Kas 13-10E: Case report: patient with vision defect
advertisement
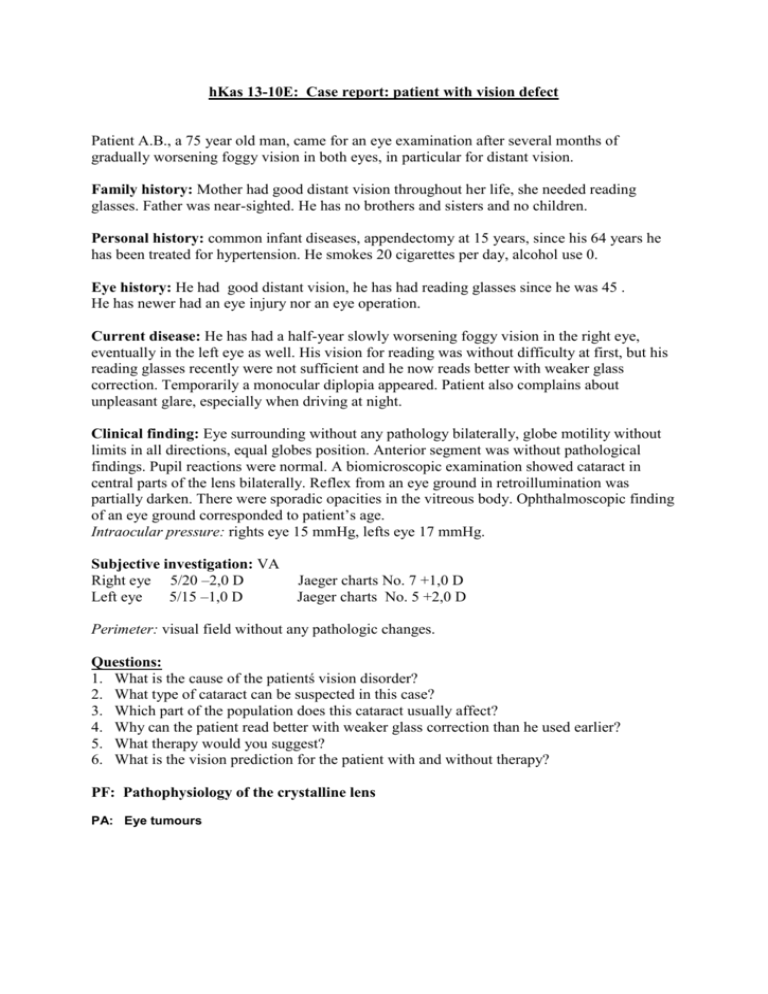
hKas 13-10E: Case report: patient with vision defect Patient A.B., a 75 year old man, came for an eye examination after several months of gradually worsening foggy vision in both eyes, in particular for distant vision. Family history: Mother had good distant vision throughout her life, she needed reading glasses. Father was near-sighted. He has no brothers and sisters and no children. Personal history: common infant diseases, appendectomy at 15 years, since his 64 years he has been treated for hypertension. He smokes 20 cigarettes per day, alcohol use 0. Eye history: He had good distant vision, he has had reading glasses since he was 45 . He has newer had an eye injury nor an eye operation. Current disease: He has had a half-year slowly worsening foggy vision in the right eye, eventually in the left eye as well. His vision for reading was without difficulty at first, but his reading glasses recently were not sufficient and he now reads better with weaker glass correction. Temporarily a monocular diplopia appeared. Patient also complains about unpleasant glare, especially when driving at night. Clinical finding: Eye surrounding without any pathology bilaterally, globe motility without limits in all directions, equal globes position. Anterior segment was without pathological findings. Pupil reactions were normal. A biomicroscopic examination showed cataract in central parts of the lens bilaterally. Reflex from an eye ground in retroillumination was partially darken. There were sporadic opacities in the vitreous body. Ophthalmoscopic finding of an eye ground corresponded to patient’s age. Intraocular pressure: rights eye 15 mmHg, lefts eye 17 mmHg. Subjective investigation: VA Right eye 5/20 –2,0 D Left eye 5/15 –1,0 D Jaeger charts No. 7 +1,0 D Jaeger charts No. 5 +2,0 D Perimeter: visual field without any pathologic changes. Questions: 1. What is the cause of the patientś vision disorder? 2. What type of cataract can be suspected in this case? 3. Which part of the population does this cataract usually affect? 4. Why can the patient read better with weaker glass correction than he used earlier? 5. What therapy would you suggest? 6. What is the vision prediction for the patient with and without therapy? PF: Pathophysiology of the crystalline lens PA: Eye tumours Kas 13-11E: Case report: transient deterioration in vision Mr. A.D., 65 years old man, visited the Eye department because of sudden vision deterioration of the left eye. Family history: parents wore spectacles, mother had strong correction for near and distant vision, son and daughter healthy, without glasses, wife underwent the retinal operation. Personal history: no serious illness, no general treatment, problems with prostate gland recently. Blood pressure 130/85, DM 0, ischaemia 0, normal blood count, neurological problems 0, hormonal therapy 0. Eye history: good sight, since he was 25 years old – spectacles for distant vision. From the age of 40 he wears bifocals. He could see well through the bifocals. Current disorder: while driving a car in the evening he realized blurred vision of the left eye, he saw rings round the lights with the left eye, the eye was slightly more sensitive. Because his wife has been treated in our clinic, he rather came over for investigation. Clinical finding: Right eye: all finding, except the shallower anterior chamber, was normal. Left eye: mild passive conjunctival hyperaemia, corneal stroma oedema was damping out, shallow anterior chamber, slightly wider reactive pupil, normal eye ground. Gonioscopy: Right eye- narrow beaked chamber angle, grade 1, ciliary border concave. Left eye- markedly concave ciliary border, angle differentiable with difficulty, grade 0-1, gently slackening with pressure. Intraocular pressure: right eye 19 mmHg, left eye 45 mmHg. Subjective investigation: VA right eye 6/6 +2,0D Jaeger 1 +5,0D left eye 6/9 +3,0D Jaeger 1 +6,0D Perimeter- visual field examination: (one week later) physiological finding bilaterally. Questions: 1. What was the cause of vision disorder? 