MARTIN_TB Diagnostics_09152011 (FILEminimizer)
advertisement
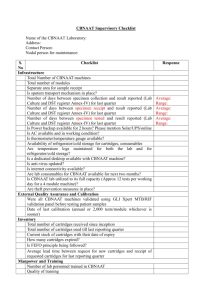
Welcome to the I-TECH Global Health Clinical Seminar Series September 15, 2011 Tuberculosis Diagnostics New Data on New Methods Robert Martin, MS, MPH, DrPH TB Diagnostics New data on new methods. Prevention of Deaths from TB Very few would have been saved by any diagnostic test. Specifically these deaths occur in mainly HIV-negative people, almost all of who die from drug-susceptible TB, principally because of the inadequacy of basic, inexpensive health care provision. Carlton A. Evans Perspective: GeneXpert-A Game-Changer for Tuberculosis Control? PLoSMedicine 2011 Vol.8(7)e1001064 What’s New? Stop TB Recommendations GeneXpert MTB/RIF Country experience – Pakistan The future For a disease that 8 million will acquire each year, why are we still using methods developed in the late 1800’s? 1. Populations that TB affects 2. Low prevalence (comparatively) in developed countries. 3. Rigorous (costly) regulatory standards in developed countries, so no incentive for manufacturers to develop new low-cost assays. What is new? The Global Plan to Stop TB 2011 - 2015 •Laboratory strengthening – included as a major component. •Fundamental research and operational research •Up-to-date epidemiological predictions. •Updated targets for TB care and for research and development. •Updated funding requirements. Estimated Funding to Implement Global Plan Laboratory Strengthening – $4 billion New Diagnostics - $1.7 billion Fundamental Research – $2.1 billion New Drugs - $3.7 billion New Vaccines - $1.9 billion Bridging the gap: LED-based Fluorescence Microscope Liquid culture media Endorsed by WHO, 2007 Line probe assay Serologic Assays? WHO Recommended Levels of Service WHO levels New Molecular Technologies? Recommended Services Culture/DST EQA Training Microscopy Many resourcelimited countries Culture/DST Microscopy EQA/Training? Intermediate Laboratory Culture/DST EQA Training Microscopy Microscopy Peripheral Laboratory Microscopy Microscopy Central Laboratory The Game Changer? On 8 December 2010 the World Health Organization (WHO) endorsed the Xpert MTB/RIF assay. GeneXpert High tech in low tech settings: XpertTM MTB GeneXpert Automated Sample Prep, Amplification and Detection <120 minutes 2008 Development Evaluation in 5 trial sites 2010 2009 Demonstration in 15 microscopy centers STAG Access Challenges downstream: Meeting the target price A technology platform: TB & Rif Resistance Potential for HIV viral load Potential for … Recent Publications Addressing GeneXpert MTB/RIF Testing Boehme CC, Nicol MP, Nabeta P, et al. Feasibility, diagnostic accuracy, and effectiveness of decentralized use of the Xpert MTB/RIF test for diagnosis of tuberculosis and multidrug resistance: a multicentre implementation study. Lancet 2011. April 30, 377(9776):1495-1505. Helb D, Jones M, Story E, et al. Rapid Detection of Mycobacterium tuberculosis and Rifampin Resistance by Use of On-Demand, Near-Patient Technology. JCM 2011 v48(1). Vadwai V, Boehme C, Nabeta P, et al. Xpert MTB/RIF: a New Pillar in Diagnosis of Extrapulmonary Tuberculosis? JCM 2011. V 49(7)p.2540-5. Comparison of Xpert MTB/RIF with Other Nucleic Acid Technologies for Diagnosing Pulmonary Tuberculosis in a High HIV Prevalence Setting: A Prospective Study. Scott LE, McCarthy K, Gous N, et al. PloS Medicine 2011. V8(7)e1001061. Dowdy D, Cattamanchi A, Steingart KR, Pai M. Is Scale-Up Worth It? Challenges in Economic Analysis of Diagnostics Tests for Tuberculosis. PLoS Med 8(7):E1001063/journal.pmed.1001063 Methods/Results (Boehme et al.) Population - 6,648 adults >18 years of age (1,033 culture positive) One-off testing MTB/RIF detected more than 90% of patients with positive cultures (90% sensitivity, 99% specificity) MTB/RIF test sensitivity was 76.9% in smearnegative, culture-positive patients (296 of 385) Smear microscopy (2-3 examinations per patient) detected 67.1% Results Correctly identified 242 of 250 rifampicin resistant TB (96.8% sensitivity) Correctly identified 779 of 810 rifampicinsensitive cases (96.2%) With modified software, decreased sensitivity to 94.4% and increased specificity to 98.3% Results Of 153 patients with clinically diagnosed TB and negative culture, 24 (16%) had a positive MTB/RIF– 20 of 24 (83%) improved on treatment. Proportion of tuberculosis cases detected by each method in culture-positive patients Percentages are the maximum proportion of cases detected by every method. (A) Tuberculosis case detection. (B) Detection of rifampicin resistance. Time to detection was defined as time between date of sputum sample collection and date of positive result. MTB=Mycobacterium tuberculosis. RIF=rifampcicin. Boehme CC, Nicol MP, Nabeta P, et al. Feasibility, diagnostic accuracy, and effectiveness of decentralized use of the Xpert MTB/RIF test for diagnosis of tuberculosis and multidrug resistance: a multicentre implementation study. Lancet 2011, published online April 19. DOI:10.1016/S0140-6736(aa)60438-8. Issues for Small Health Centers Stable electricity Equipment should not be operated in environments >30C