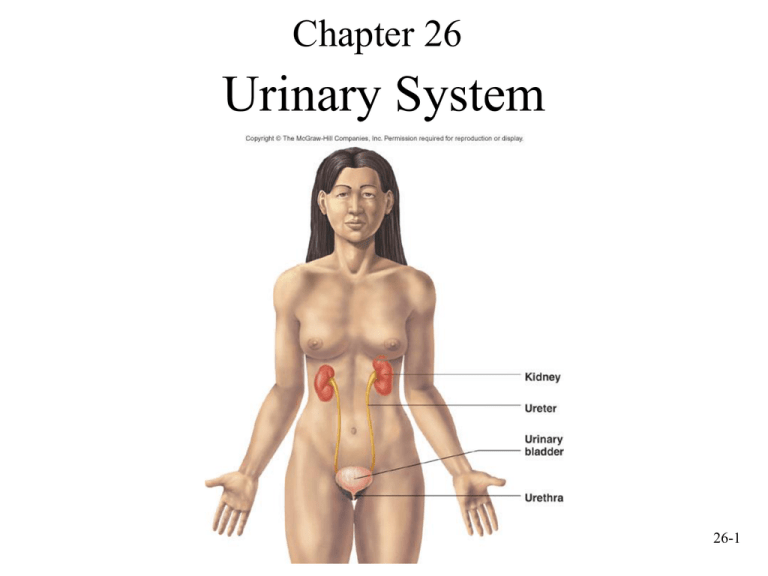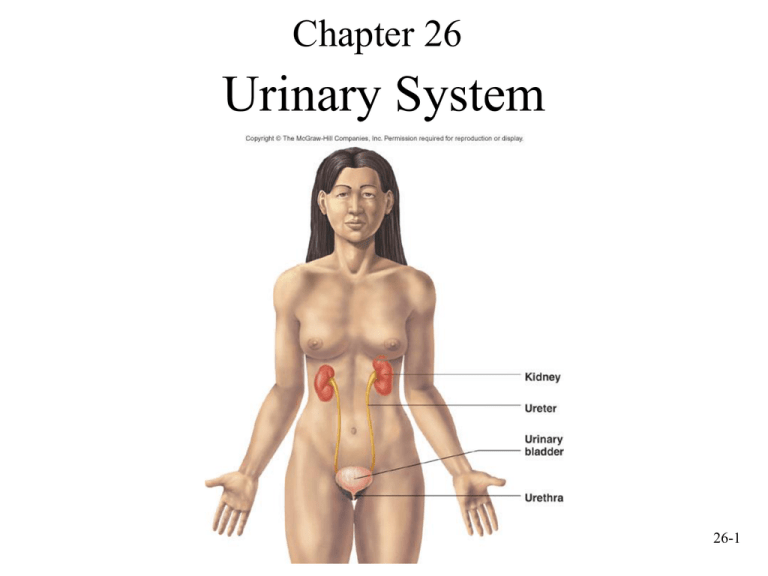
Chapter 26
Urinary System
26-1
Urinary System Functions
• Filtering of blood: involves three processesfiltration, reabsorption, secretion.
• Regulation of
– Blood volume
– Concentration of blood solutes: Na+, Cl-, K+, Ca2+,
HPO4-2
– pH of extracellular fluid: secrete H+
– Blood cell synthesis (kidneys secrete hormone,erythropoietin)
• Synthesis of vitamin D
26-2
Urinary System Anatomy
26-3
Location and External Anatomy
of Kidneys
• Location
– Lie behind peritoneum
(retroperitoneal) on
posterior abdominal wall
on either side of vertebral
column
– Lumbar vertebrae and rib
cage partially protect
– Right kidney slightly lower
than left
• External Anatomy
– Renal capsule: fibrous connective
tissue. Surrounds each kidney
– Perirenal fat
• Engulfs renal capsule and acts as
cushioning
– Renal fascia: thin layer loose
connective tissue
• Anchors kidneys and surrounding
adipose to abdominal wall
– Hilum
• Renal artery and nerves enter and
renal vein and ureter exit kidneys
• Opens into renal sinus (cavity
filled with fat and loose connective
tissue)
26-4
Internal Anatomy of Kidneys
• Cortex: outer area
– Renal columns: part of
cortical tissue that extends into
medulla
• Medulla: inner area; surrounds
renal sinus
– Renal pyramids: cone-shaped.
