breath sound: heard in the early stages of bronchial or lung inflammations, due to smoothlessness or stricture produced by mild bronchial membranous edema or inflammation. 2. Abnormal bronchial breath sound, bronchial breath sound heard at the locations where vesicular breath sound should be heard is abnormal, and is also called tubular breath sound, the reasons are as follows: 1) Consolidation of lung tissue: This makes bronchial breath sound conducted easily through the dense consolidated lung tissue to body surface, its location, area and loudness is related the location size and depth of the lesion, the larger and the shallower the lesion, the louder the sound, and the vice versa. At consolidation stage of lobar pneumonia, bronchial breath sound is often louder and high pitched near the listening ear. 2) Big cavity in the lung, when there is a cavity in the lung surrounded by consolidated lung tissue, communicating with the bronchus. The breath sound harmonicates in the cavity, and conducts well through the consolidated tissur, bronchial breath sound could be heard clearly, often seen in pulmonary abxcess or cavity-formed pulmonary TB. 3) Pressed atelactesia: pleural effusion may press on the lung, make underlying lung tissue more dense and cause atelactesia. Because of better conduction through the consolidated past of the lung, bronchial breath sound could be heard clearly. This condition is often seen in lung abscess and cavitous pulmonary TB. 3. Abnormal bronchoalveolar breath sound: heard over the area where only normal alveolar breath sound is heard. It is produced because consolidated part is smaller and mixed with normally air contained pulmonary tissues or the consolidated part is deep and covered by normal lung tissue, often seen in bronchopneumonia, pulmonary TB early stage of lobar pneumonia or over the underexpanded lung area above pleural effusion. (3) Rales, the adventitious sound, not present in normal situation, not due to the change of breath sound. Several kinds of rales could be discerned according to their characteristics. 1. moist rale: produced due to passage of air through thin secretions in the respiratory tract, such as exudate, sputum, blood, mucus, or pus etc. The sound could also be regasded as crackles produced by reopening of the bronchials at inspiration when bronchiolar wall adheres and closes because of tenacious secretion at expiration. 1) The characteristics of rales: adventious sounds besides breath sound, discrete and short in time, often series of jeveral sounds appear, siginificant in inspiration or in the terminal phase of inspiration, present sometimes in the early phase of expiration, the location is rather fixed, quality not variable, medium and fine rale could be present simultaneously, it may diminish or disappear after cough. 2) Classification of rales: 1.loud or unloud rale according to its louderness (1) loud rale: rales sonorous, heark in pneumonia, lung abscess or cavitous pulmonary TB, produced due to surrounding tissue with better conduction. Consolidation or harmony in the cavity lead to loud rale. If the cavity wall is smooth, sonorous rale may mix with somewhat metalic pitch. (2) unloud rale, the sound is low and for to ear because there is still much normal lung tissur around the lesion, sound becomes gradually lower during conduction.2. Rales could be divided into coarse, medium and fine ones and even crepitations according to the size of respiratory tract lumen the amount of secretion(Fig.3-5-16). (1) coarse rales: also named as large bubble sound, often happening in the early phage of inspiration(Fig 3-5-17), heard over the areas of trachea major bronchi and cavitation, such as bronchiectasis, lung edema, pulmonary TB or lung abscess cavitation. Comatose and death impending patients, are too weak to excrete secretion in the respiratory tract. Coarse rale could be heard over the trachea, even without usage of stethoscope, it is then called death rattle on this occasion.(2) Medium rales: or medium bubble sound, produced in the medium bronchi, at the middle phase of inspiration(Fig 3-5-17), heard in bronchitis, bronchopneumonia etc. (3) fine rale also named small bubble sound, produced in bronchioles, at the late phase of inspiration(Fig3-5-17), met in bronchiolitis, bronchopneumonia pulmonary congestion and pulmonary infarction etc. (4)Crepitus: a very fine and harmonious rale, often occussing at the terminal phase of inspirationlike the sound when one hold a lock of hair near your ear and sub it, they are the result of presence of secretion in the bronchioles and alveoli, haking them adhere one another, when the patient inhales, these bronchiole and alveoli open again and result in high- pitched fine crackling rales with high frequency. They are often met in inflammation of brochioles and alveoli or pulmonary congestion, early phase of pneumonia and alveolitis etc. However in normal old people or patients with prolonged bed rest, crepitus alsocould heard over two lung bases, it disappears after several deep breaths or coughing, with no clinical significance. Localized lung rales only indicate localized lesions of the same plase, like pneumonia, pulmonary TB, or bronchiectasis etc. Rales over two lung bases are often met in pulmonary congestion due to heart failure and bronchopneumonia etc. Rales over the whole two lung fields are often met in acute lung edema and severe bronchopneumonia. 2. Rhonchi: produced because there present stricture or partial obstruction of the trachea, bronchi or bronchioles, air through these passways becomes turbulent, the pathologic basis for which is inflammatory membranous congestion and edema oversecretion, bronchial muscular spasm, obstruction due to tumor and foreign bodies in the bronchial lumen, and stricture due to oppressian of extraluminal enlarged lymph nodes or mediastinal tumors. 1) Characteristics of bronchi: they are continuous, relatively long, and musical adventious breath sound. Rhochi are rather high-pitched with the basic frequency of about 300-500 Hz. Audible both during inspiration and expiration, in general more prominent during expiration. Rhonchi are easily variable in intensity, quality and location, sometimes they change obviously instantly. Some rhonchi, which occur in the large air passages above main bronchi, may be very loud, audible easily even without stethoscope. 3) classification: (1)sibilant rhonchi: high pitched, basic frequency may be over 500 Hz, short like “zhi-zhi” sound, or musical in character. Sibilant rhonchi are often produced in smaller bronchi or bronchioles(Fig3-5-16), and often accentuated by forced expiration.(2) sonorous rhonchi: are low pitched, the basic frequency is about 100-200 Hz, like moaning or snore in character. They often occur in trachea or major bronchi(fig3-5-16). Rhonchi heard on both sides of lungs, are often met in bronchial asthma, chronic bronchitis and cardiogenic asthma etc. Localized rhonchi are often heard in bronchial membranous TB or tumor because of localized bronchial structure. (4) Vocal resonance : is produced in the same fashion as vocal fremitus. It is elicited by having the patient repeatedly say “yi” with ordinary voice loudness, sound vibration at laryngus will conduct through trachea, broncho alveoli and chest wall to the stethoscope. Normally, the word spoken are not as loud and clear as when heard directly, and the syllables are not distinguishable. It is heard loudest near the trachea and major bronchi and is less intense at the lung bases. Vocal resonance is decreased in bronchial obstruction, pleural effusion, pleusal thickening, chest wall edema, obesity and emphysema etc. Vocal resonance changes when there present pathologic conditions, it is classified as follows according to auscultation differences.1. Bronchophony: This indicates vocal resonance that is increased both in intesity and clarity, it is usually associated with increased vocal fremitus, dullness to percussion and abnormal bronchial breathing, and indicates the presence of pulmonary consolidation.2. pectorilogny: a kind of bronchophony that is more intense and clear and near to ear. The syllables may be understood when the patient whispers. Its presence always indicates large area of consolidation. Occasionally, pectriloging may be obvious before bronchial breath sounds develop.3. eqophony: not only there is an increase in intensity of the spoken voice but its character is also altered so that there is a nasal or bleating quality. Ask the patient to say”yi-yi-yi”, if egophony is present, they will sound as “a-a-a”.It is often heard over the upper portion of a moderately pleural effusion or where there is a small amount of fluid in association with pneumonic