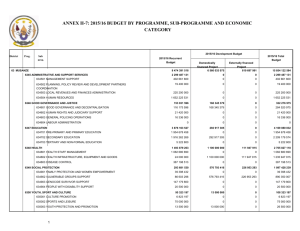
- MAST model info
advertisement

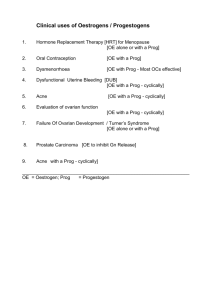
Domain 5: Economic aspects Kristian Kidholm Odense University Hospital, Denmark Content 1. Background 2. Societal level: Economic evaluation 2.1. Estimation of costs 13/04/2015 3. Institutional level: Business case 4. Methods for data collection 5. Sensitivity analysis 6. Summary 2 Background Growth in health care expenditure per capita (%) The economic situation in european health care: - Health care cost have been rising more than GDP - New pharmaceutical product (e.g. cancer) - Financial crisis – reduced growth - The population is getting older Growing need for prioritizing: 1. 2. 3 Growth in GDP per capita (%) Societal level => need for societal economic evaluation Health care institutions => need for business case (expenditure – revenue) Source: OECD Health Data 2009 Societal level: Economic evaluation Economic evaluation: • Comparative analysis of alternatives in terms of cost and consequences Costs Programme A Consequences Choice: Costs Programme B Consequences Types of economic evaluations: Cost-minimisation analysis (CMA): Incremental cost of A Cost-effectiveness analysis (CEA) Incremental cost of A per extra unit of outcome Cost-utility analysis (CUA) Incremental cost of A per extra QALY Cost-benefit analysis (CBA Cost-benefit ratio of A? 4 Societal level: Economic evaluation Economic evaluation: • Comparative analysis of alternatives in terms of cost and consequences Costs Programme A Consequences Choice: Costs Programme B Consequences Based on data from other domains Types of economic evaluations: Cost-minimisation analysis (CMA): Incremental cost of A Cost-effectiveness analysis (CEA) Incremental cost of A per extra unit of outcome Cost-utility analysis (CUA) Incremental cost of A per extra QALY Cost-benefit analysis (CBA Cost-benefit ratio of A? 5 Estimation of costs Cost = the value of resources used (when using telemedicine) = Quantities of resources used * Prices What kind of resource use should be included? 6 - Describe the patient pathways: - Where are resources used? Prog. A Prog. B - If the perspective is societal: Include all resources used by • Hospitals • The municipality • The patients • The relatives Estimation of costs Topics and outcomes Resource use related to delivering telemedicine: • Investments in equipment etc. • Training of staff • Maintenance • Use of staff (time) Which outcomes to include? – Medical doctors – Nurses – Etc. • • • • • Medication Utensils Patients’ use of time Relatives’ use of time Transportation Where do you expect telemedicine to cause a positive or negative change? See 78 examples in the appendix of the MAST Manual Estimation of costs Topics and outcomes Resource use related to changes in use of health care: • • • • • • Primary care Emergency unit visits Outpatient visits Hospitalisation Bed days Tertiary care Which outcomes to include? Where do you expect telemedicine to cause a positive or negative change? Estimation of costs Hints - Estimation of costs in practise: Disregard: - Costs that are similar for programme A and B (e.g. overhead costs per patient) - Minor costs, that does not change the results Collect data for use of resources for each patient: - If costs are expected to vary - But not for costs that are the same for all patients (fixed costs) Should investment be included? - Yes! - Estimate “equivalent annual costs” - Divide costs between different programs Estimation of costs Prices: - Should reflect opportunity costs (forgorne beneits) In practise: - Use market prices if possible - The price of patient time: Use average wage rate (e.g. 50% for retired patients) Presentation of results: - Prices for each resource should be presented (e.g. in appendix) - Increases transferability Reporting of results Economic evaluation: 1. Average use per patient of resources in programme A and B 2. Average costs per patient for each resources 3. Total costs per patient 4. Incremental analysis of costs and consequences, e.g. cost-effectiveness ratio 5. Sensitivity analysis - Confidence intervals, P-values (statistical significance) 11 Reporting of results Reporting of costs of using telemedicine and the alternative Prog. A. Average use Prog. B. Average use Prog. A. Average costs Prog. B. Average costs Investments in equipment etc. € € Training of staff € € Maintenance € € Use of staff (for each of the relevant type of staff) € € Medication € € Utensils € € Patients’ use of time € € Relatives’ use of time € € Transportation € € Total costs € € Reporting of results Reporting of changes in use of health care resources Prog. A. Average use Prog. B. Average use Prog. A. Average costs Prog. B. Average costs Primary care € € Emergency unit visits € € Outpatient visits € € Hospitalisation € € Bed days € € Tertiary care € € Total costs € € Business case Aim: Estimate Return on Investment for the institution using telemedicine = Increase in revenue (money gain) Expenditures (money invested) Part 1: Expenditures: - E.g. increase in the hospitals total expenditures of treating the patient group Estimation: - E.g. What is the hospital expenditures related to the use of resources? - Business case Part 2: Changes in revenue • For public financed hospitals: Changes in reimbursement Estimation for hospitals: • Change in DRG-rate • Change in number of patients • Change in total reimbursement Notice: • Does telemedicine change the DRG-rates per patient? • Will the DRG rate be changed in the future? Business case Presentation of results of the business case: • Describe data • • • Estimate change in expenditure per patient Estimate change in number of patients Estimate change in total expenditure • • • Estimate change in revenue per patient Estimate change in number of patients Estimate change in total revenue • Sensitivity analysis Notice: The result of a business case can be very different from the economic evaluation Methods for data collection Generally: – Criteria for quality of data on economic aspects are similar to criteria for quality of data on clinical effects Systematic literature review New studies: 1. Design: RCT, Cluster RCT, controlled studies 2. Methods for data collection: – CRF: Case Report Form (used by staff) – Patient diary – Interview or questionnaire to patients – Interview or questionnaire to staff – Data from hospital registers 17 Sensitivity analysis Sensitivity analysis: • How does the costs change by changes in the parameters? Example: What if the number of patients is changed? If you have made large investments Estimate average cost if no. if patients is increased or decreased Describes also transferability Cost per patient 120 100 80 60 Serie1 40 20 0 1 3 5 7 9 11 13 15 17 19 21 23 25 27 29 Number of patients ( * 100) Summary 1. Include both societal economic evaluation and business case 2. Economic evaluation: Estimate differences in use of all kinds of resources (costs) Present arguments for choice of outcomes Collect data for each patient (similar to clinical data) 3. Business case - Estimate changes in the institutions expenditures and revenues 4. Assess sensitivity and transferability of the results Main reference: Methods for the Economic Evaluation of Health Care Programmes (Oxford Medical Publications) M.F. Drummond, M.J. Sculpher, G.W. Torrance, and B.J. O'Brien Questions? www.renewinghealth.eu