Distribution and Metabolism of Emulsions In Vivo
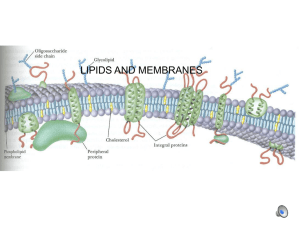
advertisement

Update on Parenteral Lipids: Which Patient ? Which Emulsion ? How much ? When ? Michael Adolph, M.D. Dept. of Anaesthesiology & Intensive Care, Klinikum Wolfsburg, 38440 Wolfsburg, Germany phone +49-5361-80-1410, fax +49-5361-80-1624, e-mail: Adolph-Michael@t-online.de Learning Objectives To identify the patients who will benefit from lipid emulsions in a TPN regimen To classify available lipid emulsions according to composition and metabolic effects To list the differential indications for the currently available lipid emulsions To understand principles and practice of the dosage and monitoring of intravenous lipid emulsions Introduction Dietary lipids are efficient fuels for many tissues of the body and can be used to prevent or correct essential fatty acid deficiency. Lipid emulsions are an important energy source for all patients requiring TPN because of their high energy density and low osmolarity. During the past two decades the old concept of only long chain triglycerides containing lipid emulsions was followed by newer concepts of reducing the high content of n-6 PUFA´s. The first step in that development was a physical mixture of medium and long chain triglycerides (MCT/LCT). Meantime this is a well proven concept in TPN regimens of many different patient types and disease states. A reduced content of n-6 PUFA´s can also be obtained by using newer preparations based on structured triglycerides or olive oil. A more promising step in the evolution of lipid emulsions can be seen in including fish oils to a physical mixture of MCT and LCT. Lipid Emulsions Containing MCT/LCT MCT/LCT-containing lipid emulsions have been available on the European market since 1984 and later worldwide. Meantime a great number of working groups have studied the parenteral application of this physical mixture not only in a clinical environment but also during long-term home parenteral nutrition (HPN). MCTs have several advantages in comparison with LCTs 1. Because of their physical and chemical properties, MCTs have better solubility and are more readily hydrolyzed by lipases. They are more quickly eliminated from the circulation and taken up by peripheral tissues. They are not stored as body fat but are oxidized more rapidly than LCTs. MCTs are ketogenic, and both medium-chain fatty acids and ketone bodies are carnitine-independent substrates. Compared directly with pure LCT emulsions, MCT/LCT emulsions are a more efficient fuel, put less strain on the liver, and have significantly less impact on the immune system and RES function. MCT/LCT emulsions appear to be of particular benefit to patients with systemic inflammatory response syndrome (SIRS) or sepsis because – containing only half the amount of long-chain triglycerides – they supply a significantly smaller amount of n-6 fatty acids and hence of the precursors of potentially immunosuppressive prostaglandins 2. Lipid Emulsions Containing Structured Triglycerides As an alternative to the physical mixture of MCT and LCT emulsions a mixture of MC and LC fatty acids can be obtained by interesterifying the different fatty acids to create a mixed triglyceride molecule called a structured triglyceride (STG) 3. Among STG chemically defined and randomized STG must be differentiated. Chemically defined STG molecules may act more efficiently but the costs for the synthesis are very high. This is why most of the research work in animals and patients was done with randomized STG emulsions. In 1997 Kruimel et al 4 presented the preliminary results of a study comparing the effect of randomized STG with a physical MCT/LCT mixture on the nitrogen balance of moderately catabolic patients after insertion of an aortic prosthesis. TPN was infused for 5 days. Over this period the cumulative nitrogen balance was less negative in the STG group but an adequate interpretation is difficult before the full publication of the study data. Regarding effects on the mononuclear phagocyte system as studied by use of the 99 m-technetium-sulfur colloid (TSC) clearance technique they found no difference between both groups 4. Chambrier et al 5 measured 3-methylhistidine excretion and total urinary nitrogen output in forty patients, scheduled for abdominal surgery. They were randomized to receive either STG or a physical MCT/LCT mixture. TPN was started on the day after surgery providing 100% of measured energy expenditure as 50% lipids and 50% glucose and 0.2 g nitrogen per kg bw and day. There were no significant differences in both outcome variables after 6 days of TPN. In conclusion, STG have been proven to be as safe as traditional LCT soybean oil emulsions. Compared to LCT, random STG have shown similar advantages as physical MCT/LCT mixtures. Further studies are necessary, to investigate potential benefits of STG compared to MCT/LCT in clinical settings. Lipid