Base is boundary between
cortex and medulla. Apex of
pyramid is renal papilla,
points toward sinus.
• Calyces
– Minor: papillae extend into
funnel of minor calyx
– Major: converge to form
pelvis
• Pelvis: enlarged chamber
formed by major calyces
• Ureter: exits at the hilum;
connects to urinary bladder
26-5
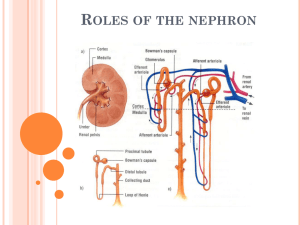
The Nephron
• Functional and histological unit
of the kidney
• Parts of the nephron:
Bowman’s capsule, proximal
tubule, loop of Henle
(nephronic loop), distal
tubule
• Urine continues from the
nephron to collecting ducts,
papillary ducts, minor
calyses, major calyses, and the
renal pelvis
• Collecting ducts, parts of the
loops of Henle, and papillary
ducts are in the renal medulla
26-6
Types of Nephrons
• Juxtamedullary nephrons.
Renal corpuscle near the
cortical medullary border.
Loops of Henle extend deep
into the medulla.
• Cortical nephrons. Renal
corpuscle nearer to the
periphery of the cortex. Loops
of Henle do not extend deep
into the medulla.
• Renal corpuscle. Bowman’s
capsule plus a capillary bed
called the glomerulus.
26-7
Renal Corpuscle
• Bowman’s capsule:
outer parietal (simple
squamous epithelium)
and visceral (cells
called podocytes)
layers.
• Glomerulus: network
of capillaries. Blood
enters through afferent
arteriole, exits through
efferent arteriole.
26-8
Bowman’s Capsule
• Parietal layer: outer.
Simple squamous
epithelium that becomes
cube-shaped where
Bowman’s capsule ends
and proximal tubule
begins
• Visceral layer: inner.
Specialized podocytes that
wrap around the
glomerular capillaries
26-9
Filtration Membrane
• Fenestrae: window-like openings in
the endothelial cells of the
glomerular capillaries.
• Filtrations slits: gaps between the
cell processes of the podocytes.
Basement membrane sandwiched
between the endothelial cells of the
glomerular capillaries and the
podocytes.
• Filtration membrane: capillary
endothelium, basement membrane
and podocytes. First stage of urine
formation occurs here when fluid
from blood in capillaries moves
across filtration membrane into the
lumen inside Bowman’s capsule.
26-10
Circulation in the Glomerulus
•
•
•
•
Afferent arteriole: supplies blood to glomerulus
Efferent arteriole: drains glomerulus
Both vessels have a layer of smooth muscle
Juxtaglomerular apparatus: sight of renin production
– Juxtaglomerular cells- ring of smooth muscle in the afferent
arteriole where the latter enters Bowman’s capsule
– Macula densa- Specialized tubule cells of the distal tubule. The
distal tubule lies between the afferent and efferent arterioles.
26-11
Histology of the Nephron
• Proximal tubule: simple cuboidal
epithelium with many microvilli
• Loops of Henle
– Descending limb: first part
similar to proximal tubule.
Latter part simple squamous
epithelium and thinner
– Ascending limb: first part
simple squamous epithelium
and thin, distal part thicker and
simple cuboidal
• Distal tubule: shorter than
proximal tubule. Simple cuboidal,
but smaller cells and very few
microvilli
• Collecting ducts: form where
many distal tubules come together.