Cartridges stable at 2-28C No data for use in dusty or humid conditions Requires annual calibration Need studies to evaluate the impact of early detection (cost effectiveness?). Results – Analytic and Validation Study Vietnam (Helb et al.) Clinical limit of detection – 131 CFU/ml in sputum In small validation study of 107 sputum samples from Vietnam Detected 29/29 (100%) smear +, culture+ Detected 33/39 (84.6%) smear -, solid culture+ Detected 38/53 (71.7%) smear -, liquid culture+ Results – India (Vadwai et al.) Extrapulmonary Specimens 547 extrapulmonary specimens (biopsy, pus, body fluids, CSF) Reference standard a composite of smear & culture results and clinical, radiological and histological findings. Culture – 53% (150/283) sensitivity MTB/RIF – 81% (228/283) sensitivity Lowest (29%) sensitivity in CSF samples 64% (89/138) in smear-negative 96% (139/145) in smear-positive Results – Comparison with Other NAT in a Prospective Clinical Validation South Africa (Scott et al.) 311 participants; 70% (215/311) HIV prevalence; 38.5% (120/311) culture positive TB Sensitivity when compared to liquid culture Smear + – 59% Smear Negative MTBDRplus – 76% 28% LCTB – 76% 22% MTB/RIF – 86%; in HIV + - 84% 61% Specificities all >97% Results – Comparison with Other NAT in a Prospective Clinical Validation South Africa (Scott et al.) Sensitivity when compared to clinical definition Smear + – 40% MTBDRplus – 51% LCTB – 51% MTB/RIF – 58% GeneXpert – A Game-Changer for Tuberculosis Control? C.A. Evans PLoS Medicine July 2011 Vol 8 Issue 7 Intermediate Sensitivity – Better than microscopy, less than broth culture. A single MTB/RIF test detected less than half of cases of smear-neg, culture-pos TB in HIV-positive patients False resistance Issue: Benefits of increased correct diagnoses with adverse consequences of occasional misdiagnoses. GeneXpert – A Game-Changer for Tuberculosis Control? C.A. Evans PLoS Medicine July 2011 Vol 8 Issue 7 Improved Accuracy Requires access to confirmatory culture-based testing. May increase demand for specialty reference laboratories and/or their services (e.g., BSL3). If RIF resistant, immediate implications for the need for DST to second line drugs (? increased demand for specialty reference laboratories). Outcomes from the Global Consultation • Agreement on interim diagnostic algorithms prepared by Working Groups. • Agreement to pursue Xpert MTB/RIF roll-out in a systematic and coordinated programmatic approach in a so-called ‘Evidence for scaling-up’ phase during 2011. • Development of a ‘Rapid Implementation’ document to guide Xpert MTB/RIF roll-out in the ‘Evidence for scaling-up’ phase. • Monitoring of global sales and market dynamics by FIND • Establishment of a post-marketing surveillance programme by FIND • Organization of an Early Implementers’ Meeting in December 2011 to share experiences. Beyond Implementation of Technology How to best implement to improve patient care. Who should receive limited capacity for better tests. How will these tests impact patient-relevant outcomes. How will these issues vary among settings (e.g., will suspect TB cases who are smear negative require MTB/RIF test?) Is Scale-Up Worth it? Addressed each of four possible test results. Pointed out that studies generally enrich the population with disease (e.g., high prevalence). Predictive value is high with a low number of false positives. Costs of false-positives often underestimated. Costs of scale-up could divert resources from more cost-effective interventions (e.g., access to highquality microscopy) Is Scale-Up Worth It? Challenges in Economic Analysis of Diagnostics Tests for Tuberculosis. Dowdy D, Cattamanchi A, Steingart KR, Pai M. PLoS Med 8(7):E1001063/journal.pmed.1001063 Example: India Providing Xpert MTB/RIF at current prices to 15% of all TB suspects would consume the entire budget of the National TB Program ($65M). Implementing Xpert MTB Rif diagnostic assay in Pakistan Operational Issues WHO Recommended Levels of Service WHO levels New Molecular Technologies Recommended Services Culture/DST EQA Training Microscopy Many resourcelimited countries Culture/DST Microscopy EQA/Training? Intermediate Laboratory Culture/DST EQA Training Microscopy Microscopy Peripheral Laboratory Microscopy Microscopy Central Laboratory Piloting of GeneXpert in Pakistan Objective :• Pilot test diagnostic algorithm for early diagnosis of MDR and smear negative TB with use of GeneXpert at 12 sites . • Financial support : US (DOS) Xpert Implementing sites – laboratory workload Recommendation • 10-20 samples a day or 2000-4000 annually from high risk group Issues and challenges • Expected samples from high risk group in implementing sites is much lower Solution • Referral linkages and specimen transport to ensure optimal efficiency Selection of individuals to Test HF with AFB microscopy + Xpert Xpert-Import • Tax exemption from central board of revenue • Custom clearance Xpert – Central storage of Kits Recommendation : Temperature for storage of kitS 2-28C Issue/challenges • Lack of cold storage space for kits Solution • Request to EPI(extended Programme for immunization) for