Neonatal IV Therapy - Emory University Department of Pediatrics
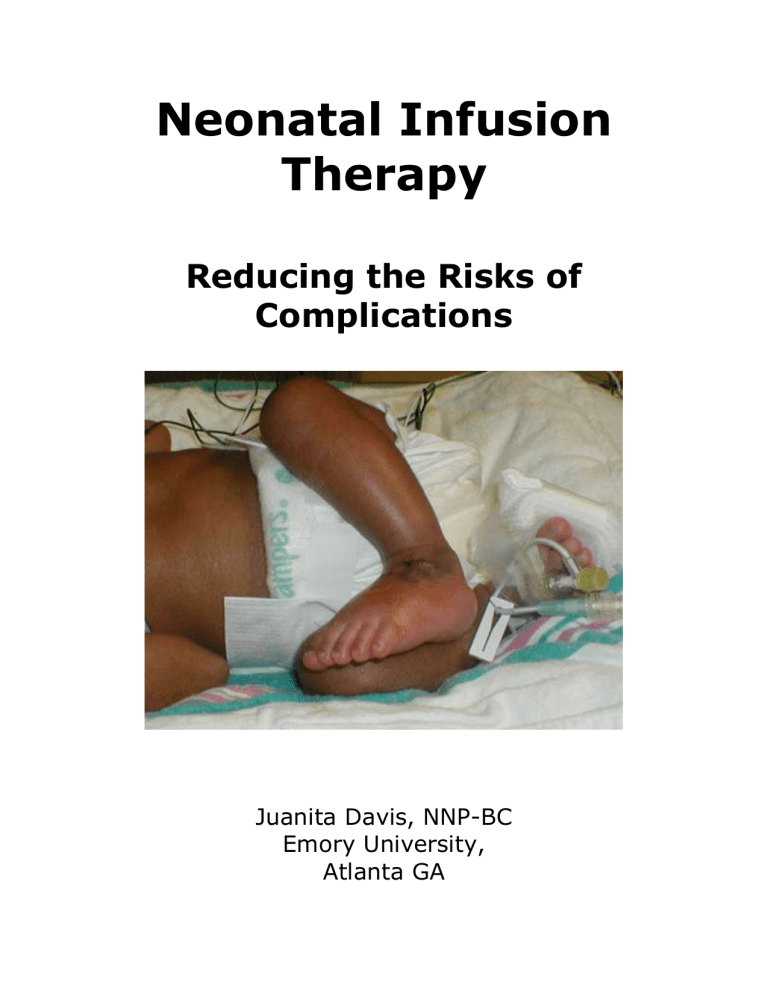
Neonatal Infusion
Therapy
Reducing the Risks of
Complications
Juanita Davis, NNP-BC
Emory University,
Atlanta GA
Neonatal Infusion Therapy
Learning Objectives
Explain rationale for IV site/device selection
Describe interventions to prevent complications
Identify clinical indicators of complications
Describe treatment strategies
Complications of IV Therapy
1) Infiltration: inadvertent administration of nonvesicant solution into surrounding tissue
2) Extravasation: inadvertent administration of vesicant, blistering solution into surrounding tissue
3) Phlebitis: inflammatory response to damage to intimal layer of the vein
4) Leaking: may be isolated or symptom of phlebitis or infiltration
5) Occlusion: formation of thrombus caused by fibrin or coagulated blood products
6) Infection: colonization of the catheter tip by migration of microorganisms from surrounding skin into insertion site, hub contamination, seeding from another site or contamination of the infusate
Peripheral Venous Anatomy
1) Tunica Intima a) Single layer of endothelial cells b) Smooth surface c) Injury exposes subendothelial layer and initiates inflammatory and coagulation processes leading to phlebitis and thrombosis
2) Tunica Media a) Thick layer of elastic and smooth muscle fibers b) Allows vein to elongate and dilate
3) Tunica Adventitia a) Loose connective tissue b) Collagen and elastic fibers allows vein to roll
IV Site Selection
1) Osmolality describes the number of particles suspended in a solution a) Normal serum osmolality: 280 – 295 mOsm/kg b) Hyperosmolar (hypertonic) solution draws fluid from endothelial cells to the serum, causing the cells to shrink c) Hypotonic solutions cause net influx of fluid into the cell, resulting in cell distention and possible rupture d) INS (Infusion Nurses Society) recommends limiting osmolality of peripherally infused substances to 500 mOsm/kg
2) pH based on concentration of hydrogen ions a) normal range 7.35 – 7.45 b) repeated infusion of pH <5 or >9 causes damage to vein
3) Chemical properties of the solution or medication
Prevention of Infection
1) Wash hands
2) Minimize entry into line
3) Maintain closed system
4) Thoroughly clean catheter hub injection port
2
3
Why Fluid Escapes From the Vein
1) Mechanical a) Trauma to tunica intima at time of insertion b) Inadequate stabilization of the catheter or site c) Movement which leads to catheter impinging on vein wall may cause catheter tip to work through vessel wall
2) Obstructed blood flow a) Thrombosis b) Vessel narrowing from scarring, sclerosis c) Pressure on vein from lymphedema
3) Obstructed fluid flow a) Fibrin adheres and accumulated on external surfaces of IV catheter – will eventually encase the device forming a fibrin sheath b) Infused fluid flows retrograde and leaks from insertion site into subcutaneous tissue
4) Inflammatory reaction: Cellular injury triggers release of chemical mediators causing capillary endothelial cells to retract and fluid to leak
Types of Thrombotic Occlusions
1) Intraluminal Thrombus
2) Fibrin Tail
3) Fibrin Sheath
4) Mural Thrombus
Identifying Complications
