Module E Oxygen Transport and Internal - Macomb
advertisement
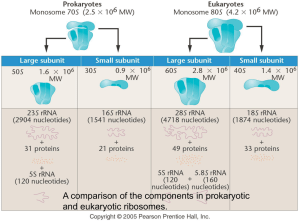
Oxygen Transport and Internal Respiration Module E Chapter 7 Malley Objectives • State the formula for calculating oxygen content. • Given a PaO2, calculate the amount of oxygen that is dissolved in plasma in vol%. • Describe the chemical structure of hemoglobin. • Describe the relationship between oxygen and hemoglobin in the presence of various factors. • List the abnormal species of hemoglobin. • Describe how hypoxia can result from ineffective cellular utilization of oxygen. Oxygen Transport • TWO WAYS TO CARRY OXYGEN • DISSOLVED IN PLASMA • COMBINED WITH HEMOGLOBIN • THE TOTAL AMOUNT OF OXYGEN PRESENT IS CALLED THE OXYGEN CONTENT. • ANY QUESTIONS? Dissolved Oxygen • Diffusion occurs because of a partial pressure difference between alveolus and capillary (gas to liquid). • The volume of gas that dissolves depends on the Solubility coefficient of the gas. • Higher solubility, more dissolved, regardless of partial pressure. • O2 dissolved in blood @ 37° C is .003 mL O2/100mL/mm Hg or • A normal individual will dissolve between 0.24 and 0.3 mL of oxygen/mL of blood at one atmosphere and 37° C. • Dissolved O2 (PaO2) represents 0.3 vol% • Linear relationship between PaO2 and the volume of oxygen dissolved • 0.3 vol% at 100mmHg PaO2, 0.6 vol% at 200 mmHg PaO2 Dissolved Oxygen – PaO2 • PaO2 does not tell us how much oxygen is in the blood. • Tells us about the potential driving pressure at a later point, but the volume (vol%) is the key issue. • Determined by PAO2, / relationships, level of ventilation and the AC membrane. • THINK ABOUT THE CAUSES OF HYPOXEMIA! Combined O2 • Dissolved oxygen is inadequate for metabolic needs. • Need a substance which will bind to oxygen and carry it, BUT will release it when needed. • Voila! Hemoglobin! • Miracle #2…Hemoglobin also carries carbon dioxide and is a key buffer of [H+]. Hemoglobin • Hemoglobin is composed of two groups: • Heme Group – Primarily iron in the Fe+2 (ferrous) state. • Globulin – 4 amino acid chains; • 2 alpha chains made up of 141 amino acids, • 2 beta chains made up of 146 amino acids. • Large molecule – GMW of 64,500 g. • One heme group binds with one of the amino acid chains and oxygen binds with the iron in the heme group in a reversible way. O2 + Fe+2 FeO2 Hemoglobin & the RBC • “Normal” hemoglobin level • 15 g/dl (men) & 13-14 g/dl (women) - Malley • 15 + 1.5 g/dl (men) & 13.5 + 1.5 g/dl (women) – Egan • 15 + 2 (men) & 14 + 2 (women) - Easy • Why do women have less? • The hemoglobin molecule resides in the erythrocyte and is responsible for giving the blood its red color. • Hundreds of hemoglobin variants. • Normal: A, A2, F • Abnormal: S, H Combined Oxygen • The affinity of hemoglobin for oxygen increases with each oxygen molecule attached • “All or Nothing” • Each gram of Hemoglobin combines with 1.34 mL of oxygen. • Oxygen Saturation only talks about how much hemoglobin is saturated, NOT how much hemoglobin is present. Oxygen Saturation • Saturation = Sites Filled Total Sites Available • Example: • 80 sites filled = 80% saturation 100 sites available Oxyhemoglobin Curve There is a direct (BUT NOT LINEAR) relationship between the dissolved oxygen in the blood (PO2) and the amount of oxygen that attaches to the hemoglobin (SO2). PO2 SO2 27 50 40 75 60 90 250 100 Significance of OHDC Shape • The steep line signifies that a small change in PO2 will yield a large change in SO2. • This is the dissociation portion of the curve. • Oxygen release is maximized. • A large amount of oxygen can be delivered to the tissues in times of compromised cardiovascular function or increased demands. • COPD patients “live” on the steep portion, small changes in PaO2 will yield greater changes in SaO2. • The flat line signifies that a large change in PO2 results in only a minimal increase in SO2. • This is the association portion of the curve. • Oxygen carrying is maximized. • The PO2 has to fall below 60 mm Hg before saturation becomes significantly affected. • Aging, High Altitudes P50 • The specific affinity of oxygen for hemoglobin can be assessed by evaluating at what PO2 there is a 50% SO2. • It is measured at 37° C, a PaCO2 40 mm Hg, pH 7.40. • Normal value is 27 mm Hg (25-27 mm Hg) • As P50 changes, we say the “curve has shifted”. Shifts in the OHDC • Left Shift • • • • Increased oxygen affinity for hemoglobin. This is the expected shift at the lungs (Left-Lungs) For any given PO2, SO2 will be higher. Decreasing P50 • Right Shift • • • • Decreased oxygen affinity for hemoglobin. This is the expected shift at the tissues. For any given PO2, SO2 will be lower. Increasing P50 Bohr Effect • The effect of CO2 on the OHDC is known as the Bohr Effect. (OH – Bohr) • High PCO2 levels and low pH decrease affinity of hemoglobin for oxygen (a right-ward shift) • This occurs at the tissues where a high level of PCO2 and acidemia contribute to the unloading of oxygen (and the attachment of CO2 to the unbound hemoglobin). • At the lungs, the high levels of oxygen facilitate the release of CO2 from the Hemoglobin molecule. This is known as the Haldane Effect. 