2. About what kind of glaucoma is the case report? 3. Which eyes are predisposed to that kind of glaucoma, what can cause the elevation of intraocular pressure? 4. Why did we not find pathological changes of optic nerve head and in the visual field? 5. Which attack can be caused by passing over several attacks of this kind without therapy? 6. What are the local and general signs in acute congestive angle-closure glaucoma? PF: The factors influencing intraocular pressure PA: Eye inflammations Kas 13-12E: Case report: patient with refractive error Mr K.R., 11 years old pupil, appeared in eye examination for foggy vision for distance. Family history: Mother has worn spectacles for distance since her 13. Father has no problems with eyes and no dioptric correction. Personal history: common infant’s diseases, as 9 years old he had an bike injury followed with fracture of the right leg. Eye history: He had good vision and no spectacles until now. Recently he realized worse vision in the school, when looking at blackboard. He was changed into the front desk. But he had the same problems with vision also from this place a few months later. Mother tells, that he has problems during watching a TV and looking for distance. He has no problems with near vision. Clinical finding: Globe motility without limits by all directions, equal globes position. Cornea bilaterally smooth, glossy, clear, anterior chamber slightly deeper, pupil round, in the center, pupilar reactions normal, Iris calm, clear optic media. Fundus is without any pathological findings. Subjective investigation: VA Right eye 5/15 nat. Jaeger charts No. 1 nat. Left eye 5/10 nat. Jaeger charts No. 1 nat. Questions: 1. What is the most likely cause of the boy difficulties? 2. Try to explain the etiology and optic status of the eye in this refractive error. 3. Do we need any further examination for the differential diagnose? If yes, which? 4. What kind of spectacle lenses do we correct this refractive error? Are they: a.) Converging lenses b.) Diverging lenses c.) Cylindrical lenses 5. Is there other possibility to correct the error than the spectacles? PF: Refractive media – basis of pathophysiology. PA: Eye tumours in children Kas 13-13E: Case report: patient with the red eye Mrs. A.B., born in 1963 (40 years-old) visited our eye department with red left eye. She had slightly worse vision with the left eye in comparison with the right eye. She told the pain in the eye only when she looked to the light. Family history: insignificant Personal history: She had had no serious illness, she had never taken any pills, occasionally she has a back pain, and she is smoking. She had some virosis recently. Eye history: She had a good vision, no eye injuries; she has no glasses until now. Now she has approximately 24 hours lasting difficulties, she had woken up after midnight and she was alived to gentle pain above and temporally to the eye. Clinical finding: Eye surroundings without any disorder, unlimited eye movements, no pain. Conjunctiva with diffuse red-violet colour around the limbus, tarsal conjunctiva normal appearance. Cornea clear, glossy, normal deep of the anterior chamber, macroscopically clear, narrow pupil, slightly irregular, photoreaction +. Vitreal opacities, fundus: papilla n.optici pink, well demarcated, macula and vascularity without any pathology. Intraocullar pressure r.e. 16, l.e. 12 mmHg, biomicroscopy LE: small precipitates at the corneal endothelium. Subjective investigation: Vision right eye 6/6 nat. left eye 6/6 hardly nat. Jaeger charts 1 nat. Jaeger charts 1 nat. Questions: 1. What kind of injection is described above and how can we differentiate the types of injections? 