outline26418
advertisement

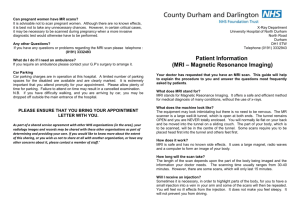
I. This interactive presentation will use clinical cases involving neuroimaging to emphasize important aspects of neuroimaging. A. Pathology of the orbit, visual pathway, paranasal sinuses, cranial nerve pathways, and cranial vascular system will be covered in a case based format: 1. Conditions: a) Idiopathic intracranial hypertension b) Papilledema c) Demyelinating optic neuritis d) Optic neuritis secondary to systemic inflammation and infection e) Optic atrophy f) Congenital abnormalities g) Tumors h) Thyroid eye disease i) Idiopathic inflammation of the visual pathway j) Aneurysm k) Ophthalmoplegic migraine l) Sinus disease m) Carotid occlusion 2. Localization of pathology causing the following symptoms: visual loss, visual field defects, diplopia, nystagmus, pupil and eyelid abnormalities, and headaches. 3. Interesting incidental findings II. The following points will be emphasized using the cases listed above: A. Neuroimaging techniques 1. Computed axial tomography (CT) a) Indications (1) Bone evaluation (2) Fresh blood (3) Paranasal sinuses (4) Detection of calcification of a lesion (5) Extraocular muscle evaluation b) Strengths (1) Lower cost (2) More rapid (3) Can image those with implanted or retained metal objects c) Bone window, soft tissue window d) Axial, coronal, and reconstructions (1) Direct imaging provides improved resolution (2) Perform reconstructions if the patient has limited mobility, you need to reduce the scan time, or to decreases dispersion artifact e) Use of contrast agents (1) Iodine based material (2) Allows evaluation of the blood-brain barrier (3) Relative contraindications (a) Renal impairment (check BUN and creatinine levels) (b) Allergic reaction to iodine (can be given short term allergy meds) 2. Magnetic resonance imaging (MRI) a) Indications and strengths (1) Evaluation of soft tissue (2) Tumors (3) Inflammation (4) White matter disease (5) Pituitary gland lesions (6) Cranial nerve lesions b) Use of contrast agent (1) Gadolinium (2) Enhances structures with incomplete or absent blood-brain barrier (3) Can further improve contrast between normal and pathological tissue (4) Normally enhancing anatomy: cavernous sinus, pituitary gland, infundibulum, sinus mucosa (5) Normal cerebral and orbital vessels with rapidly flowing blood will not enhance 3. CT angiography a) Indications and strengths (1) Cerebral aneurysms 4. Magnetic resonance angiography (MRA) a) Indications and strengths (1) No need for injection of contrast media or ionizing radiation (2) Visualize the aneurysm as well as the vicinity of the aneurysm (3) Carotid occlusion (4) Vascularity of lesions 5. Magnetic resonance venography (MRV) a) Indications and strengths (1) Venous sinus thrombosis B. Interpreting neuroimaging studies 1. Determination of pulse sequence and scan characteristics a) Appearance of the CSF (bright on T2, dark on T1) b) Intensity of the vitreous (bright on T2, dark on T1) c) Differentiation of white and gray matter in the cerebrum (white matter darker than gray matter on T2, white matter lighter than gray matter on T1) d) Orbital fat (dark = fat suppression) e) Contrast enhanced scan: small blood vessels, nasal mucosa, or EOM enhancement f) FLAIR images: CSF and vitreous are dark, but the white matter darker than gray matter 2. Appearance of normal anatomy, variations of normal, and pathology a) CT (1) Brightest areas: bone (2) Darkest areas: air (3) Hyperdense: sinus secretions, acute hemorrhage, calcification (4) Hypodense: edema, necrosis b) MRI (1) Tightly bound hydrogen does not produce a signal (bone cortex) (2) Rapidly flowing blood does not produce a signal (3) Unbound hydrogen produces a significant signal 3. Abnormal anatomy is identified by adequate knowledge of normal anatomy a) b) c) d) e) f) g) h) i) Pathology typically increases the water content in tissue Pathological process often disturb the blood brain barrier Need to localize patients signs and symptoms Visual pathway Cranial nerves Ventricles and venous sinuses Vasculature Paranasal sinuses Sellar region and cavernous sinus C. Ordering neuroimaging studies 1. Quality/type of image a) MRI vs. CT b) T1, T2, FLAIR, fat suppression, DWI sequences (1) T1: clearest anatomic delineation (2) T2: most sensitive for detecting pathology (3) Fat suppression is useful in orbital imaging (4) FLAIR: good for demyelinating disease (5) DWI: sensitive for cerebral infarction c) Axial, sagittal, coronal 2. Area of interest a) Orbit b) Brain imaging 3. Use of contrast enhancement a) Should be used routinely for cases of vision loss 4. Scan thickness a) CT (1) Thinner scan improve resolution but increase radiation dose (2) Orbital scans: 3 mm slice thickness (3) Optic nerve and canal: 1.5 mm slice thickness (4) Intracranial scan: 5-10 mm slice thickness b) MRI (1) Orbital scans: 3mm slice thickness (2) Intracranial imaging: 3-5 mm slice thickness 5. Clinical information needed 6. Urgency of scanning a) Bilateral disc swelling (same day MRI and MRV) b) Third nerve palsy (same day MRI and MRA) 7. Other considerations: urgency, scan time, and patient cooperation 8. Patient education a) Assure no contraindications b) No heavy makeup D. Contraindications to performing neuroimaging 1. Contraindications of CT a) Radiation exposure (pregnant women) 2. Contraindication for MRI a) Ferromagnetic metallic devices: vascular clips, cardiac pacemakers, prosthetic devices, and retained foreign bodies b) Relative contraindications: claustrophobia, pregnancy