Case presentation
advertisement

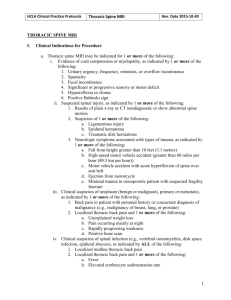
Case of the Month – January 2013. Giant Thoracic Neurofibroma with Spinal Cord Compression and Intrathoracic Extension Marcel Ivanov1, Neil Chiverton2, Jagan Rao3 1 Royal Hallamshire Hospital, Sheffield, UK 2 Northern General Hospital, Sheffield, UK History. A 51 year old lady presented with a six months history of progressive leg weakness and recent slow deterioration. She described this as her “legs giving way” with several recent falls, funny sensation in both of her feet, tingling and feeling of both of her feet cold and numb with some patchy numbness in the lower abdominal area. There were no sphincter problems. No problems with the upper limbs. Questions Where is the presumable pathology o Basal ganglia/motor cortex tumor o Cervical myelopathy o Lumbar spinal canal stenosis o Thoracic myelopathy (correct) What would be the next step? o MRI head and whole spine o Full neurological examination and targeted imaging (correct) o Xray spine Neurological examination Sensory level at T10 with reduced sensation caudally. Brisk reflexes in lower limbs. Plantars neutral, no evidence of clonus, no motor deficit. Normal neurology in the upper limbs with normal reflexes, strength, and sensation. Hoffman negative. Normal cranial nerves examination Past medical history: dyspnoea, patient known with asthma (taking inhalers), otherwise well, no history of trauma The patient was initially referred by the GP to neurology where she was suspected for MS and underwent further investigations including MRI of whole neuraxis. Where is the presumable pathology Was the MRI of whole neuraxis appropriate? What investigations would you recommend? Answers: the lesion is presumably located at the thoracic level: this is concluded from clinical presentation (lower limb problems, normal upper limbs) and neurological examination suggesting spinal cord rather the nerve compression (brisk reflexes, sensory level). The MRI ideally will need to be targeted at the thoracic area (at least in the first stage). MRI of the whole neuraxis although may show the abnormality, it will not be necessarily appropriate. Imaging: MRI neuraxis was arranged by the neurology team who initially assessed the patient. This showed severe spinal cord compression at T7/T8 level caused by a giant mass extending from the left foramina at this level into the spinal canal and into the chest cavity with displacement of the lung and the diameter of approximately 15 cm. 1 Fig.1 MRI thoracic spine demonstrated severe spinal cord compression at T7 level secondary to a large mass extending into the left chest cavity and displacing intrathoracic organs. Fig.2 – Xray chest showing large intrathoracic mass potentially explaining pre-existing patient’s dyspnoea Questions What are the differential diagnosis? 2 What would be the next step? (multiple choices possible) 1. Urgent total surgical excision of the mass 2. Watch and see 3. Biopsy 4. Referral to the oncology 5. Further investigations Answers: Potential differential diagnosis to be considered will be: sarcoma, lung tumor, spine tumor, nerve tumor, aneurismal bone cyst, giant cell tumor of the spine, osteochondroma/blastoma1. The most appropriate steps would be histological diagnosis and staging which will help the surgeon with further management (radical resection versus palliative treatment). The patient had further investigations: CT of the chest, abdomen and pelvis to rule out other abnormalities and for staging – no other lesions identified CT with contrast to identify relationship with other organs CT guided percutaneous biopsy – no malignant features, presumable diagnosis – neurofibroma Fig.3 CT chest, abdomen and pelvis with contrast – 3d reconstruction - demonstrating large intrathoracic mass, its relationships with other organs, spine, bony anatomy. 3 What would be the possible treatment options? 1. Conservative follow-up until patient develops more important neurological deficit 2. Radiotherapy 3. Cyber knife 4. Surgery 5. Send patient to thoracic surgeons Answer: Early surgical excision before installation of neurological deficit would be accepted as gold standard treatment in this case. Although this is a benign slow growing tumor, patient had continuous neurological deterioration over the last 6 months which along with severe spinal cord compression will indicated high risk of paraplegia in the near future if not addressed. What approach would you choose? 1. Posterior laminectomy and spinal cord decompression 2. Anterior transthoracic approach 3. Costotransversectomy 4. Anterior then posterior tumor excision 5. Posterior then anterior tumor excision What would be your arrangements and considerations prior to surgery? Patient underwent initially posterior spinal cord decompression with partial tumor excision followed by the removal of the rest of the tumor using anterior transthoracic approach on the same day in the same surgery. Prior to surgery, the case has been discussed with cardiothoracic and orthopaedic surgeons and a multidisciplinary approach to the patient was arranged. We preferred initially posterior approach as this would allow the spinal cord decompression in the first instance and release tumour attachment from the neural elements, reducing the risk of spinal cord damage and neurological deficit. As the biopsy showed that it was a neurofibroma, we accepted that it could have a “dumbbell” intradural extension with potential risk of CSF leak/adherences to the spinal cord. Another consideration was with regard to potential spinal instability after the surgery: the tumor clearly eroded the pedicle and partially the vertebra, with potential risk of spinal instability especially after transthoracic approach. A decision to do the instrumented spinal fixation after posterior tumor excision was made. During the first part of the procedure a laminectomy was performed, the tumour was microsurgically excised after initial debulking and partially removed (until thoracic cavity was reached). The tumor was arising from the nerve root and extending intradurally. Dura was closed in a watertight fashion. At the end of the first stage posterior spinal instrumented fixation was performed. In the second stage the transthoracic surgeons removed the part from the chest cavity. The tumour was adherent to the parietal pleura and pericardium, however macroscopically total tumor removal was achieved (fig). Thoracic drain was inserted and wound closed. Patient was discharged in one week able to mobilise independently. 4 Fig.4 Completely excised tumor – neurofibroma. Fig. 5 – Immediately postoperative MRI confirming tumor excision and spinal cord decompression. Immediately postoperative changes (blood clot) in the tumor bed are identified. What the postoperative short and long term plan? Immediately postoperatively X-ray of the chest, DVT prophylaxy, physiotherapy, routine X-ray of the spine and an early (in 6-8 weeks) MRI of the spine will need to be arranged to assess the degree of tumor removal As the histopathology showed that this was a neurofibroma, a screening for neurofibromatosis (NF) will need to be arranged. What will you need to check? Early mobilisation will be indicated and a follow-up imaging and appointment will need to be arranged. Conclusion Giant spinal neurofibromas with intrathoracic extension are relatively rare (only few cases described in the literature) and pose multiple surgical challenges (surgical planning, approach, strategy, follow-up etc). The optimal results will be achieved with a multidisciplinary approach. Bibliography 1. Benign tumors of the spine. Thakur NA, Daniels AH, Schiller J, Valdes MA, Czerwein JK, Schiller A, Esmende S, Terek RM. J Am Acad Orthop Surg. 2012 Nov;20(11):715-24. doi: 10.5435/JAAOS-2011-715. 2. Giant neurofibroma of the chest wall. Margaritora S, Galetta D, Cesario A, Granone P. Eur J Cardiothorac Surg. 2002 Feb;21(2):339 3. Giant thoracic neurofibromatosis type 1 with massive intratumoral haemorrhage: a case report. Lessard L, Izadpanah A, Williams HB. J Plast Reconstr Aesthet Surg. 2009 Sep;62(9):e325-9 5