File
advertisement

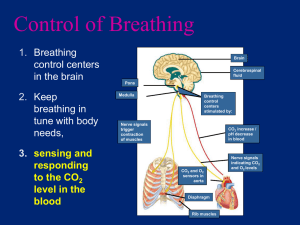
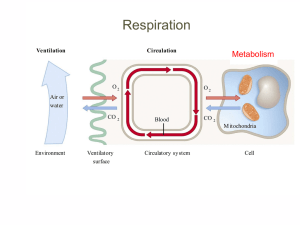
Respiration Control of Breathing Dynamics of Breathing External/Internal Respiration Gas Transport in Blood Control of Breathing PRIMARY MECHANISM • [CO2] and [H+] within the blood are the primary stimuli that affect a person’s breathing rate/depth. • CO2 and H+ levels in the blood (including all ways that they are carried) are detected by chemoreceptors (chemical-sensitive nerve endings) in the Respiratory Center of the MEDULLA OBLONGATA in the brainstem (top of spinal cord). • • The Medulla Oblongata is the part of the brain that controls the body’s organ systems. (p.334-335) The respiratory center is a cluster of nerve cells that trigger inspiration through automatic, fairly rhythmic discharges. CO2 and H+ ions are also detected by Carotid Bodies (chemoreceptors) in the carotid arteries, and by Aortic Bodies (chemoreceptors) located in the aorta. -- these bodies communicate (via nerves) with the Respiratory Center when CO2/H+ levels are too high/low. • When the levels of CO2/H+ increase in the blood (usually coupled with decreased O2), the RATE and DEPTH of breathing increases. Vice versa too… • The Respiratory Center receives signals from the Carotid/Aortic Bodies and sends a nerve message to the diaphragm and intercostal muscles to contract more often and for longer (fig. 15.6 p. 290). *** An increase of 0.3% CO2 in the blood DOUBLES the breathing rate!!! SECONDARY MECHANISM o O2 levels in the blood are detected by the same Carotid and Aortic Bodies. o Oxygen levels have little effect on the respiratory center, unless there exists an extreme deficiency. o Cases could be: o High Altitudes, CO poisoning, extreme blood loss. o The Carotid/Aortic Bodies detect the extreme O2 deficiency and signal the Respiratory Center to increase the rate/depth of breathing (again, low O2 is usually coupled with high CO2/H+, but not necessarily in extreme cases – some anaerobic respiration can produce CO2 as a byproduct). Hyperventilation lowers CO2 levels to below normal increases blood pH constricts blood vessels in brain lowers O2 levels in brain faint. Breathing into paper bag? Increases CO2 levels to keep pH nearer to normal… Synchronicity!!! The respiratory center responds to a variety of nervous and chemical signals, adjusting the rate/depth of breathing accordingly. Control of breathing is only effective if it is synchronized with the circulatory system. eg. During exercise, cardiac output is aligned with the increased breathing rate, thus enhancing the O2 supply and CO2 removal. Dynamics of Breathing -- Inspiration The respiratory center signals the diaphragm and the intercostal (rib) muscles to contract. Results: normally ‘dome-shaped’ diaphragm flattens out; intercostals contract to move ribcage up and out. * during ‘rest’ (normalcy), only the diaphragm contracts; intercostals contract during stressful/exertive situations. Both of these contractions/movements serve to increase the size of the thoracic cavity. - Since the lungs are attached to the diaphragm and the intercostals/ribs by pleural membranes, the contraction of each (and the increased thoracic cavity volume) increases the size of the lungs (and the alveoli, themselves) as well. - So, the air pressure within the lungs decreases to a point where it is less than atmospheric air pressure (ie. the air pressure outside the body). A notable pressure gradient has now been created and air flows from a region of higher pressure (outside of body) to a region of lower pressure (inside lungs/alveoli). Result: Air rushes into lungs/alveoli. Fig. 15.7a p. 291. Humans breathe due to negative pressure – air does not force the lungs open, they are opened up before air enters; a negative (relative to the ‘outside’ of the body) pressure induces this. In other words, a partial vacuum is created in the lungs/alveoli – air flows into this vacuumlike region of space. Inspiration is an active process since muscles must contract in order for it to occur. The stretch receptors in the alveolar walls signal the respiratory center to stop stimulating the diaphragm/intercostals – end of inspiration. Dynamics of Breathing -- Expiration Upon ceased stimulation from the respiratory center, the diaphragm and the intercostals relax and return to