Stiff elbow guidelines
advertisement

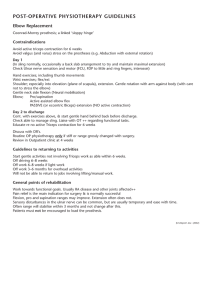
Stiff elbow guidelines Shoulder and elbow service These guidelines have been developed using the Morrey classification of the post-traumatic stiff elbow, current orthopaedic literature, and the clinical experience of our surgical and therapy colleagues. The guidelines are to provide a general overview of the rehabilitation pathway. With all patients referred from our service it is imperative that the patient specific post operative guidelines take precedence. Therapists are expected to develop their own clinical reasoning processes and progress the patient’s rehabilitation in an appropriate manner. We cannot take responsibility for any individual problems that may result from utilising these guidelines particularly as therapists may have a multitude of clinical experiences that differ from our own. Purpose: 1. To progressively restore passive ROM. 2. To introduce AROM elements within a milestone driven framework. 3. To restore functional range of movement within comfortable limits. 4. Ensuring where possible 100 degree functional arc (e.g. 0-100 degrees). Include open and arthroscopic release, manipulation under anaesthetic (MUA), arthrolysis, excision radial head, O.K. procedure (complex). Inpatient post operative protocol Resting backslab +/- drain for 24 hours (longer if medically indicated). CPM (24-48 HRS) to ensure no loss of PROM. Ensure adequate pain control. Monitor neurovascular signs. Maintain elevated resting position (above heart level where possible). Encourage early finger and hand movement (promotes venous drainage). Encourage patient mobility to bathroom and to sit out for meals with arm supported. Once drain removed and wound re-dressed look to start ROM exercises (eccentric triceps into flexion, arm supported at 90 degrees flexion of the shoulder) and active assisted extension. (BE SURE TO MONITOR WOUND INTO FLEXION). Provision of resting extension splint from OT or plaster theatre to be used between exercise sessions. Discharge criteria Ensure patient is comfortable with adequate pain control. Ensure patient is confident about managing at home with necessary provisions/precautions. Ensure patient is competent with home exercise program, purpose of operation, rehabilitation plan and limitations, and prognosis. In association with the UCL Institute of Orthopaedics and Musculoskeletal Science Arrange urgent outpatient physiotherapy appointment preferably prior to discharge (unless at weekend). Phase I: Week 0-6 1. Monitor wound and ensure appropriate healing prior to pushing ROM. 2. Monitor and manage patient pain levels including adequate medication, use of cryogenic therapy and limitation of general activity. 3. Monitor any neurological deficits/changes in early post-op period (chart if appropriate and ensure the provision of appropriate resting splints if required). 4. Monitor and control excessive oedema in the arm or hand. You may need to slow rehabilitation down if there are wound complications in the early phase. 5. Progress eccentric control into flexion and active extension exercises (focus of triceps mechanism). 6. Ensure pronation/supination elements are being maintained within pain limits. 7. Encourage ongoing use of resting splints for night time use only for first 1-2 weeks unless there is a significant risk of losing ROM (ie unremitting pain, anxiety, significant difficulty with operative release, overactive biceps). 8. Review background core control, posture, scapular kinematics etc. Treatment options: Passive stretches into extension and if required very careful stretches into flexion as excessive pressure can irritate the joint capsule (careful about bony block at the radio-humeral joint). Capsular and soft tissue mobilisations (ensure wound is healed). Joint line accessory mobilisations as appropriate (consider Mulligan concepts MWM’s). Progressive eccentric triceps activation to maintain passive flexion element (reduces biceps activity therefore limiting the potential for a flexion contracture). Use of tubigrip and cryogenic therapy for exercise induced oedema. Milestones for progression to phase II: 1. Adequate pain and oedema control coupled with sound wound healing. 