2,3 DPG • 2,3 DPG is an organic phosphate normally found in RBC, that has a tendency to bind with Hemoglobin and thereby decrease the affinity of Hemoglobin for oxygen. • It promotes a rightward shift and enhances oxygen unloading at the tissues. This shift is longer in duration than that due to [H+], PCO2 or temperature. • A doubling of DPG will result in a 10 torr increase in P50. • The levels increase with cellular hypoxia. • • • • Anemia Hypoxemia secondary to COPD. Congenital Heart Disease Ascent to high altitudes • The levels are reduced with • Septic Shock • Acidemia • STORED BLOOD in ACD: NO DPG after 2 weeks of storage. Oxygen Content • The total amount of oxygen present in the blood. • CaO2 = (Hb * 1.34 * SaO2) + ( PaO2 * 0.003) • C O2 = (Hb * 1.34 * S O2) + ( P O2 * 0.003) • The difference between the two (C(a- )O2) is approximately 5 vol%. • The Fick equation describes the relationship between the cardiac output, the oxygen consumption and the C(a- )O2. • CO * C(a- )O2 = O2 • 5,000 mL/min * 5 mL O2/100 ml = 250 mL O2/min Cyanosis • A clinical condition manifested by a bluish discoloration of the mucous membranes or nail beds. • Peripheral vs. Central • Present when 5 g/dl of hemoglobin is desaturated. • This usually correlates with a SaO2 below 85%. • Calculated as follows: [(Hb * Arterial Desaturation) + (Hb * Venous Desaturation)] /2 • Normal Arterial Desaturation is 100% - 98% or 2%. • Normal Venous Desaturation is 100% - 75% or 25%. [(15 * .02) + (15 * .25)] /2 = [.3 +3.75] / 2 = 4.05/2 = 2.025g% • ANEMIC PATIENTS WILL NEVER BE CYANOTIC! Oxygen Transport • The volume of oxygen leaving the left ventricle each minute. • CaO2 * CO = 20 ml O2/100 mL * 5,000 mL/min • 1,000 mL O2 / min • If oxygen consumption is 250 mL O2 / min, then we “extract” 25% of the total. • This can also be determined by dividing the C(a- )O2 by the CaO2. (5 vol% / 20 vol%) = .25 • Key factors are the PaO2, SaO2, SV, & HR Hemoglobin Abnormalities • • • • • Carboxyhemoglobin Sulfhemoglobin Fetal Hemoglobin Methemoglobin Hemoglobin S Carboxyhemoglobin • Carbon Monoxide has 245 times the affinity for hemoglobin as oxygen. • Causes a leftward shift (increased affinity of Oxygen) • Normal level is less than 3% • 10% is common with smokers. • Toxic at 20%; Lethal at 50%. • Venous HbCO = Arterial HbCO (Ann Emerg Med. 1995 Apr;25(4):481-3) • Suspect incomplete combustion if level is elevated. • Furnace, space heater • Treatment is 100% oxygen • Reduces half-life of HbCO from 5 hours to 20 minutes. • Hyperbaric treatment remains controversial. Methemoglobin • • • • A normal variant of adult hemoglobin. Ferrous to Ferric (loses an electron, Fe+3) Normal levels are less than 1%. Usually associated with excessive nitrate ingestion. • • • • Amyl Nitrate Nitroglycerine Nipride Topical anesthetics • Blood will appear rusty or brown in color. • Treatment with methylene blue Sulfhemoglobin • Sulfhemoglobin results from the union of hemoglobin with medications such as phenacetin (sedative no longer used) or sulfonamides (antibiotics including Bactrim & Septra). • The resultant form of hemoglobin is unable to transport oxygen, and is untreatable. • The only treatment is to wait until the affected red blood cells are destroyed as part of their normal life cycle. Fetal Hemoglobin (HbF) • Fetal hemoglobin (hemoglobin F) is the main hemoglobin that transports oxygen around the body of the developing baby during the last 7 months of pregnancy. • It has a greater affinity for oxygen than Hemoglobin A (P50 of 20 mm Hg). • At about 30 weeks gestation, the fetus begins to make increasing amounts of hemoglobin A. • Hemoglobin F does not turn into hemoglobin A. • As they grow babies automatically turn off the production of hemoglobin F (usually complete by one year). Failure to stop Hemoglobin F production is found in certain beta thalassemias. Possible link to SIDS. Hemoglobin S • Hemoglobin S is a abnormal variant of Hemoglobin A where one of the 146 amino acids in the beta chain is altered. • Inherited disorder from both parents. • 1% of African Americans. • Recurrent painful episodes (Crisis) occur as sickled cells become obstructed. • Typical “anemic” symptoms. • Can lead to infections and stroke.