consolidation.4. “whispered” pectoriloguy, the sounds must actually whispered as :yi yi yi”,In the normal subject the whispered voice is heard only faintly in the areas where bronchovesicular breath sounds are normally heard. Accentuated and higher-pitched pectoriloguy could be clearly heard when there is pneumonic consolidation, thus this sign is of value for the diagnosis of pulmonary consolidation. (5) Pleural friction rub: Normally the visceral and parietal surfaces of the pleura glide quietly during respiration because of the presence of a little amount of fluid in the pleural cavity. However, when these surfaces become inflammed and there is exudated fibrin, the subbing of the roughened surfaces during respiration produces such pleural friction rub. The characteristics of a friction rub can be imitated by pressing the palm of one hand over the ear and then rubbing the back of the hand with the fingers of the other hand. It is often heard during both phases of respiration, relatively superficial, more clearly at the end of inspiration or at the beginning of expiration. Friction rub disappears when breath is held. An increase in intensity of the friction sub may be noted with pressure of the stethoscope over the chest wall. The most common site for a friction rub to be heard is the lower anterolateral chest wall, the area of greatest thoracic mobility. It is seldom heard over the apex because its respiratory excussion is less than the laver portion of the thorax. Friction rub may disappear or reappear with the changes of body position. It also disappear when there presents moderate amount of pleural effusion, and two layers of pleura separate, but reappears when effusion is absorbed and two layers contact again. If mediastinal pleura becomes inflammed, pleural friction rub could be heard both with respiration and heart beat. Pleural friction rub often occus in fibrioous pleusisy, pulmonary infarction, pleural tumor and uremia etc. (6) Coin sign: press a coin on the patients’ one side of middle of front chest, then tap it with another coin. On the comparable part of the back of the ipsilateral thorax, one could hear a tympany with a kind of metal tone, this is the positive coin sign, which could be met in pneumothorax. (7) D The major symptoms and signs of common respiratory diseases (1) Lobar pneumonia Lobar pneumonia refers to lobar distribution of pulmonary inflammation, the main pathogen is streptococcus pneumoniae. Pathologically, three stages could be discovered, they are congestion, consolidation and dissolution. Clinical manifestations are different with different stages, however there are no clear demarcation among three stages. [symptom] the patients usually are adolescent with the occurrence after tiredness, wine drinking, exposing in the coldness. The disease often starts abruptly, with chill and then high fever, the temperature could be up to 39-40°C , as sustained fever, they usually complain of headache, muscular pain, chest pain on the affected side, tachypnea, cough, rusty brown sputum, the temperature may drop drastically several days later, and accompanied by massive sweating, the patient then may feel much better. [signs] The patient appears acute faces, with flushed cheeks, alae nasi fans, dyspnea, cyanosis, rapid pulse, and perioral herpes is also common, signs of congestive stage may be present, including increased vocal fremitus. Crackles are localized to the involved region. When pneumonia involving a whole lobe progresses, signs of consolidation appear, as significantly increased , vocal fremitus and resonance, dullness or flatness to percussion, and bronchial breath sounds, pleural friction rub could be heard if pleura is involved, During resolution stage, all the above signs gradually disappear. (2) chronic bronchitis complicated with emphysema Chronic bronchitis is a non-specific inflammation involving membrane of the brachea and bronchials and the surrounding tissues, It occurs insidiously and progresses slowly, worsens to become chronic obstructive emphysema in the late stage, and even leads to pulmonary hypertension and cor pulmonale. Its etiology is variable, most propably associated with prolonged smoking, repeated respiratory tract infections, long time contact with toxic gas and dust, air pollution, bad weather conditions, allergic tendency, deficiency of local defense mechanism and immune function and unbalance of autonomic nervous system, etc. In the lesion, there are bronchial membranous congestion, edema, oversecretion of the glands, resulting in bronchial spasm, bronchial membranous atrophy, rupture and damage of bronchial smooth muscle, hyperplasia of peribronchial fibrous tissue, and finally bronchiolar and alveolar dilatation. [symptoms] Chronic cough is the main symptom in winter, and often lasting longer than 3 months, the cough is often more severe in the morning and is associated with a lot of white mucoid or serous frothy sputum, the sputum becomes purulent when the patient has infection. The patient often feels dyspnea and chest dicomfort, which worsens during exercise, and dyspnea gradually progresses. [Signs] No obvious signs are found in the early stage,in acute exacerbations one could hear sparse dry or moist rales. often located at the lung bases, decreased or disappeared after cough. The amount and location of the rales are often variable. More rhonchi associated with elongation of expiratory phase could be heard for the asthmatic pattern of chronic bronchitis. In patient with obstructive emphysema, one could find barrel-shaped thorax,, narrow intercostal space, decreased respiratory movement, weakened vocal fremitus and resonance, hyperresonance over the lungs to percussion, lowerness and the diminished movement of the lower lung margins. Heart dullness area is smaller, the lower liver margin is displaced downward. Alveolar breath sound with elongation of expirtory phase is diffusely distributed, moist rales could be heard on two lung bases. (3) bronchial asthma Chronic bronchial inflammation is mainly caused by allergic reaction. Airways are highly sensitive to various stimuli, and this can lead to diffuse reversible airway obstruction for the vulnerable ones. At the attack, bronchial smooth muscle is spastic, mucous membrane is congestive and edematous, and the gland oversecretion is common. [symptoms] Majority patients start in young or adulthood, repeatedly occur with the change of seasons. Contact with allergens are often present before the attack, patients often have symptoms associated with respiratory infection or allergic manifestations, such as nose tickling, sneezing, snivel or dry cough. Then chest discomfort and shortness of breath quickly appear, lasting hours or even days, the asthma usually relieves gradually after more or less thin sputum was spit out. [signs] Patients usually have no obvious signs during resolution stage, while during the attacks, they appear severely expiratory dyspnea, showing orthopnea, with the recruitment of respiratory ancillary muscles. The grave patients may show cyanosis, massive diaphoresis, full thorax, diminished respiratory movement with the chest almost at the inspiratory position, diminished vocal fremitus and hyperresonance on percussion, dry rales and wheezing sound could be heard on both lungs. Patients with prolonged duration and multiple recurrence may be complicated by obstructive emphsema, and will show related symptoms and signs. (4)pleural effusion Pleural effusion is produced because the static pressure of the pleural capillaries are elevated (eg. heart failure), lower osmotic pressure (hypoalbuminemia due to liver sclerosis, nephropathy) or higher capillary wall permeability(eg. TB, pneumonia and tumor etc.), resulting in increase of production or decrease of absorption of fluid in the pleural cavity. Besides, impaired drainage of pleural lymph and trauma also could lead to pleural effusion or hemothorax. Pleural effusion could be classified into exudate and transudate due to different etiologies. [Symptoms] Symptoms are often not obvious if effusion is less than 300 ml, however, patients with small amount inflammatory fibrous exudation often complain of irritative unproductive cough, worsened on inspiration, and accompanied by chest pain on the affected side. Patients would rather lie on the affected side to restrict respiratory movement of this side in order to alleviate pain. When effusion increases, parietal and visceral layers of the pleura separate, pain may become milder or even disappeare. Patients with more than 500 ml effusion often complain of dyspnea and chest discomfort. Huge effusion may press or even displace mediastinal organs to cause palpitation, dyspnea, orthopnea or even cyanosis, besides the symptoms due to pleural effusion itself, patients often have symptoms of the orginal diseases, for example, they have fever and toxic symptoms because of exudate due to inflammation, and have symptoms of HF, ascites, edema etc if the effusion is of non-inflammatory transudate. [Sign] Patients with small amount of effusion often have no obvious signs, or they may only show diminished chest wall movement on the affected side. In the patients with moderate or large amount of effusion, there could be seen shallow respiration, restricted movement of affected side, wide intercostal space, displacement of apex beat and trachea toward the opposite side, or absent apex beat. In patients with moderate amount of effusion without thickening and adhering of the pleura, one could percuss out Damoiseau line of the upper margin of effusion. Garland triangle on the upper and back area of the effusion, Scoda hyper-resonant area above and in front of area on the normal side.