Larger in diameter, simple
cuboidal epithelium. Form
medullary rays and lead to
papillary ducts
26-12
Circulation Through the Kidney
Arterial supply:
1. Renal arteries branch
from abdominal aorta
2. Segmental arteries
branch from renal
3. Interlobar arteries
ascend within renal
columns toward cortex
4. Arcuate arteries
branch and arch over
the base of the pyramids
5. Interlobular arteries
project into cortex and
give rise to afferent
arterioles
26-13
Circulation Through the Kidney
•
The part of the circulation
involved with urine formation
6. Afferent arterioles supply
blood to glomerulus
7. Glomerulus
8. Efferent arterioles exit the
renal corpuscle
9. Peritubular capillaries form a
plexus around the proximal and
distal tubules
10. Vasa recta (loop of henle):
specialized parts of peritubular
capillaries that course into
medulla along with loops of
Henle, then back toward cortex
26-14
Circulation Through the Kidney
• Venous drainage
11. Peritubular
capillaries (PCT) drain
into interlobular veins
and lead to
12. Arcuate veins
13. Interlobar veins
14. Renal veins
26-15
Urine Formation
Nephrons considered functional units of the kidney: smallest
structural component capable of producing urine
26-16
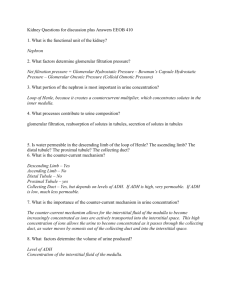
Filtration
• Movement of fluid, derived from blood flowing through the
glomerulus, across filtration membrane
• Filtrate: water, small molecules, ions that can pass through
membrane (large molecules = blood cells & protein-------do not pass)
• Pressure difference forces filtrate across filtration membrane
• Renal fraction: part of total cardiac output that passes through the
kidneys. Varies from 12-30%; averages 21%
• Renal blood flow rate: 1176 mL/min
• Renal plasma flow rate: renal blood flow rate X fraction of blood
that is plasma: 650 mL/min (1176 ml/min x 0.55 = 646.8 ml plasma/min)
• Filtration fraction: part of plasma flowing through the kidney that
is filtered into lumen of Bowman’s capsules; average 19%
( 650 ml plasma/min x 0.19 = 123.5 ml plasma/min---------125 ml/min of filtrate)
• Glomerular filtration rate (GFR): amount of filtrate produced
each minute. 180 L/day
• Average urine production/day: 1-2 L. Most of filtrate must be 26-17
reabsorbed
26-18
Filtration
• Filtration membrane: filtration barrier. It prevents blood cells and proteins
from entering lumen of Bowman’s capsule, but is many times more permeable
than a typical capillary
– Fenestrated endothelium, basement membrane and pores formed by
podocytes
– Some albumin and small hormonal proteins enter the filtrate, but these are
reabsorbed and metabolized by the cells of the proximal tubule. Very little
protein normally found in urine
• Filtration pressure: pressure gradient responsible for filtration; forces fluid
from glomerular capillary across membrane into lumen of Bowman’s capsules
• Forces that affect movement of fluid into or out of the lumen of Bowman’s
capsule
– Glomerular capillary pressure (GCP): blood pressure inside capillary
tends to move fluid out of capillary into Bowman’s capsule
– Capsule pressure (CP): pressure of filtrate already in the lumen
– Blood colloid osmotic pressure (BCOP): osmotic pressure caused by
proteins in blood. Favors fluid movement into the capillary from the
lumen. BCOP greater at end of glomerular capillary than at beginning
because of fluid leaving capillary and entering lumen
– Filtration pressure (10 mm Hg) = GCP (50 mm Hg) – CP (10 mm Hg) –26-19
BCOP (30 mm Hg)
Filtration Pressure
26-20
Filtration
• Colloid osmotic pressure in Bowman’s capsule normally close to
zero. During diseases like glomerular nephritis, proteins enter
the filtrate and filtrate exerts an osmotic pressure, increasing
volume of filtrate
• Filtrate is forced across filtration membrane; fluid moves into
peritubular capillaries from interstitial fluid
• Changes in afferent and efferent arteriole diameter alter filtration
pressure
– Dilation of afferent arterioles/constriction efferent arterioles increases
glomerular capillary pressure, increasing filtration pressure and thus
glomerular filtration
26-21
Autoregulation and
Sympathetic Stimulation
• Autoregulation
– Involves changes in degree of constriction in afferent
arterioles
– As systemic BP increases, afferent arterioles constrict and
prevent increase in renal blood flow (opposite also occurs)
– Increased rate of blood flow of filtrate past cells of macula
densa: signal sent to juxtaglomerular apparatus, afferent
arteriole constricts
• Sympathetic stimulation: norepinephrine
– Constricts small arteries and afferent arterioles
– Decreases renal blood flow and thus filtrate formation
– During shock or intense exercise: intense sympathetic
stimulation, rate of filtrate formation drops to a few ml
*Note: Glomerular filtration rate is relatively constant as B.P. changes 26-22
between 90 & 180 mmHg.
