surgery for encapsulating peritoneal sclerosis has a sucessful
advertisement
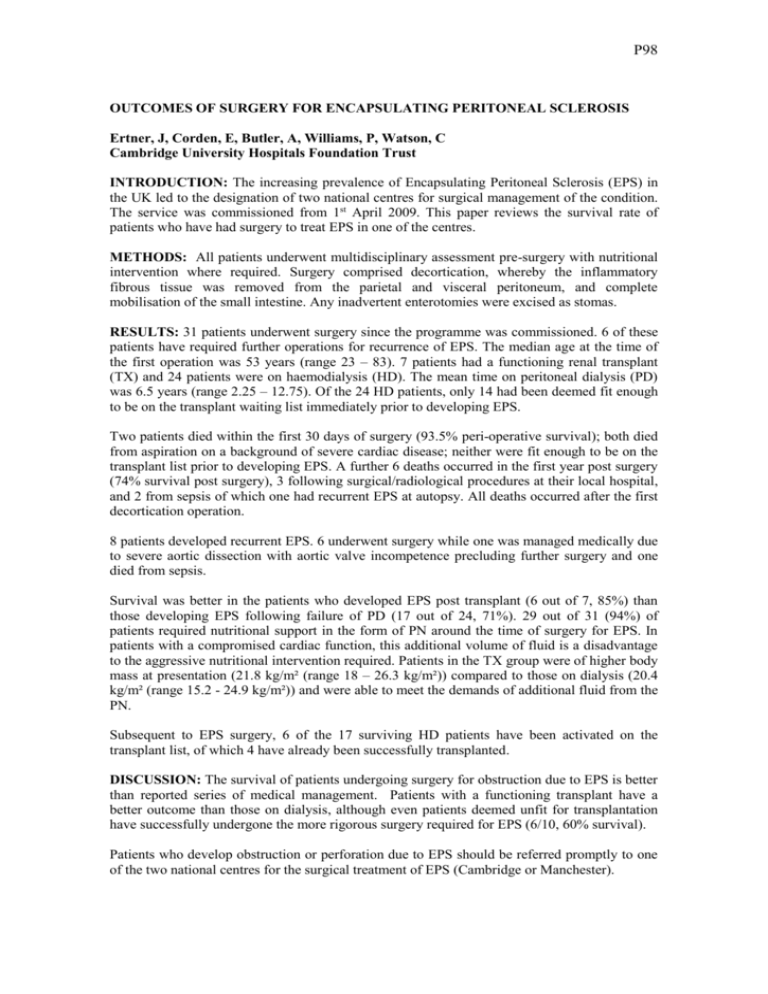
P98 OUTCOMES OF SURGERY FOR ENCAPSULATING PERITONEAL SCLEROSIS Ertner, J, Corden, E, Butler, A, Williams, P, Watson, C Cambridge University Hospitals Foundation Trust INTRODUCTION: The increasing prevalence of Encapsulating Peritoneal Sclerosis (EPS) in the UK led to the designation of two national centres for surgical management of the condition. The service was commissioned from 1st April 2009. This paper reviews the survival rate of patients who have had surgery to treat EPS in one of the centres. METHODS: All patients underwent multidisciplinary assessment pre-surgery with nutritional intervention where required. Surgery comprised decortication, whereby the inflammatory fibrous tissue was removed from the parietal and visceral peritoneum, and complete mobilisation of the small intestine. Any inadvertent enterotomies were excised as stomas. RESULTS: 31 patients underwent surgery since the programme was commissioned. 6 of these patients have required further operations for recurrence of EPS. The median age at the time of the first operation was 53 years (range 23 – 83). 7 patients had a functioning renal transplant (TX) and 24 patients were on haemodialysis (HD). The mean time on peritoneal dialysis (PD) was 6.5 years (range 2.25 – 12.75). Of the 24 HD patients, only 14 had been deemed fit enough to be on the transplant waiting list immediately prior to developing EPS. Two patients died within the first 30 days of surgery (93.5% peri-operative survival); both died from aspiration on a background of severe cardiac disease; neither were fit enough to be on the transplant list prior to developing EPS. A further 6 deaths occurred in the first year post surgery (74% survival post surgery), 3 following surgical/radiological procedures at their local hospital, and 2 from sepsis of which one had recurrent EPS at autopsy. All deaths occurred after the first decortication operation. 8 patients developed recurrent EPS. 6 underwent surgery while one was managed medically due to severe aortic dissection with aortic valve incompetence precluding further surgery and one died from sepsis. Survival was better in the patients who developed EPS post transplant (6 out of 7, 85%) than those developing EPS following failure of PD (17 out of 24, 71%). 29 out of 31 (94%) of patients required nutritional support in the form of PN around the time of surgery for EPS. In patients with a compromised cardiac function, this additional volume of fluid is a disadvantage to the aggressive nutritional intervention required. Patients in the TX group were of higher body mass at presentation (21.8 kg/m² (range 18 – 26.3 kg/m²)) compared to those on dialysis (20.4 kg/m² (range 15.2 - 24.9 kg/m²)) and were able to meet the demands of additional fluid from the PN. Subsequent to EPS surgery, 6 of the 17 surviving HD patients have been activated on the transplant list, of which 4 have already been successfully transplanted. DISCUSSION: The survival of patients undergoing surgery for obstruction due to EPS is better than reported series of medical management. Patients with a functioning transplant have a better outcome than those on dialysis, although even patients deemed unfit for transplantation have successfully undergone the more rigorous surgery required for EPS (6/10, 60% survival). Patients who develop obstruction or perforation due to EPS should be referred promptly to one of the two national centres for the surgical treatment of EPS (Cambridge or Manchester).