(Fig. 3-5-19). In patients with huge effusion or effusion with thickening and adhering of the pleura, flatness on percussion is common, over the effusion areas, breath sound and vocal resonance are diminished or absent, bronchial breath sound sometimes could also be heard. Pleural friction rub is often heard in fibrinous pleuritis. (5) pneumothorax Pneumothorax means that the air enters the pleural cavity. If the pneumothorax is caused by rupture of visceral layer of the pleura, due to bleb beneath the surface of the normal lung, chronic respiratory emphysema, or pulmonary TB, it is called spontaneous pneumothorax. Sometimes doctors inject filtered air into the pleural cavity artificially to treat some diseases, such pneumothorax is called artificial pneumothorax. Besides, those caused by thoracic injury or acupuncture are called traumatic pneumothorax. [symptoms] Inducing factors are often as follows, holding heavy things, holding breath, strenuous exercises or cough. Patients feel ipsilateral chest pain suddenly and progressive dyspnea, sometimes, they can’t lie supine and so have to lie on the normal side, let the affected side upward in order to alleviate pressing symptoms. Patients could have cough, with or without sputum. In mild closed pneumothorax only mild dyspnea is present, and patients may calm down several hours later. Severe tension pneumothorax patient, may show nervousness, restlessness, diaphoresis, rapid pulse, syncope, cyanosis and even respiratory failure besides dyspnea. [Signs] Patients with mild pneumothotax often have no obvious signs. When air trapped in the pleural cavity is voluminous, then on the affected side appear fullness of the chest, wide intercostal spaces, diminished respiratory movement, and diminished or no vocal fremitus or resonance. Trachea and heart displace toward the Cons olidat ion Emph ysem a Atele ctasis Pleur al dffusi on Thick ened pleura pneu moth orax healthy side, tympanic sound on percussion, liver dullness edge displaces downward when pneumothorax is on the right side. Breath sound is diminished or disappeared on the affected side. Coin sign is positive. The signs of common pulmonary and pleural diseases are listed in table 3-5-1 Table 3-5-1 inspection palpation Percussio Auscultation n Chest Respirato Trachea Vocal Note Breath rale Vocal appearance ry location fremitus sound resonance movemen t Symmetrica Diminish Central Increased Dullness Bronch Moist Strengthened l ed on the on the or ial rale affected affected flatness breath side side sound Barrel-shap Diminish Central Diminish Hyperres Dimini Always Diminished ed ed on ed on onance shed without both sides both sides Denting of Diminish Deviate Diminish Dullness Disapp Withou Disappeared or the affected ed on the toward ed or eared t diminished side affected the disappear or side affected ed diminis side hed Fullness of Diminish Deviate Diminish Flatness Dimini Withou Diminished or the affected ed or toward ed or shed or t disappeared side disappear the disappear disappe anced on normal ed ared the side affected side Denting of Diminish Deviate Diminish Dullness Dimini Withou Diminished the affected ed on the toward ed shed t side affected the side affected side Fullness of Diminish Deviate Diminish Tympany Dimini Withou Diminished or the affected ed or toward or shed or t disappeared side disappear the disappear dissape anced on normal ed ared the side affected side E . The Heart In the present era of technological advances, particularly in the various imaging modalities, there is a growing conception among practicing physicians in cardiovascular medicine that bedside physical examination is unnecessary and does not provide useful information. It should be emphasized, however, that for proper application and interpretation of various new and old tests that are available for cardiovascular evaluation in a given patient. Bedside clinical examination should be performed and practiced in the same way following similar sequences. Preparing the patient The heart examination should be made as easy as possible for the patient, who usually expects it to be a relatively distasteful experience. If the physician is considerate and gentle, the patient should feel when it is all over, that most of his or her fears on that score were unfounded. The ideal examining room is private, warm enough to avoid chilling, and free from distracting noise and sources of interruption. Adequate (preferably fluorescent or natural) light is essential. The examining table may be placed with its head against the wall, but both sides (particularly the right) and the foot should be accessible to the examiner. And the results should be recorded carefully. Inspection 1. Observe precordium Inspection of the precordium should begin at the foot of the bed. The subject should be supine with the legs horizontal and the head and trunk elevated to approximately 15-30 degrees. Asymmetry of the thoracic cage due to a convex bulging of the precordim suggests the presence of heart disease since childhood, such as congenital heart disease and rheumatic heart disease, with skeletal molding to accommodate cardiac enlargement. In the adult, precordial bulge may be produced from the massive pericardial effusion. 2. Apical impulse The apical impulse is occurring early in systole. In adults the apical impulse normally is located in the left fifth intercostal space, either at or medial to the mvl and about 2-2.5 cm diameter, it serves the examiner as a marker for the onset of cardiac contraction. Displacement of the apical impulse: a) Heart disease: Some heart diseases cause the left ventricular hypertropy dilatation or both, the apical impulse is displaced laterally and inferiorly and sustained, and it may be shifted to the left and upward in right ventricular hypertrophy, dilatation or both. It can be found at the right fifth intercostal space in dixtrocardiac and can not be found in massive pericardial effusion. b) Thoracic disease: pneumothorax and pleural effusion will displace the apical impulse to the normal side. Pleuraladhesion and ateleotasis will result in a displacement of impulse toward the diseased side. c) Abdominal disease: The apical impulse also can be displaced by large mass, massive ascites. d) The apical impulse may have increased amplitued and duration in those persons with a thin chest, anemia, fever, hyperthyroidism and anxiety. The examiner should always observe the shape and contour of patint’s chest. Depressions of the sternum, Kyphosis of dorsal spine, scoliosis often alter the shape and position of the apical impulse. Abnormal pulsations in the other areas. a) Right vertricular hypertophy (RBH). The impulse is clearly seen in left third fourth intercostal space. b) Pulmonary emphysema with RVH, usually the pulsation can be found inferior the xiphoid process. c) In asending or arch aortic aneurysm, one may detect abnormal pulsations in aortic area, with bulging or pulsation in systole. d) Pulmonary hypertension with dilatation the pulsation in systole may be detected in left second intercostal space to the edge of sternum. palpation Usually inspection and palpation are discussed together because there is an intimate relationship between these two processes in the heart examination. Palpation not only confirms the results in inspection, but also discovers diagnostic signs. Through careful palpation, the examiner should aim to determine the location and size of the cardiac apex impulse, characterize its contour, and identify any abnormal precordial pulsations. The palm of the hand, ventral surface of the proximal metacarpals, and fingers should all be used for palpation because each is useful for optimal appreciation of certain movements. 