Tubular Reabsorption: Overview
• Tubular reabsorption: occurs as filtrate flows through
the lumens of proximal tubule, loop of Henle, distal
tubule, and collecting ducts
• Results because of
–
–
–
–
–
Diffusion
Facilitated diffusion
Active transport
Symport
Osmosis
• Substances transported to interstitial fluid and
reabsorbed into peritubular capillaries: inorganic salts,
organic molecules, 99% of filtrate volume. These
substances return to general circulation through venous
26-23
system
Reabsorption in Proximal
Convoluted Tubule
• Substances pass through cells of tubule
wall. Each cell has
– Apical surface: surface that faces
filtrate. Apical membrane
– Basal surface: faces interstitial fluid.
Basal membrane
– Lateral surfaces: surfaces between
cells
• Active transport of Na+ across the basal
membrane from cytoplasm to interstitial
fluid linked to reabsorption of most solutes
•Because of active transport, the concentration of Na+ is low inside the cell and
Na+ moves into nephron cell from filtrate through the apical membrane. Other
substances moved by symport from the filtrate into the nephron cell are substances
that should be retained by the body
•Substances transported
–Through apical membrane: Na+, Cl-, glucose, amino acids, and water.
–Through basal membrane: Na+, K+,
Cl-, glucose, amino acids, water
26-24
Reabsorption in Proximal
Convoluted Tubule
• Number of carrier molecules
limits rate of transport
• In diabetes mellitus
– Concentration of glucose in filtrate
exceeds rate of transport
– High concentration of glucose in
plasma (and thus in filtrate) reflected
in glucose in the urine
• Diffusion between cells: from
lumen of nephron into interstitial
fluid
– Depends on rate of transport of some
solutes through the cells of the tubule
– K+, Ca2+, and Mg2+
• Filtrate volume reduced by 65%
due to osmosis of water
26-25
Reabsorption in Loop of Henle
• Loop of Henle descends into
medulla; interstitial fluid is high
in solutes.
• Descending thin segment is
highly permeable to water and
moderately permeable to urea,
sodium, most other ions
(passive).
• Water moves out of nephron,
solutes in. Volume of filtrate
reduced by another 15%.
• Ascending thin segment is not
permeable to water, but is
permeable to solutes. Solutes
diffuse out of the tubule and
into the more dilute interstitial
fluid as the ascending limb
projects toward the cortex.
Solutes diffuse into the
descending vasa recta.
26-26
Reabsorption in Loop of Henle
• The wall of the ascending limb of
the loop of Henle is not permeable
to water. Na+ moves across the wall
of the basal membrane by active
transport, establishing a
concentration gradient for Na+. K+
and Cl- are symported with Na
across the apical membrane and ions
pass by facilitated diffusion across
the basal cell membrane of the
tubule cells.
• At the end of the loop of Henle,
inside of nephron concentration of
solutes is 100 mOsm/kg (milli-osmole
per kilogram). Interstitial fluid in the
cortex is 300mOsm/kg. Filtrate
within DCT is much more dilute
than the interstitial fluid which
surrounds it.