1) Phlebitis a) Stage I: mild redness above IV site; no pain, edema, hardness or palpable cord b) Stage II: painful IV site with moderate redness, warmth, and/or edema above IV site, no palpable cord or hardness c) Stage III: painful IV site with redness, edema, possible induration, venous cord/hardness palpable at insertion site d) Stage IV: painful IV site, redness, edema, induration with palpable cord extending above insertion site, purulent drainage, frank vein thrombosis
2) Infiltration a) Stage I: pain at IV site, no erythema, no swelling b) Stage II: painful IV site, slight swelling at site, presence of redness, 1-2 second capillary refill distal to site, good pulse distal to site, no blanching c) Stage III: painful IV site, moderate swelling above or below insertion site, blanching, skin cool to touch, 1-2 second capillary refill distal to insertion site, good pulse distal to insertion site d) Stage IV: severe swelling above or below site, blanching, painful IV site, decreased or absent pulse distal to insertion site, capillary refill >4 seconds above or below insertion site, skin cool to touch, skin breakdown or necrosis
PHLEBITIS OR INFILTRATION
Phlebitis
Mild redness above IV site; no pain, edema, hardness or palpable cord
Painful IV site with moderate redness, warmth, and/or edema above IV site, no palpable cord or hardness
STAGE
I
II
Infiltration
Pain at IV site, no erythema, no swelling
Painful IV site, slight swelling at site, presence of redness, 1-2 second capillary refill distal to site, good pulse distal to site, no blanching
4
Painful IV site with redness, edema, possible induration, venous cord/hardness palpable at insertion site
Painful IV site, redness, edema, induration with palpable cord extending above IV insertion site, purulent drainage, frank vein thrombosis which may cause the infusion to stop running
III
IV
Painful IV site, moderate swelling above or below insertion site, blanching, skin cool to touch, 1-2 second capillary refill distal to insertion site, good pulse distal to insertion site
Severe swelling above or below site, blanching, painful IV site, decreased or absent pulse distal to insertion site, capillary refill >4 seconds above or below insertion site, skin cool to touch, skin breakdown or necrosis
If phlebitis or infiltration is identified, perform the following actions based on the assigned
Stage. Do not apply heat to the site of an infiltration. Heat can lead to maceration, necrosis, or rapid movement of the drug into the tissue, expanding the infiltration even further. The use of heat should specifically be avoided with hyaluronidase.
STAGE I: Continue assessments at least hourly and consider initiating alternate site.
STAGE II: Stop the infusion immediately.
Discontinue the IV catheter and initiate an alternate site.
Avoid tape or pressure to site for at least 24 hours or until site is healed.
Document effectiveness of intervention at least every 12 hours until signs of complications are resolved.
STAGE III:
Stop the infusion immediately
Attempt to aspirate offending solution if infiltrated.
Notify the physician/nurse practitioner.
Elevate the extremity for 24 hours.
Avoid tape or pressure to site until healed.
If phlebitis present without infiltrate, apply warm moist packs for 20 minutes every 6 hours until symptoms resolve.
