An audit to evaluate the use of post operative pain guidelines on
advertisement
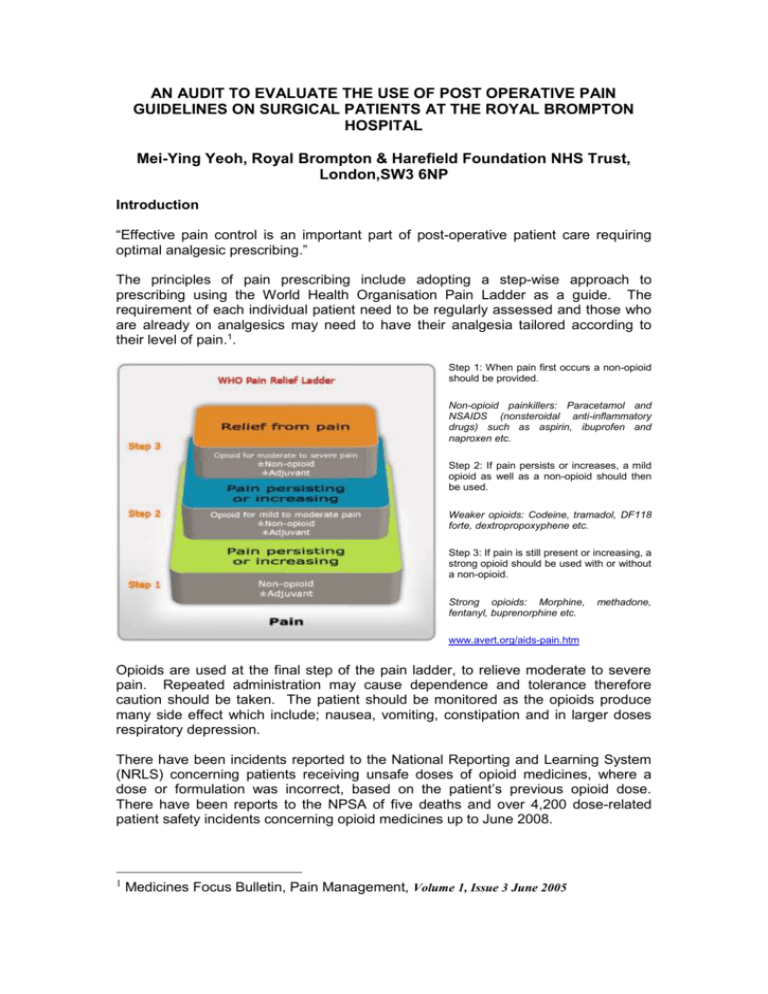
AN AUDIT TO EVALUATE THE USE OF POST OPERATIVE PAIN GUIDELINES ON SURGICAL PATIENTS AT THE ROYAL BROMPTON HOSPITAL Mei-Ying Yeoh, Royal Brompton & Harefield Foundation NHS Trust, London,SW3 6NP Introduction “Effective pain control is an important part of post-operative patient care requiring optimal analgesic prescribing.” The principles of pain prescribing include adopting a step-wise approach to prescribing using the World Health Organisation Pain Ladder as a guide. The requirement of each individual patient need to be regularly assessed and those who are already on analgesics may need to have their analgesia tailored according to their level of pain.1. Step 1: When pain first occurs a non-opioid should be provided. Non-opioid painkillers: Paracetamol and NSAIDS (nonsteroidal anti-inflammatory drugs) such as aspirin, ibuprofen and naproxen etc. Step 2: If pain persists or increases, a mild opioid as well as a non-opioid should then be used. Weaker opioids: Codeine, tramadol, DF118 forte, dextropropoxyphene etc. Step 3: If pain is still present or increasing, a strong opioid should be used with or without a non-opioid. Strong opioids: Morphine, fentanyl, buprenorphine etc. methadone, www.avert.org/aids-pain.htm Opioids are used at the final step of the pain ladder, to relieve moderate to severe pain. Repeated administration may cause dependence and tolerance therefore caution should be taken. The patient should be monitored as the opioids produce many side effect which include; nausea, vomiting, constipation and in larger doses respiratory depression. There have been incidents reported to the National Reporting and Learning System (NRLS) concerning patients receiving unsafe doses of opioid medicines, where a dose or formulation was incorrect, based on the patient’s previous opioid dose. There have been reports to the NPSA of five deaths and over 4,200 dose-related patient safety incidents concerning opioid medicines up to June 2008. 1 Medicines Focus Bulletin, Pain Management, Volume 1, Issue 3 June 2005 Guidance was issued from the NPSA for prescribing, dispensing or administering opioid medicines (in anything other than acute emergencies). The healthcare practitioner concerned, or their clinical supervisor, should follow these steps: • Confirmation of any recent opioid dose, including the formulation, frequency of administration and any other analgesic medicines prescribed for the patient. There are various ways this can be done for example through discussion with the patient or their representative the prescriber or through medication records. • With regards to strong opioids, ensuring that the calculated dose is safe for the patient; oral morphine or oxycodone in adult patients, not normally more than 50% higher than the previous dose. Particular care should be taken where a dose increase is intended. • Ensuring that the Physician is familiar with the following characteristics of that medicine and formulation: usual starting dose, frequency of administration, standard dosing increments, symptoms of overdose, common side effects.2 This guidance is reflected through the Pain Management Service (PMS) at the Royal Brompton & Harefield Foundation Trust who have implemented their own guidelines: Guidelines for the Prescribing & Administration of Strong Opioids in Opioid Naive Adults (revised December 2008). These guidelines should be