26-27
Reabsorption in Distal Convoluted Tubule
and Collecting Duct
• Active transport of Na+ out of tubule cells into interstitial fluid
with cotransport of Cl• Na+ moves from filtrate into tubule cells due to concentration
gradient
• Collecting ducts extend from cortex (interstitial fluid 300
mOsm/kg) through medulla (interstitial fluid very high)
• Water moves by osmosis from distal tubule and collecting duct
into more concentrated interstitial fluid
• Permeability of wall of distal tubule and collecting ducts have
variable permeability to water
• Urine can vary in concentration from low volume of high
concentration to high volume of low concentration
26-28
Changes in Concentration of
Solutes in the Nephron
• Urea: enters glomerular filtrate.
– As volume of filtrate decreases (approx. 99% H2O is reabsorbed),
concentration of urea increases
– Walls of nephron not very permeable to urea: only 4060% passively reabsorbed
• Urate ions, creatinine, sulfates, phosphates, nitrates
partially reabsorbed
– Concentration is high in urine
– Toxic substances and are eliminated
26-29
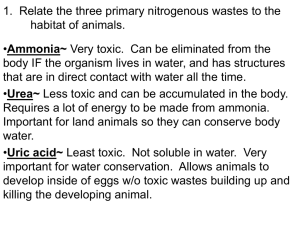
Tubular Secretion
• Moves metabolic by-products, drugs, molecules
not normally produced by the body into tubule of
nephron
• Active or passive
• Ammonia: produced by epithelial cells of nephron
from deamination of amino acids. Diffuses into
lumen
• H+, K+, penicillin, and substances such as paraaminohippuric acid (PAH): actively secreted into
nephron
26-30
Secretion of Hydrogen and Potassium
A. Hydrogen ions secreted into
filtrate by countertransport in
proximal tubule
– H+ either diffuse from
peritubular capillaries into
interstitial fluid and then into
epithelial cells of tubule or
derived from reaction between
carbon dioxide and water in
cells of tubule.
– Na+ and HCO3- cotransported
across basal membrane into
interstitial fluid, then diffuse
into peritubular capillaries
26-31
Secretion of Hydrogen and Potassium
B. H+ and K+ secreted into
filtrate by countertransport
in distal tubule. Na+ and K+
move by active transport
across the basal membrane.
Na+ and HCO3cotransported across basal
membrane into interstitial
fluid, then diffuse into
peritubular capillaries
26-32
Urine Production
• In Proximal convoluted
tubules
– Na+ and other substances
removed
– Water follows passively
– Filtrate volume reduced
• In descending limb of loop
of Henle
– Water exits passively, solute
enters
– Filtrate volume reduced 15%
• In ascending limb of loop of
Henle
– Na+, Cl-, K+ transported out of
filtrate
– Water remains
• In distal convoluted tubules
and collecting ducts
– Water movement out regulated
by ADH
• If absent, water not
reabsorbed and dilute urine
produced
• If ADH present, water moves
out, concentrated urine
produced
26-33
Urine Concentration Mechanism
• When large volume of water consumed
– Eliminate excess without losing large amounts of
electrolytes
– Response is that kidneys produce large volume of dilute
urine
• When drinking water not available
– Kidneys produce small volume of concentrated urine
– Removes waste and prevents rapid dehydration
• Mechanisms that create urine of variable concentration
– Maintenance of high concentration of solutes in medulla
– Countercurrent functions of loops of Henle
– Control of permeability of distal nephron to water
26-34
Medullary Concentration Gradient
• In order to concentrate urine (and prevent a large
volume of water from being lost), the kidney must
maintain a high concentration of solutes in the
medulla
• Interstitial fluid concentration (mOsm/kg) is 300
in the cortical region and gradually increases to
1200 at the tip of the pyramids in the medulla
• Maintenance of this gradient depends upon
– Functions of loops of Henle
– Vasa recta flowing countercurrent to filtrate in loops of
Henle
– Distribution and recycling of urea
26-35
Creating/Maintaining High Solute
Concentration in Medulla
• Active transport of Na+ and cotransport of ions such as K+ and
Cl- and other ions out of the thick portion of ascending limb into
interstitial fluid
• Impermeability of thin and thick parts of ascending limb of loop
of Henle to water
• Vasa recta remove excess water and solutes that enter the
medulla without destroying the high concentration of solutes in
interstitial fluid of medulla
• Active transport of ions from collecting ducts into interstitial
fluid of medulla
• Passive diffusion of urea from collecting ducts into interstitial
fluid of medulla, impermeability of the ascending limb and
permeability of the descending limb of the loops of Henle to
26-36
urea
Loops of Henle
• Juxtamedullary nephrons:
long loops.