1) Usage of the palpation confirms the precordial pulsation’s location. Amplitude, duration and intensity. In left ventricular hypertrophy (LVH) the impulses are very forceful, sustained throughout systole and has a great amplitude. The apical impulse may have decreased amplitude and duration in those patients with myocarditis. In massive pericardial effusion the impulse cannot be palpable. 2) Thrills are actually palpable fine vibrations, most commonly produced by blood from one chamber of the heart to another through a restricted or narrowed orifice, it may occur in systole, diastole, presystole and at times may be continuous. Any thrill should be described as to its location, its time in cardiac cycle, and its mode of extension or transmission. The intensity of the thrill varies according to the velocity of the blood, the degree of narrowing of the orifice and which it is produced and difference in pressure between the two chambers of the heart. Quality of a thrill depends on the frequency of vibration producing it, rapid vibrations result in fine thrills whereas slower vibrations produce coarser thrill. 3) Pericardial friction rub is a to-and-fro grating sensation, which is usually present during both phases of cardiac cycle, often rubs are more readily palpated with the patient sitting erect and leaning forward during the end period of deep inspiration. The rub is caused by a fibrinous pericarditis. In the presence of pericardial effusion the rub will usually disappear because of the separation of visceral and parietal layers by the accumulated fluid. Percussion The chest is percussed to confirm the cardiac borders, size contour and position in the thorax, patient should lie supine on an examining table or sit on the chair, with the physician at his right side. Usually we employ indirect percussion for percussing heart borders. It is outlined by percussing in the 5th, 4th, 3rd and 2nd interspace on the left sequentially, starting near the axilla and moving medially until cardiac dullness is encountered. The beginner should mark with a skin pencil where the note changes. The distance from left midsternal line to the left border should be measured and recorded, measurement should be made along a straight line paralleled to the transverse diameter in the thorax. 1) The heart borders (1) The base of the heart, formed by both atria, corresponds to a line crossing the sternum obliquely, from the lower border of the second left costal cartilage, at a point just to the left of its juction with the sternum, to upper border of the third right costal cartilage, at a point 2 cm lateral to its sternal junction. (2) The right border of the heart: It confirms with a curved line with its convexity toward the right, extending from the upper border of the third right costal cartilage 2 cm lateral to its junction with the sternum, to the sixth right chondrosternal articulation. (3) The left border of heart. It is formed by the left ventricle and the atrium and is represented by a curved line with its convexity directed upward and toward the left, extending from the 5th left interspace 1.5 cm medial to the Mvl, to the lowerborder of the second left costal cartilage 1-2 cm, to the left of its articulation with the sternum. (4) The inferior border: It is formed by the RV and a lesser extent by the L V, is represented by a line drawn from the 5th chondrosternal articulation to the site of the cardiac impulse in the left 5th intercostal space 1-2 cm to the M. V. I. 2) Normal relative dullness of the heart Right Intercostal space Left (cm) 2-3 II 2-3 2-3 III 3.5-4.5 3-4 IV 5-6 (cm) V 7-9 In normal person the distance from the 5th to the midsternal line is about 7-9 cm. 3) Changing cardiac dullness Heart disease Left ventricular enlargement, the cardiac dullness will be extended to the left and downward, the heat silhouette is like a shoe. It is frequently seen in aortic regurgitation and called aortic heart. Right ventrucular enlargement, the cardiac dullness will extended to left and upward. The right ventricular is severely enlarged the right border of the hert will extended to the right. Left atrium and pulmonary dilatation Both the left artrium and pulmonary artery enlarged, the pulmonary artery will be exaggerated to leftward. The cardiac silhoutte is like a pear and called mitral heart, it is frequentlyseen in mitral valve stenosis. Aortic dilation, aneurysm of aorta, pericardial effusion, all those diseases may cause the base border of heart enlargement, so that the base border of the heart will be widened. Congestive heart failure, myocarditis, myocardiopathy and pericardial effusion may cause the heart silhouette extending both to right and left. Especially in presence of pericardial effusion, percussion at times may be helpful in outlinging the changing cardiac silhouette resulting from a change in the patient’s position. AUSCULTATION OF THE HEART The purpose of auscultation of the heart is to find the normal and abnormal sounds of the heart. It plays a very important role in the diagnosis of heart disease. It is a very interesting thing to master the auscultation, but it is difficult. For a thorough examination, auscultation must be done with the patient in a sitting, lying, and left lateral recumbent position, and change the position of patient in order to detect some abnormal sounds and murmurs. while the patient roll onto his left side, the murmur at the apex will be hear more clearly. Exercise is valuable for increasing the intensity of faint murmurs. In auscultation, sometimes let the patient holding the breath at the end of expiration, the murmur will be hear easier. I. Auscultatory Valve Areas Sounds produced by each valves of the heart may propagate to different area at the pericardial area following the blood stream. At this area, one can hear the sound clearest in auscultation. It is called “auscultatory valve area”. The auscultatory valve area does not correspond with the anatomic location of the valve themselves. l. Mitral valve area: it is at the apex, in the fifth left intercostal space, medial to the midclavicular line. 2. Aortic valve area: there are two auscultatory area of AV, one is located in the second right intercostal space, just lateral to the sternum. The other is at the third or fouth intercostal space, left to the sternum border. We call it the second auscultatory area of AV. 3. Pulmonary valve area: in the second intercostal space just lateral to the sternum. ; 4. Tricuspid valve area: at the lower part of the sternal near the xiphoid. . The physician should adopt a systematic way of listening: start at the apex, then move to the PV area , AV area, second AV area, TV area. Beside, according the clinical feature, the other part of pericardium, neck, axilla, and back may be examined. Ⅱ. The Content of Auscultation It includes rate, rhythm, heart sound, murmur and pericardial friction sound. 1. Heart rate: It means how many beats per minute. It normally varies with age, sex, physical activity and emotional status. In normal adults: 60-80/min Sinus tachycardia : >1OObeats/min in adults; Sinus bradycardia : <=60 beats/min in adults. 2.Heart rhythm: It is regular in Normal adults, but young adult and children may sinus arrhythmia. The most common arrhythmias in clinical practice are: premature beat (extrasystole) and atrial fibrillation. Premature beat is a sudden extrasystole of the heart in the basis of normal heart rhythm ,and followed by a longer compensatory pause. The characteristic auscultation of extrasystole is: (l) The intensity of S1 is increased; (2) The intensity of S2 is decreased or even disappeared; (3) The peripheral arterial pulse is absent. Atrial fibrillation: It is the common arrhythmia in clinical. It is caused by a very high frequency impulse coming from the atrial ectopic point or caused by the circus movement of the ectopic impulse. The clinical auscultatory characters are “three inconsistence”; (1) The ventricular rhythm has absolutely no regularity; (2) The intensity of S1 is inconsistence; (3) The rate of heart and pulse are unconcerned. 