2. Why the pupil is narrow and irregular? 3. What the “precipitates” means and in which disease we can find them? 4. What the anterior and posterior synechies are and when we can find them? 5. Which parts of the eye are affected in the case report? 6. Describe the possibilities of the local therapy. 7. What is the pupilar seclusion and what it can cause? 8. Which general investigation would you recommend? PF: Inflammation - local signs PA: Eye inflammations Kas 13-14E: A case-report: what forces the patient to visit eye doctor A patient E.F., 65 year old pensioner, referred for cutting, pain and deteriorated vision on the left eye. Family history: mother had diabetes in her old age, died in 76 years of stroke, father died of heart infarction in 72 years. Sister has hypertension. Personal history: three years ago (for dysuria) incidentally diagnosed diabetes, glycemia at that time 20,0mmol/l. Treated with oral antidiabetics, she doesn´t follow a strict diet, glycemia from 9 to 12, sometimes even 15,0. Eye history: previously no eye problems, bad vision of her right eye in last years but she didn´t mind, she can still read with her left eye. She doesn´t go to any eye check-ups. Complaints: Since yesterday her eye is red, painful and vision is worse. She informed us about contact with branch of tree. Ophthalmologic examination: RE VA (right eye visual acuity): HM (hand movement), certain light perception LE VA (left eye visual acuity): 6/24 uncorr. VA: 6/12 with +1,0 D. Jaeger No.5 with +4,0 D. IOP (intraocular pressure): RE 23mmHg, LE 17mm Hg RE: Eye is quiet, slightly divergent, motility normal, outer segment normal, pupil is 2,5 mm, photoreaction +, cortex lens opacifications, red reflex is dead, blurred due to hemorrhage, therefore other retinal examination is impossible. LE: Partial blefarospasm, conjuctiva is irritated, eye motility is normal, corneal defect epitelial abrasion coloured by fluorescein in central part. Anterior chamber is deep, content without changes, iris is atrophic and quiet, pupil photoreaction +, lens with opacification in periferal cortex, red reflex +. Fundus: optic disc well demarcated, with small new vessels. Arteries narrow, nasally obliterated, veins irregular, tufts of new vessels nasally. More new vessels are in the upper and lower temporal region. Many microaneurysms, dot and blot hemorrhages. Cotton-wool patches in all quadrants. Macula thickened, with clusters of microaneurysms surrounded with hard exudates. Internal examination: medium obesity, BP 190/100, HR 72/min, varices of lower extremities. Laboratory tests: SR 15/30, glycemia 15,0, other tests not available. Questions: 1. What forced her finally to visit eye doctor? 2. What is the principal eye diagnosis, what is its etiopathogenesis, what is its probable duration and the control of the disease? Think about the relation to the patient´s history, the education of the patient and other circumstances. 3. Assess the finding on the left eye. 4. Evaluate the findings on the right eye, why eye is nearly blind? 5. Why the right eye is in divergent position? 6. Summarize the case report and formulate principles of co-operation between the patient and his attending physicians. PF: Complications of diabetes – theirs pathophysiology PA: Microangiopathic complications of diabetes