their resting positions: The diaphragm resumes its dome shape by pushing upward; The intercostals relax, dropping the ribcage down and inward. See fig. 15.7b p. 291. Both of these actions serve to decrease the size of the thoracic cavity, decrease the size of the lungs (the lungs recoil), and increase the air pressure in the lungs to greater than that of atmospheric air. Air, once again, flows from a region of higher pressure (the lungs/alveoli) to a region of lower pressure (the ‘outside’). Expiration is a passive process in that it simply involves the relaxation of muscles. That said, expiration, at times, may be active in nature when breathing is deeper and/or more rapid (eg. during exercise). Intercostal muscle contractions can FORCE the ribcage down and in with more vigor; Contraction of abdominal muscles can push diaphragm upwards with more force. Thus, more air might be expelled at a faster rate. Lung Air Capacity The volume of air a human inhales and exhales with each breath is called tidal volume (avg = 500 mL). The maximum volume of air that can be inhaled/exhaled during forced breathing is known as vital capacity (avg = 4-5 L). The lungs are actually able to hold more air than the vital capacity, but since it is impossible to completely empty (and thus, collapse) the alveoli, a residual volume of air remains in the lungs after active expiration (avg = 1.2 L). This air plays no role in gas exchange. Certain respiratory disorders increase the residual volume of the lungs (more useless air = less chance to get useful air weak, short of breath, etc). Avg total lung capacity = 6 L. See fig. 15.5 p. 288 Some inspired air (in all people) never reaches the lungs; instead it fills the respiratory tract where there exists no gas exchange functioning Known as ‘dead space’ air… To increase the chances of inspired air reaching the lungs, and expired air actually reaching the ‘outside’, it is better to breathe slowly & deeply – luckily, the medulla promotes this. This idea is evident when getting a cramp while running (the cramp is indicative of anaerobic respiration taking place in certain muscles (usually the abs)) – it is better to exhale deeply to rid body of dead space air so that the next inhalations contain mainly ‘fresh’ air with a higher % of O2. External Respiration (Location: Lungs) Refers to the exchange of O2 and CO2 between the alveoli and the blood in the alveolar (pulmonary) capillaries. Recall that the two structures are, at most, 0.2 micrometers apart and that each of them possess walls that are only one cell thick – excellent conditions for efficient exchange. Transfer occurs via simple diffusion, but the gradient is based on gas pressures. All gases exert pressure (proportional to their concentrations); each indiv. gas exerts its own partial pressure (PP). The PPO2 in the alveoli (due to the inspiration of O2-laden air) is higher than the PPO2 in the lung capillaries (due to the usage of/transfer of O2 by/to the tissue cell capillaries in the body). Thus, O2 flows (via the principles of diffusion) from a region of higher PP (alveoli) to a region of lower PP (blood). CO2 follows a similar gradient, except that it moves, via diffusion (higher PP to lower PP), from the lung capillaries into the alveoli for expiration. CO2 is produced as a byproduct of cellular respiration by the body’s cells – high blood PPCO2 PPCO2 in inhaled air is quite low. Internal Respiration (Location: Body Cells) Gas exchange that occurs at the tissue cell level is between the blood in the capillaries and the ECF (tissue fluid) – the material entering the ECF eventually enters cells; the material ‘waiting’ in the ECF to enter the blood originated within the cells. PPO2 in blood > PPO2 in ECF O2 diffuses into ECF for eventual entry into cells. PPCO2 in ECF > PPCO2 in blood CO2 diffuses into blood (in order to reach lungs for exhalation). **Both external and internal respiration involve the movement of water and other substances as well (Capillary-Tissue exchange) – but here, in the Respiration Unit, we are focusing primarily on the driving force (gradient) behind the movement of gases. Transport of Gases in Blood OXYGEN: Oxygen binds loosely and therefore reversibly to hemoglobin (Hb) in RBCs. One Hb molecule can bind up to 4 O2 molecules Once this occurs, and it is saturated, it