Emulsions Containing Olive Oil The potential of olive oil based emulsions for reduced lipid peroxidation was studied by several authors yielding conflicting results. From their animal study Dutot et al 6 concluded that olive oil emulsions are a better source of antioxidants and should contribute to decreased peroxidation. Arborati et al 7 evaluated both the lipid peroxide content and the peroxidability of fat emulsions under oxidative conditions. While highest values for lipid peroxide content were found in a 20% soybean emulsion the peroxidability was significantly increased in the soybean/olive-oil mixture. Lowest levels were found in a physical mixture of MCT/LCT. Garcia de Lorenzo et al 8 compared the Olive/Soya oil based lipid emulsion with a physical mixture of MCT/LCT in burned patients. After 6 days of TPN changes in plasma lipids, haemogram and liver function tests were similar in both groups. No differences between the two lipid emulsions on patients nutritional status or clinical outcome (ICU and hospital length of stay) were observed. Compared to conventional LCT emulsions, olive oil-based lipid emulsions show potential benefits regarding peroxidation and immune function. However, no clinically relevant outcome data are yet available demonstrating any advantage with regard to MCT/LCT emulsions. Lipid Emulsions Containing Fish Oil As reported previously [9], lipid emulsions containing fish oil (n-3 fatty acids) are poor substrates for lipoprotein lipase (LPL) and tend to accumulate in the circulation. In contrast to most triglyceride fatty acids, they are taken up by tissues mainly via remnant endocytosis, followed by intracellular triglyceride hydrolysis. Even the addition of n-3 containing triglycerides to classical LCT emulsions inhibits the release of free fatty acids from the soybean oil emulsion [9]. In contrast, the combination in the same particle of MCT together with n-3 fatty acid triglycerides appears to completely normalize triglyceride hydrolysis by LPL [10] and to rapidly produce small remnants enriched with n-3 fatty acids. In addition, Carpentier et al. [11] obtained evidence that the presence of both MCT and n3 fatty acid triglycerides in remnant particles enhances their uptake by different types of cells. Not only the alsolute amount of n-3 fatty acids, but the n-6/n-3 fatty acid ratio is determining the effects of an n-3 enriched lipid emulsion. Conventional soybean containing lipid emulsions have a n-6/n-3 ratio of approximatly 7:1, the olive / soybean mixture of 9:1. The recommended ratio of 4:1 to 2:1 for serverely ill patients [12, 13] is based on the requirements of healthy people (below 5:1 [14]) and takes into account the enhanced omega-3-fatty acid requirements of ill patients in respect to lowering the risk of an overwhelming systemic inflammatory response in hyperinflammatory stress situations. In 40 patients undergoing major intestinal surgery Wachtler et al. [15] analyzed the effect of TPN with a physical MCT/LCT mixture plus n-3 fatty acid triglcerides versus TPN with a physical MCT/LCT micture alone on the release of leukotrienes from whole blood leucocytes as well as circulating cytokines. In the n-3 supplemented group they observed a significant increase in 5-series leukotrienes and a decrease in the 4-series leukotrienes as an indicator of an attenuated inflammatory reaction. In contrast to interleukin-1, interleukin-6, and interleukin-10, the systemic levels of tumor necrosis factor- were postoperatively decreased in the n-3 supplemented group. n-3 fatty acids may also modulate regional blood flow and possibly prevent intestinal ischemia. Pscheidl et al. [16] could demonstrate in a low-dose endotoxin rat model that diets enriched with fish oil abolish the endotoxin-induced decrease of nutritive blood flow to the gut and ameliorate the bacterial defense of the splanchnic region. The lower count of viable bacteria in the fish oil groups was more related to an improved killing of translocated bacteria than a reduction of the translocation rate. Gadek et al. [17] could demonstrate that in patients with ARDS artificial nutrition for at least 4–7 days with a enteral diet supplemented with eicosapentaenoic acid (EPA), -linolenic acid (GLA), and antioxidants was superior to a control diet in terms of reduced pulmonary neutrophil recruitment and inflammation, improved oygenation, reduced time on the ventilator and stay in the ICU, and reduced morbidity as defined by the number of patients newly developing organ failure. However, not only n-6 but also n-3 polyunsaturated fatty acids are substrates for lipid peroxidation and inadequate balance by antioxidants may jeopardize their beneficial effects. Therefore a well balanced enrichment of this new generation of lipid emulsion with -tocopherol is strongly recommended [18]. Lipid Emulsions: When? How much? In clinical practice, lipids are suitable energy sources whenever TPN is