DEPARTMENT OF RADIOLOGY
advertisement

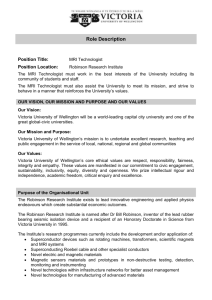
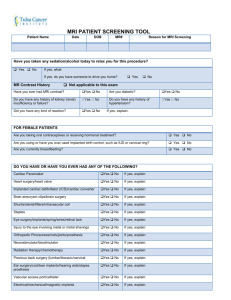
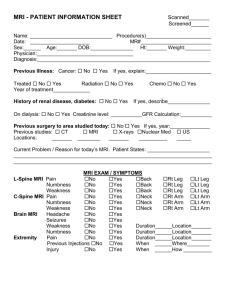
POLICY NO.:A109 APPROVED DATE:Nov. 22, 2005 EFFECTIVE DATE: Nov. 22, 2005 REVIEWED DATE: Nov. 22, 2005 MRI DEPARTMENT OF RADIOLOGY SUBJECT: MRI Hospital Safety Plan I. Mission: Provide a MRI environment for VCU employees, patients and visitors while providing the highest quality MRI services. II. Goal: Establish a MRI Educational program, which provides safety training for VCU Employees, patients and visitors. III. Objectives: 1) Identify and codify those elements, which are necessary for the safest possible MRI environment while ensuring the highest quality MRI Imaging services. a) Site Access Restrictions – the MR suite is conceptually divided into 4 zones 1) Zone 1 – this region includes all areas freely accessible to the general public. Zone 1 is typically outside the MR environment. 2) Zone 2 – this is the area between the publicly accessible, uncontrolled Zone 1 and the strictly controlled Zones 3 and 4. Access to Zone 2 will be restricted by card swipe. 3) Zone 3 – this area is physically restricted from general public access by some sort of locking system. 4) Zone 4 – the MR scanner room itself. b) Identify personnel 1) MR Personnel a) Level 1 – those who have passed minimal safety education efforts to ensure their own safety as they work within Zone III, henceforth referred to as level 1 MR Personnel. Examples of level 1 MR Personnel are: 1) Radiologist (not participating in MRI studies) 2) Radiology Residents 3) Level 1 personnel competency testing a) View Video b) Self directed MRI Safety competency test b) Level 2 – those, who have been extensively trained, educated, tested and demonstrated competency in the broader aspects of MR safety issues. Examples of level 2 MR Personnel are: 1) MR Technologist 2) Anesthesiologist 3) CRNA 4) MR Radiologist (radiologist participating in MRI Studies) 5) 6) 7) 8) 2) 3) 4) 5) Radiology Nurses OEM Service Personnel Radiology Research Personnel Level 2 personnel competency testing a) MRI Safety Lecture b) View the Power Point c) Comprehensive MRI Safety competency test 9) All Level 2 will fill out an initial MRI checklist before beginning work in the MRI environment. 10) No Level 2 personnel will be allowed to work in MRI without completing the education process and have demonstrated mastery. Non MR Personnel (VCU) – those who have not complied with MR safety instruction guidelines. a) VCU Employees must have completed EEB b) Zone III & IV access must be accompanied by a Level 2 MR Technologist. Non MR Personnel – all other non-MR personnel wishing to enter Zone III must first past a MR Safety Screening Process. Only Level 2 MR personnel are authorized to perform a MR Safety Screen prior to permitting non-MR personnel into Zone III. a) Non-MR personnel should be under the immediate supervision of Level 2 personnel for the entire duration the Non-MR personnel is in Zone 3 or Zone 4. b) Radiology Registration will hand the MRI patient the MRI checklist for completion at the time of registration. c) Outpatients will be escorted to the MRI waiting area (Zone 2) by Radiology Transport. Radiology Transport will check to make sure that the patient has filled out the MRI checklist before bringing the patient to the MRI waiting area (Zone 2). d) Non-emergent patients should be MR safety screened on site by a minimum of 2 separate individuals. e) Emergent patients and their accompanying non-MR personnel may be screened only once provided level 2 MR personnel perform the screening. No exceptions. f) Any individual undergoing a MR procedure must remove all readily removable metallic personal belongings and devices on or in them. g) All patients and non-MR personnel with a history of potential ferromagnetic foreign object penetration must undergo further investigation prior to being permitted entrance to Zone 3. h) All patients who have a history of orbit trauma by a potential ferromagnetic foreign body for which they sought medical attention are to have their orbits cleared. MR Personnel Screening a) All MR personnel are to undergo a MR-screening process as part of their employment interview to ensure their safety in the MR environment. Device and object screening a) All devices and / or objects will be contraindicated in Zones 3 and 4 unless previously identified in writing to be either MR safe or MR compatible. b) Never assume MR compatibility or safety information about a device if is not clearly documented in writing. 