Leprosy
advertisement

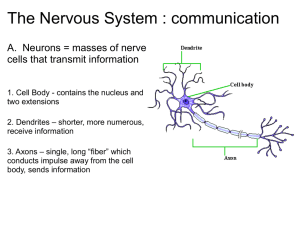
Leprosy (Hansen’s Disease) A chronic granulomatous disease, caused by Mycobacterium leprae, which affects principally the skin and peripheral nervous system. Armauer Hansen discovered M leprae in Norway in 1873. Animal reservoirs of leprosy have been found in 3 species: 9-banded armadillos, chimpanzees, and mangabey monkeys. Pathophysiology M leprae is an obligate intracellular acid-fast bacillus with a unique ability to enter nerves. Predilection for cooler areas. Most affected areas: 1) superficial peripheral nerves 2) mucous membranes of the upper respiratory tract 3) anterior chamber of the eyes 4) testes. Tissue damage is caused : 1) degree to which cell-mediated immunity is expressed 2) the extent of bacillary spread and multiplication 3) appearance of tissue-damaging immunologic complications (ie, lepra reactions) 4) development of nerve damage and its sequelae. Target is Schwann cell. Macrophages and lymphocytes invade the nerve when infection is recognised – forming granuloma and fibrosis. Nerve becomes enlarged – a pathognomic sign of leprosy Earliest change observed in leprematous leprosy is presence of bacilli in Schwann cells. Maximum concentration of bacilli are found 1) fine dermal nerves 2) superficial nerve trunks There is always nerve damage. Nerve lesions are due to 1) infection of nerve(early) 2) immune reactions even after bacteria is no longer present (late) Where skin lesions are present, underlying dermal nerves are always infected. 30% of fibers need to be destroyed before sensory change is detected. If a skin lesion is found to be insensitive or an adjacent subcutaneous nerve is visible or palpable, leprosy can confidently be suspected. Saddle nose deformity may occur with involvement over nose. Characteristic alopecia of lateral brow Clinical Course Profound loss of sensation (pain and temperature) allows uncontrolled trauma and infection With repeated tissue necrosis, self debridement and trauma – fingers and toes may shorten to form mitten hands and feet. 90% of people exposed are immune to the bacilli The incubation period ranges from 6 months to 40 years or longer. The average incubation period is 2-3 years Cardinal signs: 1. anesthesia of a skin lesion in the distribution of a peripheral nerve 2. thickened nerves at the site of predilection 3. typical skin lesions 4. slit skin smears 90% of patient present with numbness first, sometimes years before the skin lesions appear. Temperature is the first sensation that is lost, followed by light touch, then pain, and finally deep pressure. These losses are especially apparent in the hands and feet. Common sites of nerve involvement: 1) ulnar nerve at elbow 2) median nerve wrist 3) superficial branch radial nerve wrist Peripheral nerve paralysis occurs in 20% to 25% of patients with Hansen’s disease. Ulnar nerve responsible for 50% of hand deformities followed by combined high ulnar/low median, then low ulnar/low median. Radial nerve palsy rare (1-2%) o Ulnar nerve may be involved at elbow or wrist o Median nerve usually at wrist (low) o Radial nerve usually as it lies in the spiral groove According to Brand’s experience “the paralysis is predictable. It affects only certain nerves and these nerves only at certain anatomical levels. Therefore, when a hand is assessed at any stage in the disease, one may say with some confidence that though certain muscles may become paralyzed later, certain others will almost certainly never become paralyzed, however far the infection progresses.” Median/ulnar nerve palsy Classification Clinical Features or Test TT Form LL Form Skin lesions Number Sensation Surface Hair growth in lesions One or few Absent Dry or scaly Absent Numerous Not affected Shiny Not affected Nerve enlargement Cutaneous nerves Larger peripheral nerves Common Very rare Not enlarged Symmetrically enlarged ENL reaction Does not occur Common Lepromin test Strongly positive Negative Bacillary index 0 5 or 6 Skin histology Granuloma cell Lymphocytes Dermal nerves Epithelioid +++ Destroyed Foamy histiocyte +/Easily visible Prognosis Good Poor Patients with negative smears at all sites are grouped as having paucibacillary (PB) leprosy, whereas those showing positive smears at any site are grouped as having multibacillary (MB) leprosy. Persons with more than 5 patches and involvement of more than 1 nerve trunk are also considered to have MB leprosy. Symmetrical skin lesions tend be MB. The PB group includes TT and BT types, whereas the MB group includes BB, BL, and LL. The disease does not remain static but evolves spontaneously or in response to therapy. Transition toward the TT pole is referred to as upgrading (and may lead to a reversal or type I reaction) and transition toward the LL pole as downgrading (leading to type II reaction or erythema nodosum leprosum [ENL]). Unlike the other types of leprosy, LL cannot convert back to the less severe borderline or tuberculoid types of disease. Investigations 1) Lepromin test a. a guide to the cell-mediated immunity of the individual. b. a suspension of killed M leprae obtained from infected human or armadillo tissue is injected intradermally – measure size of wheal 2) Slit Skin Smear a. An incision is made in the skin, and the scalpel blade is used to scrape the cut edges to obtain fluid from a lesion. b. Dorsum of fingers = most sensitive 3) Skin biopsy a. bacterial index (BI) – number of bacilli in dermis. 4) Nerve biopsy 5) Histamine testing a. This test is used to diagnose postganglionic nerve injury. b. Histamine diphosphate is dropped on normal skin and affected skin, and a pinprick is made through each site. The site forms wheal on normal skin but not where nerve damage exists. 6) Methacholine sweat testing a. Demonstrates the absence of sweating in leprous lesions. b. Useful in dark-skinned patients in whom the flare with the histamine test cannot be seen.