3. Heart sound A. Normal heart sounds In most of normal individuals there are four heart sounds. The first and second sounds can be heard with ease in normal subjects. However, the third sound only can be heard in young person and children. The fourth sound is frequently inaudiable. The producing mechanism of heart sound 1) S1: Although several cardiac events play a part in the production of the S1 , the vibration of the closure of the atrioventricular valves is the most important and accounts for most of the sounds that are heard. The S1 indicates the beginning of the ventricular contraction. Phonocardiographic analysis shows four components in the S1, which have been related to the various events occuring at the onset of systole: (a) Development of tension in the ventricular musculature; (b) Closure of the Atrioventricular valves; (c) Opening of the semilunar valves and the onset of ventricular ejection; (d) Acceleration of the blood in the arteries during maximum ejection. Often some residual vibrations of auricular origin occur at the very beginning of the S1.Normally, only the components due to the closure of the AV valves and the opening of the similar valves are heard, but the either components may be heard under abnormal circumstance. S1 can be heard at any part of pericardium, loudest at apex, lower in pitch than those of the S2,with 55-58 Hz in frequency, last about 0.1 second, longer than those of the S2. 2) S2: The second heart sound is mainly produced by the vibration of the closure of the semilunar valves during the beginning of the ventricular diastole. It is a composite sound result from closure of both the aortic and pulmonary valves. The vibration of the relax of ventricular muscle in diastole, the moving of blood flow within the great vessels, the opening of MV and TV, are taken part in the formation of S2. The exist of S2 is an indicator of the beginning of ventricular diastole. It can be heard at any part of pericardium and loudest at the basic. The S2 is high in frequency and shorter in lasting duration than the S1 It has a snapping-like tone. 3) S3: The third heart sound is heard in most children and some adults. It occurs in early diastole approximately 0.12-0.18 second after the S1. Being lower in both frequency and intensity. It occurs during the phase of early diastolic filling, the blood moves into ventricle rapidly from atrium, produces the vibrating of ventricle wall. Usually it is heard clearly at the apex or superinternal of the apex. 4) S4: The fourth heart sound occurs late in diastole or just prior to the S1 about 0.l second , produced in the ventricle during the ventricular filling associated with an effective atrial contraction. It is also low in frequency and intensity and rarely heard under normal conditions. b. The differentiate between S1 and S2: 1) The S1 has a lower pitch, a longer lasting time. It is maximal in intensity at the apex. The S2 has a higher pitch, a shorter lasting time. It is maximal in intensity at the basic; 2) The duration between the S1 to S2 is shorter (has a shorter pause) than the duration between the S2 to the S1 of next cardiac cycle (has a longer pause); 3) The S1 is synchronized with the apical pulse. and is mimic coincident to the aortic artery pulse. The S2 is produced after the apical impulse. B. Abnormal Heart Sounds Change in loudness 1) Both the S1 and S2 are affected simultaneously: Both increased; both decreased; 2) Change of S1:It depends on the myocardial contraction, the filling degree of ventricle, the elastic and position of the valve. S1 increased: (1) In the situation of high fever, hyperthyroidism and ventricular hypertrophy, (2) In MS (3) In complete AV block S1 decreased: (1) It occurs in myocardial infarction; (2) In mitral insufficiency; (3) In aortic insufficiency. In arrhythmia, the S1 at apex may be louder or weaker. 3) Change of the S2:It mainly depends on the pressure within the aorta and pulmonary artery and the situation of semilunar valves. (1) S2 Increased at aortic valve area :It is due to the pressure increased within the aorta. (2) S2 increased at pulmonary valve area: It is due to pulmonary hypertension. (3) S2 decreased at aortic valve area: It is due to aortic pressure diminished. (4) S2 decreased at pulmonary valve area: It is due to the pressure diminished within the pulmonary artery. b. Change of the quality of the heart sound If the myocardial muscle is damaged severely, the heart sound like a pendular, it is called pendular rhythm. If accompany with tachycardia, like the heart sound of embryo, it is called embryocardia. c. Splitting of heart sounds. Splitting of S1 :It is due to the closure of MV and TV asynchronously, loudest over the apex. It may occur in normal children and young person, and usually occur in right bundle branch block. Splitting of S2:It can be heard in following conditions. (1) In normal person; (2) In pathological situation: conditions that cause an over volume to empty or delay of emptying time of one side of the heart will produce splitting of the S2. (3) The influence of respiration: in inspiration, the pressure within the thorax is decreased and the venous return to right heart is increased. The RV require a slightly longer period to empty it itself, the PV closure does not occur until the ventricle has emptied itself, so make the S2 splitting slightly in normal condition. In pathological situation, if the splitting of S2 is due to the abnormal of right side of the heart, inspiration will produce the S2 splitting more. If the abnormal is within the left side of the heart, such as AS, the emptying time of left ventricle is delayed. The order of valve closure may be reversed, the two components then more closer together or may be single, this is referred to as paradoxical splitting of S2. (4) Fixed splitting of S2: in the usual case of ASD, the S2 over the PV area is widely split, with little or no change in .the degree of splitting during either phase of respiration. This is referred to as fixed splitting. d. extra sounds: The extra sounds in systolic period 1) Early systolic ejection sound: In the presence of dilatation of the aorta or pulmonary artery, or in the hypertension of aorta or pulmonary artery, it can be heard. (1) Pulmonary early systolic ejection sound : It can be heard after S1 with a high pitch sharp. They are best heard at the left side of the sternal border, in the 2-3 intercostal space. These sound are not transmit to the apex. It can be heard in obvious pulmonary dilation and pure PS. (2) Aortic early systolic ejection sounds: It appear after the S1, have the equal quality of pulmonary artery early systolic click. They are heard over the base of heart as well as at the apex. 2) Mid and late systolic click:It occurs in MVP. The redudent and floppy of the tandae chordea can not control the mitral valve at annul level and prolapse into the LA at late systolic period. In systolic period the pathological tandea chordea suddenly be tight, produce vibration, so the click occurs. Sometime it may produce MI, so there is SM after the click.The click usually occurs after the S1 close to the S2, best heard at apex. The pitch is lower that in early systolic click. The extra sounds in diastolic period: 1) Gallop (l) Protodiastolic gallop rhythm: It is termed S3 gallop orS3 gallop. It is the pathologic counterpart of the S3 and occurs at the time of rapid diastolic ventricular filling.It is a brief low-pitched sound It occurs at middle diastole at the end of rapid filling phase of diastole. In the early diastole, the blood through into the ventricle from the atrium in failing myocardium, the tension is poor, produce the vibration of the ventricular wall.. It reflexes that the LV function is decreased. (2) Presystolic gallop: The extra sound in prespstolic gallop is pathological S4.It is termed as S4 gallop or atrium gallop.It occurs in late diastole and is temporally related to atrial contraction . It is due to the increasing contraction of atrium.It occurs precede the the S1. It is low-pitched, best heard at the apex or 3-4 intercostal space, left to the sternal border. (3) Summation gallop: It is termed the middle diastolic gallop, produced by the overlapping of early diastolic gallop and presystolic gallop while the heart rate is quite faster. 2) Opening snap of MV: It occurs after the S2 in MS. This sound is brief in duration and high in pitch than other gallop sounds. It is due to the vibration of the opening AV valve suddenly stopped during the blood from LA into LV in early diastole of the ventricle. The opening snap of the MV usually indicates a flexible valve, and its presence is, an evidence that the valve is probably suitable for mitral commisurotomy operation. 