Administer antidote as indicated (requires MD order)
Inform parents of findings and plan of care.
Report event to Risk Management.
Document effectiveness of intervention each shift until complications resolved.
STAGE IV:
Stop the infusion immediately.
Attempt to aspirate offending solution if infiltrated.
Notify the physician/nurse practitioner.
Elevate the extremity for 24 hours.
Avoid tape or pressure to site until healed.
If phlebitis present without infiltrate, apply warm moist packs for 20 minutes every 6 hours until symptoms resolve.
If purulent drainage present, culture drainage at insertion site, culture cannula tip.
Administer antidote as indicated (requires MD order)
Inform parents of findings and plan of care.
Report event to Risk Management.
Document effectiveness of intervention each shift until complications resolve.
5
Aspiration
EMERGENCY MEASURES
1)
2) Antidotes a)
H
yaluronidase is indicated for high osmotic solutions and other miscellaneous drugs such as calcium, penicillin, methicillin, nafcillin, oxacillin, potassium chloride, vancomycin, total parenteral nutrition, blood, and high dextrose solutions. This antidote modifies the permeability of the connective tissue to enhance the distribution and absorption of the infiltrated solutions. It is most effective if administered within 1 to 2 hours, but may be administered up to 24 hours after the event.
b) Phentolamine is indicated for use with vasopressive drugs such as dopamine, norepinephrine, epinephrine, and dobutamine. Phentolamine is an alpha-adrenergic blocking agent that decreases local vasoconstriction and ischemia. It is most effective if administered within 12 hours. Dosages are not well established for neonates and are contraindicated for premature infants due to the potential for excessive vasodilation, hypotension or tachycardia.
c) Corticosteroids have an anti-inflammatory effect. The most commonly used is hydrocortisone sodium succinate.
d) Glycerol trinitrate (topical nitroglycerin) promotes local vasodilation to improve perfusion to affected area. e) If the PIV is left in and an antidote is to be administered, withdraw the PIV 1-2 mm to
4) avoid direct IV antidote administration. f) No antidote recommendations are published for phenytoin infiltrates.
3) Saline washout
5)
Liposuction – requires local or general anesthesia
Gault procedure – combination of instillation of hyaluronidase followed by saline flush out procedure and gentle liposuction of surrounding area
6) Elevation.
Principles of Wound Care
1) Normal wound healing requires proper circulation, nutrition, immune status and avoidance of negative mechanical forces a) Process usually takes 3 -14 days b) Three phases: i) Inflammation ii) Proliferation iii) Remodeling with wound contraction
2) Moisture and occlusion a) Wounds heal twice as rapidly when covered with moisture-retentive occlusive dressings b) Excessively dry wound healing environments cause further tissue death c) Occlusive dressings decrease infection rates d) Overhydrated, macerated tissue has a tendency to break down, delay wound healing
3) Bacterial colonization versus infection a) Colonization may hasten wound healing by increasing wound bed perfusion b) Wounds become clinically infected when host defenses are overwhelmed
4) Debridement: Process of removing slough, eschar, exudate, bacterial biofilms, and callus from wound bed
6
Type
Surgical
Chemical (enzymatic debridement);
Enzymatic removal of debris
(fibrinolysis/deoxyribonuclease
“elase”; collagenase)
Autolytic
Types of Debridement
Advantages
Generally definitive removal of eschar
Facilitate softening of eschar tissue and aids clearing of debris from wound
Disadvantages
General anesthesia
Unknown
Allows body to use natural process; noninvasive
May take longer
Topical
Bacitracin
Silver sulfadiazine
Topicals and Irrigants for IV Extravasation Wound Care
Uses Disadvantages
Gram-positive organisms
Effective for gram-negative organisms
May promote Gram-negative bacteria
Increased risk of kernicterus owing to sulfur competing with bilirubin; agranulocytosis; cytotoxicity to fibroblasts
Aquaphor Superficial wounds to provide a moist wound environment
Amorphous hydrogels Used extensively for treatment of sloughy or necrotic lesions where they are believed to facilitate autodebridement of the wound by rehydrating slough and enabling autolysis to take place at an enhanced rate
Product
Gauzes
Films
Advantages
Inexpensive
Accessible
Considered safe and preferred emollient
Unknown; limited evidence from case reports
Summary of Basic Wound Dressings
Disadvantages Indications
Moisture-retentive
Transparent
Semiocclusive
Protects wound from contamination
Drying
Poor Barrier
No absorption
Fluid trapping
Skin stripping
Packing deep wounds
Wounds with minimal exudate
Secondary dressing
Comment
Change every 12-24 hours
Can leave in place up to 7 days or until fluid leaks
Hydrogels
Hydrocolloids
Alginates and hydrofibers
Foams
Moisture-retentive
Nontraumatic removal
Pain relief
Long wear-time
Absorbent
Occlusive
Protects wound from contamination
Highly absorbent
Hemostatic
Absorbent
Thermal insulation
Occlusive
May over hydrate
Opaque
Fluid trapping
Skin stripping
Malodorous discharge
Fibrous debris
Lateral wicking
(alginates only)
Opaque
Malodorous discharge
Dry wounds
Painful wound
Wounds with light to moderate exudate
Wounds with moderate to heavy exudate
Mild hemostasis
Wounds with light to moderate exudate
Change every 1-3 days
Can leave in place up to 7 days or until fluid leaks
Can leave in place until soaked with exudate
Change every 3 days
7
Intravenous Infiltration
Inadvertent administration of a solution or medication into surrounding tissue.