adhered to in both cardiac and thoracic patients post surgery. Objectives To asses if the Trust’s guidelines for the Prescribing & Administration of Strong Opioids in Opioid Naive Adults are being adhered to. Standards 100% of patients should be prescribed analgesia according to the pain guidelines unless contraindicated. METHODOLOGY 33 patients were audited over a two week period between the 26th October and the 6th November from the surgical wards (Princess Alexandra and Elizabeth ward). Data was collected via drug charts; medical records integrated patient pathways (ICP) and TTOs. In particular the data collection focused on cardiac and thoracic surgery patients, the types of surgery that was performed and the analgesic prescribed to see if there was a correlation The data collection tool incorporated pre-op analgesia, initial post-operative analgesia (e.g PCA/PVB), post op enteral analgesia and discharge analgesia. Results 2 Rapid Response Report, NPSA/2008/RRR05,From reporting to learning 04 July 2008 NHS A total of 33 cardiothoracic surgery procedures were audited, all of which were included in the analysis. Results showed that there was 100% adherence to the guideline. Only 20% of all surgical patients were prescribed a strong opioid medication after surgery, these were all thoracic patients. Fig 1: Flowchart to show results of strong opioid prescribing. Total number of surgical procedures (n=33) Procedures that did not receive opioid analgesics (n=26) Procedures that received opioid analgesics (n=7) Cardiac Surgery (n=0) Thoracic Surgery (n=7) Oramorph (n=5) Oxycontin (n=1) Oxynorm (n=1) 70% of patients given strong opioids were prescribed oramorph 10mg/5ml. The remaining patient was prescribed oxynorm and oxycontin. Discussion Each time a patient was prescribed a strong opioid analgesic there was a valid rationale behind it. In cases where the sequence of steps from the WHO pain ladder was not followed, the strong opioids was commenced following consultation with the Pain Management Service . The reasons behind the non- adherence to the Guidelines for the Prescribing & Administration of Strong Opioids in Opioid Naive Adults included that the patients were not opioid naïve therefore after major surgery a strong opioids was deemed appropriate. The guideline states that oramorph should be used first line when a strong opioids is required. One patient who did not receive oramorph, but was prescribed oxynorm and oxycontin, this was initiated in consultation with the Pain Management Service since the patient was experiencing vomiting and nausea and hallucinations side effects from the oramorph. The 100% adherence was achieved over 2 weeks of auditing, when there was a nonadherence to the WHO pain ladder, the guideline was still adhered too as the Pain Management Service had been consulted before any opioids were prescribed. Recommendations The ward would benefit from a re-audit of a longer period. There was not many procedures that needed strong opioid medication during the audit period therefore this may not be a true reflection of the adherence to the guideline. The audit did not include reasons why non-first line opioids i.e oxynorm or oxycontin were prescribed, this could be looked into in the future. To feed back the results through clinical governance meetings to the surgical directorate and multidisciplinary team to promote the Guidelines for the Prescribing & Administration of Strong Opioids in Opioid Naive Adults to ensure continuing adherence.