3) Pericardial knock: In the presence of constrictive pericarditis, at time an extra sound is heard in diastole, occuring shortly after the second heart sound. This is reffered to as the pericardial knock. It may be heard all over the precordium and loudest at the apex and left side at lower part of the sternal. It is due to the constriction of the pericardial after inflammation, the diastole of ventricle are eliminated at the ventricular rapid filling phrase in early diastole, the ventricular diastole has to stop suddenly produces the vibrate of ventricular wall. Quadruple rhythm In some pathological situation, when the presystolic gallop and protodiastolic gallop both sounds are present, a quadruple rhythm results. The heart rate usually increased , the presystolic gallop and protodiastolic gallop usually summate together, this is the summation gallop. In the therapy of pacemaker, there are some abnormal heart sounds, murmur and extra sounds. The pacemaker sound is produced by the contraction of the local intercostal muscle due to the leakage of the electric current stimulate the intercostal nerves. In the patients suffering from valvular disease, after the operation of valvular replacement, the prosthetic valve as in mechanical valve, the abnormal heart sound are produced by the crush of metal stent or metal annuls of the valve, such as the click sounds. Heart Murmurs 1. General considerations l) Heart murmurs are an abnormal sound; 2) It should be differentiate from the heart sounds; 3) It has a very important clinical value. 2. Mechanism of production: Mechanism of production: Heart murmurs are abnormal sounds produced by vibrations within the heart itself or in the walls of the large arteries. It usually caused by one of the following mechanisms: l). Increased velocity of blood flow though normal valves; 2). Forward flow though narrowed or deformed valves; 3). Backward or regurgitant flow through incompetent valve; 4). Abnormal connection; 5). Vibration of loose structure within the heart; 6). Increase with diameter of a major vessels. 3.Characterized of murmurs: 1. Location: murmurs of valvular origin are usually best heard over their respective auscultatory valve area. 2. Timing: murmurs are timed according to the phase of the cardiac cycle during which they occur. There are three basic types of murmurs: systolic, diastolic and continuous. 3. Quality: the quality of murmur depends on the frequency and intensity of the sound wave, and related close to the pathology and hemodynamic changes of the heart. We usually describe the SM as blowing, harsh or musical. About the DM, it may be describe as blowing, sigh-like and rumbling. The CM are described as machine-like and hum. 4.Radiation: some murmurs are transmitted with the direction of the bloodstream by which they are produced, other murmurs are propagated from their point of origin in many directions. 5.Intensity: the intensity of murmurs are related to several factors: (1) the severity of abnormal; (2) the velocity of blood flow; (3) the pressure gradient of crossing valve. The most widely used system (Levine and Harvey)for grading the intensity of heart murmur is six-point scale: grade 1 murmur is barely audible and is often missed on the first cardiac examination, grade 2 is usually readily heard and slightly louder than grade 1, grade 3 and 4 are quite loud and grade 5 is even more pronounced, grade 6 may be heard with the stethoscope just removed from the chest wall. . A murmur that increases in intensity after its onset termed “crescends”. If it decreases in intensity, it is referred to as “decrescends”. If the first portion of a murmur is increases in character and the latter portion is decreased it is then referred to as a “diamond-sharped” murmur. 6.Physiological maneuver : The examiner may intervene in several ways to modify sounds and murmurs for the purpose of better recognition and differentiation. Some of the most helpful maneuver are discussed below: 1.Change the body position: it may produces some heart sound or murmur increase or decrease. The murmur of mitral stenosis is more evident in left recumbent position. In sitting position, leaning forward, held respiration in the end of deep expiration, is useful to the ausculation of aortic insufficiency murmur. Prompt squatting from standing position or raising two legs at supine position may increase venous return, therefor increase the strock volume and cardiac out put, increase the murmur of MI and AI .The murmur of hypertrophic obstructive cardiomyopathy is decreased in squatting and increased in standing position. 2.Respiration: respiration may change the output volume of left and right ventricle, then inflence the tensity of the murmur. During deep inspiration, the pressure with in the thorax decreased, the venous return increases, the blood volume of pulmonary circulation increases, therefore the output volume of right side heart is large than those of left side heart and the heart has a clock wise rotation along long axis ,the tricuspid valve closes to the chest wall more, produce the murmur of TI,TS,PI increase in intensity. It is in the opposite way during expiration. 3.Exercise: exercise increases heart rate, blood volume of circulation and blood velosity, so the murmur due valvular stenosis will increase. Ⅳ.The clinical value of murmur in each valve area of auscultation. Heart murmur usually is a feature of the disease of cardiac or vessels. It may appear in rare normal individuals. The abnormal which produce the murmur may be organic, relative, and functional.we call it organic, relative, and function murmur. The term “relative M” indicates the valves itself is not involved but the supporting tissues of the valves are abnormal. It consist the dilation of the valve annulus, the damage of chordae tendineae, the enlargement of cardiac chamber or great vessels, and produce a relative stenosis or insufficiency of the orifice of the valve. The functional M usually reveals in systolic period in part of healthy child or young person or in the situation due to increasd flow across a normal valve. (1) Systolic murmur 1) MV area: the murmur at apex is produced by mitral insufficiency. Its origin and cause may be organic, relative or functional. Organic MI most are due to rheumatic heart disease, MVP and dysfunction of papilly muscule. It is a pansystolic M,overlap the S1,high-pitched, blowing in charter, more harsh, louder than 3/6 degree in decresento type and frequently radiate toward the left axilla. It is diminished in inspiration, increased in expiration. It is best heard in left supine position. Relative MI: It is due to the dilated LV. It is heard in hypertensive heart disease,acute rheumatic fever, dilated cardiomyopathy and severe enemia.The M is in soft charter and less in radiation. Functional MI: the valve is normal but the blood flow is quite faster. It is heard in high fever, enemia in middle degree, hyperthyroidism, usually is less than 2/6 degree, in soft charter, more local in area, does not radiateto other part. The M will disappear when the cause producing faster velosity of the blood flow disappeared. It is heard in part of the normal adult. When valvular insufficiency exists, the ventricular pressure remains above atrial pressure throughout systole. When the aortic and pulmonary valves close, the ventricular pressure is still well above the atrial pressure, thus the murmur of Mi is heard throughout systole and for a brief period following the S2. 2) AV area: it is heard in organic AS. The murmur is harsh in charicter, cresendo-decresendo type, radiate toward the neck following the great vessels, usually are accompanying with systolic thrill and S2 is diminished at AV area.It is also heard in relative lesion of AV, such as dilation of aorta due aortic arteriosclerosis, hypertensive heart disease. 3) PV area: it is an ejection murmur, most of them are functional.It can be heard in part of normal children and young person. It is soft and weakness in charter. This murmur may exist in relative stenosis of the orifice of pulmonary artery, due to pulmonary artery dilation in pulmonary hypertension,such as ,MS, ASD.The organic murmur in this area are produced in congenital PS. It is louder in intensity, harsh in quality, diamond-shaped, usually accompanying with systolic thrill. The S2 decreased in this area. 4) TV area: The systolic murmur in this area indicates Ti, most are relative TI due to dilate of right ventricle. It is a blowing SM, increased in inspiration. The organic SM are very rare here. . 5) Other position: In VSD, a loud and harsh SM can be heard at third and fourth intercostal space, left to the sternal border, usually are accompanying with systolic thrill. (2) Diastolic murmur: 1) MV area: Most of them are produced by organic lesion of the valve. In rheumatic MS,an mid-late rumbling diastolic murmur can be heard at the apex, cresendo-sharped, in low-pitch. It is generally confirmed to a rather small area, best hears in left recumbent position at the end of expiration, usually are accumpanying with louded S1, OS of MV and diastolic thrill. The DM of relative MS may occurs in AI.It is termed Austin Flint murmur. Do not accompanying with louding S1 or OS.The mechanism are the blood regurgitating from the aorta into LV stricking the MV area up,produce relative stenosis of MS. d. 2) AV area: The murmur begins immediately after the AV closure sound.It is usually heard in rheumatic AI. The murmur are sigh-like, decresedo, may radiate to the left side of the lower part of sternal. It is best heard at the aortic second area, 3) PV area: The diastolic murmur at this area, most are produced by relative Pi. The Grahan Steell murmuris also a relative murmur. 