1) Prevention of IV Infiltration a) Use small enough catheter to avoid restriction of blood flow b) Evaluate suitability of all infusates for peripheral administration by assessing osmolality, pH, and chemical composition c) Avoid areas of flexion or those that are difficult to immobilize d) Support extremity with arm or foot board to prevent catheter motion or dislodgement e) Secure to avoid catheter movement but avoid restrictive dressing f) Avoid repeated use of a vein g) Cover insertion site with transparent dressing or tape h) Inspect insertion site and surround tissue every hour i) Tape loosely over elbow or knee to prevent obstruction of venous return
2) Treating Intravenous Infiltration a) Stop infusion if any signs of infiltration occur i) Swelling, pain at site, coolness, leakage, erythema ii) Blanching, blisters, discoloration, skin sloughing b) Assess degree of injury c) Elevate the site of affected extremity d) Administer hyaluronidase (Wydase) e) Make multiple puncture holes over the area of greatest swelling and let infiltrated fluid leak out f) If infiltrated fluid contains Dopamine, use phentolamine (Regitine) g) Treat tissue injury with saline irrigation, ointments, or other dressings as indicated
IV INFILTRATE WOUND CARE
1.
Wound care principles include: remove necrotic tissue; eradicate infection; absorb excess exudate; obliterate dead space; maintain a moist wound surface; insulate the wound; and protect the wound from further trauma or bacteria.
2.
If skin is intact (even if blistering), cleanse with sterile normal saline. Gently pat dry with sterile gauze, a.
Cover wound with sterile semi-permeable transparent dressing. b.
Leave transparent dressing in place as long as skin covering wound is intact or until healed.
3.
If skin is broken, cleanse with sterile normal saline using syringe with IV catheter attached to gently irrigate wound. a.
Apply hydrogel to wound, not surrounding skin. Hydrogels enhance epithelialization without reinjuring tissue. A secondary dressing is recommended to maintain the moisture b.
Cover with non-stick (Telfa) gauze, then wrap with sterile gauze. Do not apply tape to skin. c.
Change dressing and re-apply hydrogel every 6 - 12 hours until edges of wound appear pink. d.
Once wound edges appear pink and wound bed has a red, moist, beefy appearance, cover with sterile semi permeable transparent dressing as above.
4.
If wound bed is covered with eschar (hard, black, leathery tissue) cover with sterile semi permeable transparent dressing and leave in place to soften eschar. a.
Once eschar is completely moist, or every 5-7 days, gently remove transparent dressing. b.
Cleanse wound with sterile normal saline and proceed as above, depending upon condition of wound edges.
5.
Consider consultation with enterostomal therapist.
8
References
Bardot, C. J., Magalon, G. (2001). Emergency Treatment of Accidental Infusion Leakage in the
Newborn: Report of 14 Cases. British Journal of Plastic Surgery, (54), 396-399.
Beauman, S. S., & Swanson, A. (2006). Neonatal Infusion Therapy: Preventing Complications and Improving Outcomes. Newborn and Infant Nursing Reviews, 6(4), 193-210.
Brown, A. S., Hoelzer, D. J., & Piercy, S. A. (1979). Skin Necrosis From Extravasation of
Intravenous Fluids in Children. Plastic & Reconstructive Surgery, 6(2), 145-150.