2. Easily maintained PROM within intra-operative limits (allow -10%). 3. Competent muscle control through range (esp triceps and forearm musculature). Phase II: Weeks 6-12 1. Incorporate some forearm resistance work for flexor/extensor muscle groups. 2. Add some gentle closed chain work (ie wall press-ups with progression to gym. ball, wobble boards, etc) to restore propioceptive elements. 3. Increase triceps and aconeus control through range (note: pre-op the elbow did not have the ROM therefore motor control needs to be trained into the new ROM) 4. Incorporate active biceps exercises. 5. Start to address kinetic chain (yes, Kibler’s principles of shoulder rehabilitation also apply to the elbow!). 6. Look at step-up and reach tasks (great for theraband work to triceps). In association with the UCL Institute of Orthopaedics and Musculoskeletal Science 7. Look at throwing techniques (DO NOT START ACTUAL THROWING till +12 weeks). Progression to phase III: 1. Pain and oedema have now resolved or at pre-op levels. 2. Competent AROM and no deficits to formal isometric muscle testing. Phase III: Weeks 12+ This is the patient specific component of program addressing sport/work specific demands. Patient in conjunction with therapist can look at return to gym, cycling, motorcycle, manual work, etc. No specific restrictions in this phase other than pain, swelling, and loss of ROM. Failure to progress: Problem Irritractible pain Clinical reasons Consider neuropathic pain Potential intra-articular pain Potential wrist pain General post-op pain Swelling Infection Poor vascular drainage Intra-articular irritation Early or progressive loss of Stiff capsule or adhesive ROM capsulitis. Secondary impingement due to instability post op or muscle imbalance. Overactivity in biceps/triceps Poor compliance with HEP Pain Management solutions Neurodynamic mobilisation, TENS, Acupunture, Meds, slow rehab to keep PROM Wrist support, review hand function for manual tasks. Do not forget risk of increased radial deviation (excision radial head). GP, clinic for review ASAP Positioning, review splints, lymphatic massage, compression garments/gloves, elevation of the limb. Increase intensity of PROM Stretches and frequency of appointments. Review night resting splints and encourage increased use. Review joint line articulations (valgus/varus deviations). Review endfeel for bony vs soft tissue elements in case of radial head,coronoid or olecranon impingement. Review resting muscle tone (surface EMG) and balance In association with the UCL Institute of Orthopaedics and Musculoskeletal Science between flexors /extensors and forearm rotators. Contact details: It is essential you contact us if you have any concerns: Physiotherapy Team: 020 8909 5820/5519 Occupational Therapy Team: 020 8909 5310 Consultant Team Secretaries: 020 8909 5456/5727 References: 1. Mansat P, Morrey BF: The column procedure: a limited lateral approach for extrinsic contracture of the elbow. J Bone Joint Surg Am 1998, 80:1603-15. 2. Morrey BF: Surgical treatment of extraarticular elbow contracture. Clin Orthop 2000, 57-64. 3. Cohen MS, Hastings H 2nd: Post-traumatic contracture of the elbow. Operative release using a lateral collateral ligament sparing approach. J Bone Joint Surg Br 1998, 80:805-12. 4. Itoh Y, Saegusa K, Ishiguro T, Horiuchi Y, Sasaki T, Uchinishi K: Operation for the stiff elbow. Int Orthop 1989, 13:263-8. 5. Morrey BF. Post-traumatic contracture of the elbow. Operative treatment, including distraction arthroplasty. J Bone Joint Surg Am. 1990 Apr;72(4):601-18. 6. A. Lindenhovius, J. Jupiter. The Posttraumatic Stiff Elbow: A Review of the Literature. The Journal of Hand Surgery, Volume 32, Issue 10, Pages 1605-1623 7. Timmerman LA, Andrews JR: Arthroscopic Treatment of Posttraumatic Elbow Pain and Stiffness. J Hand Ther. 2006 Apr-Jun;19(2):238-43 In association with the UCL Institute of Orthopaedics and Musculoskeletal Science