is referred to as oxyhemoglobin (HbO2). Hb + O2 HbO2 (at lungs) HbO2 Hb + O2 (at tissue cells) Hb = Deoxyhemoglobin (purplish) whereas HbO2 = Oxyhemoglobin (bright red). Within the lung capillaries, 98% of O2 joins Hb whereas 2% simply dissolves in the plasma (oxygen is fairly non-polar). Hb binds more readily to oxygen at a relatively cooler temperature (370 C) and a higher pH (7.40) – conditions that exist in the lung capillaries (since they are ‘closer’ to the outside of the body). (See fig. 15.9 p. 294) Once Hb has 1, 2, or 3 O2 molecules bound to it, its ‘attraction’ (affinity) for the 2nd, 3rd, and 4th molecule increases exponentially. Thus, all Hb molecules are saturated with O2. Conditions at the tissue cells are warmer (380 C) and more acidic (7.38 pH) than those in the lung capillaries. Hb tends to release an appreciable amount (~28%) of its O2 in these conditions. The difference in the affinity of Hb for O2 under different temp./pH conditions = the Bohr Shift. The ‘freed’ O2 then diffuses across the capillary walls into the ECF, and eventually into cells, following its PP gradient and traveling with water and other stuff (recall Tissue/Capillary Exchange). *label Bohr shift! TISSUES LUNGS During exercise, muscles heat up and produce lactic acid (decr. pH) which promotes Hb to give up even more of its O2 to the cells (sometimes up to 75%). INTERNAL SUFFOCATION – Carbon monoxide (CO) binds to Hb 200x more readily than O2. Thus, oxygen is prevented from reaching the tissue cells on any RBC ‘infested’ with CO. Therefore, the cells ‘suffocate’. CARBON DIOXIDE (CO2) CO2 is transported through the blood in three ways: 1. 70% is transported as the bicarbonate ion (HCO3-) in the plasma (more on this in a moment). 2. 23% attaches directly to Hb to form carbaminohemoglobin (HbCO2) CO2 + Hb @ TISSUES @ LUNGS HbCO2 The lower temp./higher pH in the lungs promotes CO2 release by Hb. The higher temp./lower pH at the tissue cells promotes CO2 uptake by Hb. 3. 7% simply dissolves in the plasma (as molecular CO2). ** Metaphor: Hb likes O2 in the winter (O2 is like a snowman) and hates O2 at the beach. CO2 is opposite…when Hb likes O2, it hates CO2, and vice versa… The ‘Beach’: ‘Winter’: Higher temperature, Lower pH Lower temperature, Higher pH O2 “snowman” Bicarbonate Ion Transport of CO2 As mentioned previously, 70% of the tissue cellproduced CO2 is transported in the plasma (dissolved) as HCO3-. HCO3- acts as a blood buffer. Once CO2 leaves tissue cells and enters the ECF, the blood, and eventually the RBCs, it reacts with water to form carbonic acid (H2CO3) which then dissociates slightly to form HCO3- and H+. CO2 + H2O H2CO3 H+ + HCO3- The RBC enzyme carbonic anhydrase acts to catalyze the first portion of this reaction and the higher tissue temperature promotes the 70% production of the final products. The HCO3- diffuse out of the RBCs (Cl- ions move into RBCs to balance the charge) and are carried in the plasma to the lungs, leaving H+ behind. The remaining H+ are picked up by Hb (or else the pH would severely drop – blood proteins would be denatured, as would vessel walls) to form reduced hemoglobin (HHb), which is carried within RBCs to the lungs. H+ + Hb HHb (at tissues, within RBCs). Thus, Hb acts to buffer the blood and keep it at, or near, its optimal pH. FYI: optimal blood pH = 7.4 due to the fact that HCO3is a better base than it is an acid and that there is a much higher concentration of it in the blood than CO2 and H2O (which, in combo, produce H2CO3). Once blood reaches the lungs, the HCO3- and H+ must be converted back to CO2 and water so that the majority of the CO2 can be expired. At the lower temp. and higher pH conditions in the lung capillaries, Hb gives up H+ (so that Hb can pick up O2), HCO3- diffuses back into the RBC (Clions diffuse back out), reacts with H+ to form H2CO3, which then forms CO2 and water; the CO2 then diffuses into the alveoli from the blood. Carbonic anhydrase helps again, but this time catalyzes the reverse reaction at the cooler temperature. Also, the diffusion of the other 30% of the CO2 into the alveoli drives the following reaction to the right: H+ + HCO3- H2CO3 CO2 + H2O See fig. 15.8 p. 293 for summary diagram Read pp. 295-298 (for interest only) – Respiratory Disorders…including figs. 15.10 p. 295 and 15.11 p. 296. Finished!!!