4) TV area: It is rare in clinical. (2) Continuous murmur: Murmurs which extend from systole into diastole are called continuous murmur, such as in Patent Ductus Arteriosus. It is a continunous murmuur, harsh in quality, mimic the sound of machine rotating.It is best heard at second intercostalspace, left to the sternal border. The murmuer begins after S1, middle pitch,cresendo type, recher peak intensity at late systole, envelop the S2 and decreased at early-middle diastole, produceing a large diamond sharp, persistent from systole to diastole, the peak of diamond is at the top of S2. Continuous murmur can also be heard in arterio-vein fistula. Pericardial friction rub The pericardial friction rub is produced by the rubbing on each other of the parietal and visceral surfaces of the roughened pericardium during pericadiatis. The sound is usually in both systolic and diastolic, with a to-and-fro character, but the systolic component predominates, and sometime the sound is heard only during systole. In general, the sound is harsh, resemble massage the ear using the finger. At times, it is soft, it seems closer to the ear than the heart sounds. The rub is most commonly heard at the third to fourth intercostal space left to the sternal border. It is best heard in the sitting position leaning forward and held breath.The common cause of pericardial friction rub is pericarditis(TB,non-spicific, rheumatic). It also can be seen in acute myocardial infarction, uremia and SLE. F. THE BLOOD VESSELS ⅠPulse The palpation of artery is an important step in the cardiovascular examination. From here We can get data of the patient above the general condition, the function of circulation, and some cardiovascular abnormalities. So it has an important value in the clinical diagnosis. The arterial pulse can be papated at any point where the arteeainst a firmer surface usually bone. l. First pay attention to the intensity and the beginning time of the radial A. and compare the radial A. in both sides if it is equal or not. 2. The pulse intensity may not be equal between the upper and lower extremitries. 3. Compare the pulse of artery of both lower extremtries at the relevant position. In examining the pulse, It Is important bear In mind the following points: rate, rhythm, consistency, intensity, wave form and condition of the arterial wall. a. rate b. rhythm c. tention: The tention of pulse depends on the level of the arterial systolic pressure. d. Intensity: The intensity depends on the arterial filling degree and the resistance of peripheral vessels, it also depends on the cardiac output and pulse pressure. e. Wave form The arterial pulse starts at the instant the valve opens and left ventricular ejection begins. This results in an abrupt sharp rise in aortic pressure, since blood enters the aorta much faster than it flows to the more distal arteries. During the systolic phase of left ventricular ejection a large portion of the blood is temporarily stored in the proximal aorta. Once the aortic pressure reaches a peak it begins to fall as ventricular ejection slows, and blood continues its flow in the peripheral arteries. As the ventricle relaxes there is a transient reversal of flow from the central arteries to the ventricle and the aortic valve closes. The aortic pressure continues to decrease during diastole as blood flow continues to the peripheral vessels. The pulse wave is composed of an ascending limb, peak, and descending limb. There is a small notch near the peak of the ascending limb and a similar notch on the descending limb. l. Water hammer pulse. A strong bounding pulse with a tall rapid ascending limb and an equally rapid decending limb .It is called a water-hammer or collapsing pulse. 2. Pulsus alternans. Pulsus alternans is charterized by a regulary alternating pulse, in which every other beat is weaker than the preceding beat. Actually, there is an alternating series of high and low pulse waves caused by an alternating contractile force of the left ventricle. Since the weak beats are but slightly weaker than the strong beats, this arrhythmia may be overlooked unless the examiner is skilled or alerted to its possibility. It is more likely to be detected when the patient is sitting or standing. It must be distinguished from bigeminy.Consequently it is a valuable indication of left ventricular failure . 3. Dicrotic pulse. In dicrotic pulse there are two impulses that are palpable during diastole. It usually occurs in the presence of high fever and may be palpated in both the carotid and peripheral arteries. 4. Paradoxical pulse. Paradoxical pulse is charterized by a decrease in the amplitude or an actual imperceptibility of the pulse that occure during the inspiratory phase of respiration. This phenmenon is caused mainly by pooling of blood in the pulmonary circuit during inspiration resulting from the expansion of the lungs and an increase in the negative intrathoracic pressure. In turn this results in a decrease in the return of blood to the left side of the heart, a decrease in left ventricular output, and thus a decrease in arterial blood pressure. When the systolic blood pressure falls more than 10 mm.Hg during inspiration the pulse is refferred to as paradoxical. The most accurate means of identifying a sphygmomanometer, since it can be easily overlooked while palpating the radial artery. The presence of a paradoxical pulse should suggest the possibility of massive pericardial effusion, constrictive pericarditis. f.Consistency of the arterial wall. This is best accomplished by expressing the blood from a distal segment of the radial artery that has been ocluded by digital pressure. The trun consistency of this vessel can then be determined by means of palpation. Normally the wall of an artery under these circumstances is soft and pliable. In arteriosclerosis the wall offers more resistance to compression by the palpating finger, and the vessel may be rolled easily between the examining digits. This is often referred to as a “pipe stem” artery may be beaded in consistency and tortuous in its couse. In elderly persons the examiner may actually visualize these snakelike pulsating arteries under the skin of the arms and forearms. 2. Pistol-shot sound 3. Duroziez's sign. 4. Pathological sound: including systolic murmur and continuous murmur. Measurement of Arterial Blood Pressure For routine measurement, the patient may be either sitting or lying in the supine position. The patient should have been resting for some time. Bare the arm and affix on it the collapsed cuff smoothly, so the distal margin of the cuff is at least 3 cm proximal to the antecubital fossa. The cuff is evenly and firmly wrapped about the arm with the center of the inflatable portion over the brachial artery, place the chestpiece of the stethoscope over the brachial A. at the antecubital fosse. The radial pulse is palpeted and inflate the cuff to a pressure about 30 cm of mercury about the point where the palpable pulse disappears. Open the valve slightly ,so the pressure drops gradually(2 mm/second). From this point, observation may be made by either auscultation or palpation. Press the bell of the sterhoscope hightly over the brachial A. and note the pressure reading at which sounds first become audible, this reading is taken as the systolic pressure. As the blood pressure cuff is further deflated, the sounds undergo changes in intensity and quality. As the cuff pressure approaches diastolic, the sounds often quite suddenly become dull and muffled and then cease. The point of complete cessation of sounds is the best index of the diastolic pressure. The systolic pressure is depended on the myocardial contractility and the cardiac output. The diastolic pressure is depended on the resistance of peripheral vessels. The cardiac output decreasing or the peripheral vesseular resistance decreasing may produces the blood pressure drop. Under normal circumstances there is little or no significant difference in the blood pressure in the two upper extremities. In certain instances-for example, aortic aneurysm or obstruction of the innominate artery-there may be a significant discrepancy in the blood pressure in the upper extremities. Blood pressure is somewhat variable and depends on sex, race,and climatic conditions. Some serious causes of low blood pressure(hypotension) include Addison’s disease, acute myocardial infarction, hemorrhage, and shock. Among the causes of high blood