indicated. Isolated organ failure per se is not a contraindication to the parenteral application of lipid emulsions. However, in all cases of impaired tissue blood flow and peripheral oxygen deficiency, e.g. as in shock, any type of TPN is contraindicated including the infusion of parenteral lipids. The patient should be hemodynamically stable before any form of nutrition is resumed. Following massive blood transfusions or in the presence of severe coagulation disorders, lipid infusion should be withheld temporarily. Caution should be exercised in primary lipid metabolism disorders, and lipid emulsions should be given only to provide essential fatty acids. In general, the dosage for lipid emulsions is between 0.5 and 1.5 g/kg bw/day. The calculated amount of lipids should be infused over at least 12 h per day, and during critical metabolic situations, a 24 h continuous infusion is strongly recommended. The ratio of fat calories to carbohydrate calories should be similar to that of a normal oral diet, i.e. one-third of calories should be provided as fat and two-thirds as carbohydrate. However, in times of critical illness and sepsis, when glucose intolerance is dominant and carbohydrate should not be given in excess of 3 g/kg bw/day, the proportion of infused fat can be increased to 1 : 1. The parenteral application of lipid emulsions should be increased in a stepwise manner with concomitant monitoring to ensure stable values of serum tiglycerides of no more than 3 – 4 mmol/l. References 1. Wolfram G. The use of lipid infusions in postoperative nutrition. Chirurgische Gastroenterologie 1994; 10: 173-176 2. Adolph M. Lipid emulsions in parenteral nutrition. Ann Nutr Metab 1999; 43:1-13 3. Nordenström J, Thörne A, Olivecrona A. Metabolic effects of infusion of a structured-triglyceride emulsion in healthy subjects. Nutrition 1995; 11: 269-274 4. Kruimel JW, Naber AHJ. Structured triglycerides. Educational Program XIX. ESPEN Congress. Amsterdam, 1997: 102-104 5. Chambrier C, Guiraud M, Gibault JP, Labrosse H, Boulétreau P. Medium- and long-chain triacylglycerols in postoperative patients: structured lipids versus a physical mixture. Nutrition 1999; 15: 274-277 6. Dutot G, Melin C. Assessment of lipid peroxidation during lipid infusion: influence of fatty acid composition of fat emulsion. Clin Nutr 1991; 10 (Suppl.2): 50 (abstr.) 7. Arborati M, Ninio E, Chapman MJ, Sultan F. Comparison of lipoperoxide content and lipoperoxidability in parenteral fat emulsions with different triglyceride content. Clin Nutr 1997; 16 (Suppl.2): O.18 (abstr.) 8. Garcia de Lorenzo A, Denia R, Martinez Ratero S, Fernandez Pavon A, Bereziat G, Le Brun A, Atlan P, Dutut G. Randomised, double-blinded study in severely burned patients under short term total parenteral nutrition (TPN) with a new olive-oil based lipid emulsion vs. MCT/LCT lipid emulsion. Clin Nutr 2000; 19 (Suppl.1): 177 (abstr.) 9. Oliveira T, Carpentier YA, Hansen I, Deckelbaum RJ. Triglyceride hydrolysis of soy vs fish oil LCT emulsions. Clin Nutr 1992; 11 (Suppl): 44 (abstr.) 10. Hamberger L, Carpentier YA, Hansen I, Deckelbaum RJ. In vitro lipolysis of MCT and fish oil containing emulsions: evidence that longer chain fatty acids must be cleared as intact triglycerides in emulsion remnants. Clin Nutr 1996; 15 (Suppl): 23 11. Carpentier YA, Siderova VS, Richelle M, Deckelbaum RJ, Eggerickx D, Sultan F. Does the presence of fish oil in emulsion particles affect the elimination of MCT/LCT emulsion. Clin Nutr 1996, 15 (Suppl): 2 (abstr.) 12. Fürst P, Kuhn KS. Fish oil emulsions: what benefits can they bring? Clin Nutr 2000; 19: 7-14 13. Morlion BJ. What is the optimum 3 to 6 fatty acid ratio of parenteral lipid emulsions in postoperative trauma Clin Nutr 1997; 16 (Suppl.2): P.98 (abstr.) 14. Deutsche Gesellschaft für Ernährung. Referenzwerte für die Nährstoffzufuhr (2000), Umschau/Braus, Frankfurt 15. Wachtler P, König W, Senkal M, Kemen M, Köller M. Influence of a total parenteral nutrition enriched with -3 fatty acids on leukotriene synthesis of peripheral leukocytes and systemic cytokine levels in patients with major surgery. J Trauma 1997; 42: 191-198 16. Pscheidl E, Schywalsky M, Tschaikowski K, Böke-Pröls T. Fish oil-supplemented parenteral diets normalize splanchnic blood flow and improve killing of translocated bacteria in a low-dose endotoxin rat model. Crit Care Med 2000; 28: 1489-1496 17. Gadek JE, DeMichele SJ, Karlstad MD, Pacht ER, Donahoe M, Albertson TE, Hoozen CV, Wennberg AK, Nelson JL, Noursalehi M. Effect of enteral feeding with eicosapentaenoic acid, -linolenic acid, and antioxidants in patients with acute respiratory disress syndrome. Crit Care Med 1999 27: 1409-1420 18. Dupont I, Siderova VS, Vanweyenberg V, Eggerickx D, Lontie J-F, Deckelbaum RJ, Carpentier YA. Incorporation of alpha-tocopherol in plasma lipoproteins during and after infusion of fish oil containing emulsions. Clin Nutr 1997; 16 (Suppl.2): 2 (abstr.)