storage of KITS Xpert Implementation –Infrastructure Recommendation/Requirement uninterrupted and stable electrical power supply . Issues /challenges • Xpert with UPS having 15 min back up only • Severe power crises with long hours of power failures is common • Only 5/12 proposed sites has generator back up –but generator output is not stable . Solution • Power supply stabilizers and UPS with 2hours battery back up. Xpert Implementing sites – Ambient temprature Recommendation • ambient temperature not to exceed 30C Issues and challenges • Temperature exceeding 40c in summers is usual across country Solution • Air conditioners for all installation site Xpert Implementing sites – storage of kits Recommendation • Storage of KITS 2-28C Issues and challenges Enough refrigerators not available Solution • Dedicated refrigerator (freezer less) for storage of KITS Xpert Implementing sites – laboratory worload Recommendation • 10-20samples a day or 2000-4000 annually from high risk group Issues and challenges • Expected samples from high risk group in implementing sites is much lower Solution • Referral linkages and specimen transport to ensure optimal efficiency Workshop for Early Implementers Chateau du Penthes, Pregny-Chambésy (Geneva), Switzerland 7 - 8 April 2011 Meeting Objectives • To provide country health programmes and their local and international technical partners with the science behind Xpert MTB/RIF, assay performance characteristics and the need to link diagnosis with treatment and care in different epidemiological and resource settings; • To discuss with countries and partners the practical considerations for roll-out of Xpert MTB/RIF using the WHO Implementation Document, including interim diagnostic algorithms, patient management approaches, and key data elements to be collected to inform future scale-up; • To map country and technical partner plans for roll-out of Xpert MTB/RIF in order to maximize resources and avoid duplication and overlap. Other New Developments WHO Policy/Recommendations The Pipeline for New Technology The Lancet, Volume 377, Issue 9760, Pages 113 - 114, 8 January 2011 WHO recommends against inaccurate tuberculosis tests The available evidence indicates that current tests lack either the necessary sensitivity or specificity or both to be an effective diagnostic test, and for many of these tests, false results far outnumber true results. WHO Diagnostic Evaluation No. 2 - Laboratory based evaluation of 19 commercially available rapid diagnostic tests for tuberculosis Why Are Serological Tests for TB Inaccurate? From WHO Diagnostic Evaluation Series No. 2 Heterogeneity of host immunological responses to TB antigen. The profile of antigenic proteins of MTB recognized by antibodies differs at different stages of infection and disease progression. Thus, an accurate diagnostic test for TB will almost certainly need to be based on a combination of antigens. Rapid Methods for Identification and Susceptibility Testing Alternatives to liquid or solid culture – MODS, Thin Layer Rapid DST testing from culture (e.g., Capilla, Reazurin Microtiter Assay) Molecular testing methods for identification of TB and DST (e.g., Hain Geno Type, INNO-LiPA RifTB) Challenges to all of these in resource limited settings (e.g., minimum requirements to establish a successful molecular testing facility) Possible changes in biosafety requirements being considered by WHO? Possibly three levels under consideration dependent on risk Low – Preparing smears or preparing GeneXpert cartridges. Moderate – culture, DST (manipulation in BSC class I or IIA, room ventilation with 6-12 air exchanges/hour, PPE (glove recommended, gowns, respirators not required, restricted access, training to minimize aerosols. High – XDRTB (manipulation performed in BSL4) Progression of Development of TB Diagnostics http://www.tbevidence.org/tbdxpl.htm Lessons learned Political will and commitment Ensure a reliable supply of reagents and supplies Sustainability requires integration into a national laboratory policy and into strategic plans Conclusion New interest in laboratory strengthening. Exciting and promising new laboratory technologies – improved sensitivity. Must keep in mind that technologies are replaced quickly – is the future a POC NAT or POC antigen or antibody (or both) detection test? However, GeneXpert (or any new technology): implementation in the field (where) and how it will be used (algorithm) will be critical learning experiences. to be cost-effective, good clinical judgment is required as well as quality assured smear-microscopy. A referral system for transfer of specimens to a reference laboratory for DST will still be necessary. economic evaluations in each country will be an important consideration. Thank You Robert Martin, MPH, DrPH University of Washington RMartin1@uw.edu Thank you! Next session: Oct 27, Case Consultations: HIV Listserv: itechdistlearning@uw.edu Email: DLinfo@uw.edu Welcome to I-TECH HIV/AIDS Clinical Seminar Series Next session: October 27 Case Consultations: HIV Chris Behrens MD, Shireesha Dhanireddy MD, Robert Harrington MD and Christian Ramers MD MPH