2) Identify Qualifications of MR Technologist a) MR technologist shall be ARRT registered b) MR technologist will be subspecialty MR certified by the ARRT. c) MR technologist shall be trained as level 2 MR personnel during orientation prior to being permitted free access to Zone 3. d) MR technologist shall maintain current BLS certification e) Except for emergent coverage, there will be a minimum of 2 MR technologist or one technologist and one other individual with level 2 designation. 3) Provide relevant data on Pregnancy Related Issues a) Health care practitioner pregnancies 1) Pregnant health care practitioners are permitted to work in and around the MR environment through all stages of their pregnancy. 2) Should avoid remaining in Zone 4 during actual acquisition or scanning. b) Patient pregnancies 1) Pregnant patients can be accepted to undergo MR scans at any stage of pregnancy if the risk-benefits ratio warrants the study be performed if. a) Information requested from the MR study cannot be acquired via nonionizing means. b) MR data needed will potentially affect the care of the patient or fetus during the pregnancy. c) Referring MD does not feel it is prudent to wait until the patient is no longer pregnant. d) MR contrast agents should not be routinely provided to pregnant patients. e) Pregnant patients will sign the MR information sheet once the radiologist or radiology resident has given a thorough explanation. 4) How to deal with Claustrophobia, Anxiety, Sedation, Analgesia, and Anesthesia a) Adult and pediatric patient anxiolysis, sedation, and anesthesia for any reason should follow established American College of Radiology, American Society of Anesthesiologists and JCAHO standards. 5) Dealing with Pediatric MR Safety Concerns a) Sedation and monitoring guidelines 1) Pre-procedural medical history and examination for each patient. 2) Fasting guidelines appropriate for age. 3) MR compatible intra-procedural and post-procedural monitors are available. 4) Uniform training and credentialing for sedation providers. 5) Sedation providers are Level 2 personnel using direct patient observation 6) Resuscitation equipment, including oxygen delivery and suction 7) Uniform system of record keeping and charting 8) Location and protocol for recovery and discharge 9) Quality assurance program that tracks complications and morbidity b) Pediatric MR Screening (checklist) 1) Once with the parent or guardian. 2) If possible once with the child. 3) All personnel accompanying the child should be screened as well. 6) Other Precautions a) Patients with implanted or retained wires in anatomically or functionally sensitive areas will be considered at higher risk, areas included: 1) Myocardium 2) Epicardium 3) Brain 4) Spine b) Auditory Considerations 1) Patients are encouraged to use hearing protection while undergoing MR examinations. c) Thermal concerns 1) Electrical connections should be removed from the patient and not allowed in Zone III or Zone IV. 2) It is important to ensure that the patient’s tissues do not form a conductive loop. 3) Drug delivery patches should be removed d) Cryogen related issues 1) In the event of a “system quench” all personnel and patients should be evacuated from Zones III and IV. IV. Attachments 1) Zone Maps for: a) Main 3 MR Area b) ACC MR Area c) Stony Point MR Area 2) Competency Exam Level 1 Personnel 3) Competency Exam Level 2 Personnel