Design and Analysis
Techniques for CaseControl Studies
Instructor: 李奕慧
yihwei@mail.tcu.edu.tw
1
Lecture Overview
1.
2.
3.
4.
5.
Case-Control Study
Example: ”Risk factors associated
with lung cancer in Hong Kong”
OR for multiple exposure levels
Confounding factors
Methods of Controlling (adjusting for)
confounders
2
Epidemiologic Study Design
Analytical studies
Intervention
studies
Clinical trials
Observational studies
Cohort studies
Case-control studies
3
Case-control study
Exposed
Cases
Non-exposed
Study Population
Exposed
Controls
Non-exposed
4
Selection of cases
Establish a strict diagnostic criteria for the
disease:
Examples:
Type 1 diabetes in children: severe symptoms,
very high BG, marked glycosuria, and
ketonuria.
Type 2 diabetes: few if any symptoms, Slightly
elevated BG, diagnosis “complicated”.
5
Selection of cases
Population-based cases: include all subjects or
a random sample of all subjects with the disease
at a single point or during a given period of time
in the defined population:
Danish
childhood diabetes register
Hospital-based cases:
All patients in a hospital department at a given
time
6
Selection of Controls
Principles of Control Selection:
Study base:
Controls
can be used to characterise the distribution of
exposure
Comparable-accuracy
Equal
reliability in the information obtained from cases
and controls no systematic misclassification
Overcome confounding
Elimination
of confounding through control selection
matching or stratified sampling
7
Selection of Controls
General population controls:
registries,
households, telephone sampling
costly and time consuming
recall bias
eventually high non-response rate
Hospitalised controls:
Patients
at the same hospital as the cases
Easy to identify
Less recall bias
Higher response rate
8
Ascertainment of Disease and
exposure status
External sources:
Death
certificates, disease registries, Hospital
and physicians records etc.
Internal sources:
Questionnaires
and interviews, information
from a surrogate (spouses or mother of
children), biological sampling( e.g. antibody)
9
Bias in Case-Control studies
Selection bias
Non-response
Detection
bias
cases and controls are identified not independently of
the exposure
Observation bias
Recall
Bias: Cases are more likely to remember
exposure than controls
10
Strengths in Case-control
Quick,
inexpensive
Well-suited to the evaluation of
diseases with long latency period
Rare diseases
Examine multiple etiologic factors for a
single disease
11
Limitations in Case-control
Case-control study
Not rare exposure
Incidence rates cannot be estimated
unless the study is population based
Selection Bias and recall bias
12
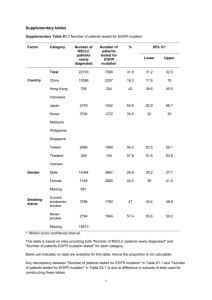
Risk factors associated with
lung cancer in Hong Kong
Lung Cancer 40 (2003) 131-140
13
Chi-Square Tests
Value
Pearson ChiSquare
Asymp. Sig.
(2-sided)
df
0.257a
1
Exact Sig. (1sided)
Exact Sig. (2-sided)
.613
Risk Estimate
95% Confidence Interval
Value
Odds Ratio for Marital
(other / married)
.880
Lower
.535
Upper
1.446
14
Multiple Exposure Levels
Exposure
level
Cases
Controls
OR
A1
B1
OR1
B2
B3
OR2
Low
A2
A3
Not exposed
C
D
Reference
High
Medium
OR3
15
Multiple Exposure Levels
A significant (P<0.05) increasing trend in the OR was found between nonsmokers,
ex- and current smokers; and increasing amount of smoking
among the ever smokers.
Lung cancer.sav
Lung Cancer 40 (2003) 131/140
16
smoking * case Crosstabulation
smoking
Total
nonsmoker
Count
% within case
exsmoker
Count
% within case
current smoker Count
% within case
Count
% within case
case
case
control
52
96
24.5%
45.3%
68
87
32.1%
41.0%
92
29
43.4%
13.7%
212
212
100.0%
100.0%
Total
148
34.9%
155
36.6%
121
28.5%
424
100.0%
Chi-Square Tests
Pearson Chi-Square
Value
48.212a
df
Asymp. Sig.
(2-sided)
2
.000
Likelihood Ratio
50.088
2
.000
Linear-by-Linear
Association
N of Valid Cases
42.734
1
.000
424
抽煙與罹患肺癌有
關,
Case中抽煙者佔較
高的比例(43% vs
13.7%)
a. 0 cells (.0%) have expected count less than 5. The minimum expected count is 60.50.
17
Data > Select cases >
18
只選smoking=2,
3的資料進行分析
Risk Estimate
95% Confidence Interval
Value
Odds Ratio for
1.443
smoking (exsmoker /
nonsmoker)
Lower
Upper
.908
2.293
1.249
.942
1.656
For cohort case = control
.865
.721
1.039
N of Valid Cases
303
For cohort case = case
Exsmoker 罹患肺癌
是nonsmoker的1.4
倍,
95%CI (0.9, 2.3)
Exsmoker與
nonsmoker罹癌機率
沒有顯著差異
19
Confounding factors (干擾因素)
Confounder:
Variable is associated with both the
disease and the exposure variable.
20
Method for control for confounders
1.
2.
3.
Study design:
restriction/ matching/ randomization
Statistical adjustment:
Standardization; e.g. age standardized (where
age is a confounder)
Stratified by confounder (Mantel-Haenszel test)
Incorporate the confounder into a regression
analysis as a covariate. (logistic regression
approach)
21
Restriction
Example
研究主旨:二手煙(ETS, exposure)與罹患肺癌
(disease)的關係
confounder: 研究對象本身是否抽煙
為了避免干擾只分析ETS對nonsmoker的影響
22
Stratified Analysis
23
將性別當作分層(stratum)的因子
smoking * case * sex Crosstabulation
Count
sex
male
smoking
ex- and current smoker
nonsmoker
female
Total
smoking
ex- and current smoker
nonsmoker
Total
case
case
control
160
116
Total
276
52
212
13
96
212
6
148
424
19
106
119
113
119
219
238
Lung cancer2.sav
24
Sex-Specific OR for smoking
Risk Estimate
sex
male
female
95% Confidence
Interval
Value Lower
Upper
2.55
1.68
3.85
Odds Ratio for smoking (ex- and
current smoker / nonsmoker)
N of Valid Cases
Odds Ratio for smoking (ex- and
current smoker / nonsmoker)
424
2.31
N of Valid Cases
238
0.85
6.30
可以將男士的OR與女士的OR合併嗎?
怎麼併?
Lung cancer2.sav
25
Thank you!
26