pressure(hypertension) are essential hypertension, chronic glomerulonephritis, pheochromocytoma, renal artery stenosis, and coarctation of the aorta. G. MAJOR SYMPTOM AND SIGN OF COMMON DISEASE IN CIRULARORY SYSTEM Mitral stenosis Mitral stenosis(MS) results from recurrent rheumatic activity. During the course of M.S., the flow of blood is damped from left atrium to left ventricle in diastole, left ventricle filling is then decreased, and the left atrial pressure is increased, left atrium is overfilled, causing dilatation and hypertrophy of it. The high atrial pressure induces a dilatation and stasis of pulmonary vein and capillary. Then pulmonary artery pressure increased gradually due to the increased pulmonary circulatory resistance and pulmonary arterial sclerosis developed later on. The right ventricle is overloaded and then the compensatory hypertrophy and dilatation occur. Right ventricular failure may be present finally. Symptoms There is no symptom, or only a slight in a case of mild or moderate M.S. Major symptoms (due to left atrial dysfunction)are as follows. Exertional dyspnea, cough, hemoptysis and occasional paroxysmal nocturnal dyspnea. Signs Inspection: The so-called “Mitral Facies” May be present. The apical pulse may extend to left side. Palpation: diastolic thrill may be felt at apex. Percussion: The cardiac dull area extend to left in early stage and later on to right. A prominence of “cardiac waist” may be present, making the heart to form a pea –shaped dullness. Ausculation : A loud snappy first sound and a localized cresendo rumbling diastolic murmur in the mid-late stage may be hear at apex, which can be clearer when the patient in lying in left lateral position. The opening snap may be present. The pulmonary second sound may be accentuated or splitting. Moist rales at the base of lung may be appeared. X - ray. The lung markings are increased. The heart shadow showed a “ Mitralized contour”. Barium meal of esophagus may show an enlargement of the left atrium which compresses the esophagus backwardly. Enlargement of right ventricle may be present in late stage. EKG: A broad p wave with a notch “Mitral P” and enlargement of right ventricle may be present. Echo: Double -spike of mitral anterior leaflet disappeared and flat curve may be seen. Anterior and posterior leaflets move in same direction. Right ventricular enlargement may be seen in late stage. Mitral Insufficiency (MI) The main cause of MI is rheumatism, and MI may be produced by left ventricular dilatation due to any cause. During left ventricular contraction the blood regurgitates into the left atrium, so that the filling degree and pressure were augmented for the left atrium and them the compensatory dilatation of left atrium occurs. During the left ventricular diastole the left ventricle accepts more blood flow from left atrium and from left ventricle regurgitate. Consequently, the left ventricle bears blood volume so heavily during the left ventricular contraction that the compensatory dilatation and hypertrophy of the left ventricle occur gradually. Symptoms: The patient has fatigue, palpitation in the early stage. If without heart failure, the patient feels no symptom for a long time. Signs: Inspection: The apical beat is displaced to left and lower. Palpation: The apical beat is heavy. percussion, cardiac dullneus enlarged toleft, or right in late stage. Auscultation: a grade Ⅲ or more pansystolic blowing murmur may be heard and transmitted to the left axilla and supscapular region. The first heart sound was decreased and masked by the murmurs. The pulmonary second heart sound was accentuated. X-ray shows dilated left ventricle and left atrium and pulmonary congetion. EKG shows left ventricular hypertrophy. Aortic Atenosis The valvular deformity in aortic stenosis may be the result of rheumatic fever but also occur on the basis of a congenital defect or atherosclerosis. Calcific stenosis may occur when the underlying pathologic condition is either rheumatic or sclerotic. In aortic stenosis blood is forced under great pressure by the left ventricle through a narrowed aortic valve into the aorta. The resistance of output the blood in left ventricle is increased. The wall thickening of LV gatting high and high due to the constraction of LV increased. The mean pressure of aorta is decreased, the blood flow in coronary artery and periphelow artery is decreased. The main symptom are palpation, fatigue,,angina, even syncope. Signs: The apical impulse is increased,and displaced laterally.A systolic thrill may palpable at the second intersapace lateralal to the sternal with a pulsus parvus..In auscultatioin, there is a murmur , systolic in time, loud, harsh, and usually has a crescendo-decrescendo charter. The murmur is ejection in nature, beginning shortly after the first heart sound and ending just before the aortic component of the second sound. The murmur is heard over the right second interspace lateral to the sternum and radiated widely, frequently to the right side of the neck and especially to the apex. The aortic component of the second sound is delayed in most cases and is absent in a few. Consequently, there is either a single second heart sound, or a reversed splitting of the second sound, the aortic component occurring after the pulmonary. Aortic Insufficiency Etiology: The cause of aortic insufficiency are rheumatic fever, the commonest, and arteriosclerosis and infective endocarditis. Syphilis is a less common cause of A.I. in our country now. In aortic insufficiency, the left ventricle receives both blood from left atrium and aortic regurgitation, the augmentation of stroke volume leads to compensatory, left ventricular dilatation and hypertrophy and relative M.I. The regurgitant jet from aorta hits the anterior mitral leaflet and causes it moving toward left atrium during diastole, result in relative mitral stenosis, Because the blood leaks to the left ventricle in diastole, the diastolic pressure is decreased causing an increase in pulse pressure and other signs of peripheral vessels due to A.I. Symptom: The patient may be free symptom or only feels palpitation in the early signs: Signs: Inspection: Patient looks pale, the apical impulse is diffuse and displaced laterally or inferiorly. Palpation: The apical impulse is displaced laterally and inferiorly, lifting impulse may be felt. Percussion: cardiac dullness is enlarged laterally and inferiorly. The “cardiac waist” is decreased. The cardiac dullness shows a boot-shaped shadow. Auscultation: First heart sound is decreased at apical area and the aortic second heart sound decreased or disappeared. A blowing diastolic murmur is audible in the aortic area or third intercostal space left to sternum and transmitted to apex. A soft blowing systolic murmur at apex may be heard due to the relative mitral insufficiency. If there is relative mitral stenosis, a rumbling murmur in early-mid diastole at apex may be heard, it is called “Austin-Flint” murmur. Peripheral varcular signs due to increased pulse pressure are as follow: (l) Moving of head with each heart beat, i.e. Musset sign; (2)Carotid pulsation; (3)Capillary pulsation; water hammer pulse; pistolshot sound; Duroziez dicrotic murmur etc. Pericardial Effusion The commonest causes of pericardial effusion are inflammatory( tubercurosis or purulent disorders)and noninflammetory ( Rheumatism, nephrosis). For a slight effusion, there is no effect on heart and hemodynamics. If pericardial effusion increased rapidly or gradually but massive, the elevated pressure of pericardial cavity limit the dialate of the heart,influnce the blood flow retun from systemic venus to the right ventricle, the ventricular filling and out put were reduced, produceing a serious hymodynsmic changes. Symptom: The severity of symptom depends on the pericardial effusion volume and the velosity of effusion producing.patients may complainpericardial compression, dyspnea. If the effusion compresses the neighboring organs, cough, hiccup, dysphagia may be present. In addition, there are inflammatory symptoms of fever, sweating, fatigue and pericardial pain. Signs: Inspection: It is dyspnea in a sitting, leaning forwarl posture. The cardiac impulse decreased or disappeared. Palpation: Apical pulsation reduced or absent, with fast and small pulse, paradoxlcal pulse may be present. Percussion: Cardiac dullness is enlarged and almost coincide with posture. Auscultation: A faint heart sound and sometimes pericardial friction rub may be heard. Ewa's sign with dullness below the angel of left scapula as associated with the increased vocal fremitus , broncbial breath. Elevated venous pressure, small pulse pressure and positive hepatojugular reflex may be present.