Cisler-Cahill, L. (2006). A Protocol for the Use of Amorphous Hydrogel to Support Wound
Healing in Neonatal Patients: An Adjunct to Nursing Skin Care. Neonatal Network,
25(4), 267-273.
Clifton-Koeppel, R. (2006). Wound Care After Peripheral Intravenous Extravasation: What Is the Evidence? Newborn and Infant Nursing Reviews, 6(4), 202-211.
Fleming, L. & Chan, J. S. L. (1993). A Pediatric Protocol for Management of Extravasation
Injuries. Pediatric Nursing, 19 (4), 355-358.
Fonder, M. A., Lazarus, G. S., Cowan, D. A., Aronson-Cook, B., Kohli, A. R., & Mamelak, A. J.
(2008) Treating the Chronic Wound: A Practical Approach to the Care of Nonhealing
Wounds and Wound Care Dressings. Journal of the American Academy of
Dermatology, 58(2), 185-206.
Frey, A. M., & Schears, G. J. (2006). Why Are We Stuck on Tape and Suture? Journal of
Infusion Nursing, 29(1), 34-38.
Garland, J. S., Dunne, W. M., Havens, P., Hintermeyer, M., Bozzette, M. A., Wincek, J.,
Bromberger, T., & Seavers, M. (1992). Peripheral Intravenous Catheter Complications in Critically Ill Children: A Prospective Study. Pediatrics, 89 (6), 1145-1150.
Hadaway, L, C. (2000). IV Infiltration. Not Just a Peripheral Problem. Nursing Management,
(November), 26-31.
Harris, P. A., Bradley, S., & Moss, A. L. (2001). Limiting the Damage of Iatrogenic
Extravasation Injury in Neonates. Plastic & Reconstructive Surgery, 107(3), 893-894.
Heckler, F. R. (1989). Current Thoughts on Extravasation Injuries. Clinics in Plastic Surgery.
16(3), 557-563.3.
Hermansen, M. C., & Hermansen, M. G. (2005). Intravascular Catheter Complications in the
Neonatal Intensive Care Unit. Clinics in Perinatology, 32, 141-156.
Olsen, C, L., Hahn, J, F., Goldberg, M., & Tomaselli, N. (2002). Wounds: Nursing Care and
Product Selection – Parts I & II. Online Education/CE Self-Study Modules.
Infusion Nurses Society. Policies and Procedures for Infusion Nursing. Cambridge, MA:
Infusion Nurses Society; 2000.
Maki, D. G. (1989). Pathogenesis, Prevention, and Management of Infections Due to
Intravascular Devices Used for Infusion Therapy. In A. L. Bisno & F. A. Waldvogel
(Eds.). Infections Associated with Indwelling Medical Devices (pp. 161-177).
Washington, DC: American Society for Microbiology.
Montgomery, L. A., Budreau, G. K. (1996). Implementing a Clinical Practice Guideline to
Improve Pediatric Intravenous Infiltration Outcomes. AACN Clinical Issues, 7(3), 411-
424.
Montgomery, L. A., Hanrahan, K., Kottman, K., Otto, A., Barrett, T., & Hermiston, B. (1999).
Guideline for IV Infiltrations in Pediatric Patients. Pediatric Nursing, 25(2).
National Association of Neonatal Nurses (NANN). 1997. Neonatal Skin Care Guidelines for
Practice.
O’Connor, K. (2006). Vascular Issues. Newborn and Infant Nursing Reviews, 6(4), 245-246.
Pettit, J. (2003). Assessment of the Infant with a Peripheral Intravenous Device. Advances in
Neonatal Care, 3(5):230-240.
Perucca, R., Micek, J. (1993). Treatment of Infusion-Related Phlebitis: Review and Nursing
Protocol. Journal of Intravenous Nursing, 16(5), 282-286.
Sawatzky-Dickson, D., Bodnaryke, K. (2006). Neonatal Intravenous Extravasation Injuries:
Evaluation of a Wound Care Protocol. Neonatal Network, (25)1:13-19.
Subhani, M., Sridhar, S., DeCristofaro, J.D., (2001). Phentolamine Use in a Neonate for the
Prevention of Dermal Necrosis Caused by Dopamine: A Case Report. Journal of
Perinatology, 21:324-326.
Websites http://www.worldwidewounds.com/1997/october/Neonates/NeonatePaper.html