– Walls of descending limbs
permeable to water, water
moves out into interstitial fluid
– Walls of ascending limb
impermeable to water
– Solute diffuses out of thin
segment of ascending limb as
it passes though progressively
less concentrated interstitial
fluid
– Na+, K+ and Cl- actively
transported out of ascending
limb into interstitial fluid
– Thus, water enters interstitial
fluid from descending limbs
and solutes enter interstitial
fluid from ascending limbs
26-37
Vasa Recta
• Countercurrent systems that remove
excess water and solutes from medulla:
parallel tubes in which fluid flows, but in
opposite directions
• Blood flows through vasa recta to the
medulla, vessels turn near tip of renal
pyramid, then blood flows in opposite
direction
• Walls are permeable to water and to
solutes: as blood flows toward medulla,
water moves out, solutes diffuse in. As
blood flows back toward cortex, water
moves into vasa recta, some solutes
diffuse out
• Diffusion is such that slightly more
water and slightly more solute are
carried from the medulla by the vasa
recta than enter it
26-38
• Loops of Henle and vasa recta function
together to maintain a high concentration
of solutes in the interstitial fluids of the
medulla and to carry away the water and
solutes that enter the medulla from the
loops of Henle and collecting ducts
– Water moves out of descending limb
and enters vasa recta
– Solutes diffuse out of ascending thin
segment and enter vasa recta, but
water does not
– Solutes transported out of thick
segment of ascending enter the vasa
recta
– Excess water and solutes carried
away from medulla without reducing
high concentration of solutes
– Concentration of filtrate reduced to
100 mOsm/kg by the time it reaches
distal tubule
26-39
• Water and solutes
move out of the
collecting duct into
the vasa recta
26-40
Urea
• Responsible for large part of
high osmolality in medulla
• Descending limbs of loops of
Henle permeable to urea;
urea diffuses into interstitial
fluid
• Ascending limbs and distal
tubules impermeable to urea
• Collecting ducts permeable to
urea; some diffuses out into
interstitial fluid
• Urea flows in a cycle
maintaining high urea
concentration in medulla
26-41
Urine Concentrating Mechanisms
26-42
Renin/Angiotensin/Aldosterone
26-43
ADH and the Nephron
26-44
ADH and the Nephron
26-45
Other Hormones
• Atrial natriuretic hormone
– Produced by right atrium of heart when blood volume
increases stretching cells
– Inhibits Na+ reabsorption
– Inhibits ADH production
– Increases volume of urine produced
– Venous return is lowered, volume in right atrium
decreases
• Prostaglandins and kinins: produced in kidney.
Role unclear
26-46
Clearance and Tubular Maximum
• Plasma clearance: calculated using substances
like inulin
– Volume of plasma cleared of a specific substance each
minute
– Used to estimate GFR
– Used to calculate renal plasma flow. Calculated using
substances like PAH
– Used to determine which drugs or other substances
excreted by kidney
• Tubular load
– Total amount of substance that passes through filtration
membrane into nephrons each minute
26-47
Tubular
Maximum
• Maximum rate at which a
substance can be actively
absorbed
– Each substance has its own
tubular maximum
– Normally, glucose
concentration in the plasma
(and thus filtrate) is lower
than the tubular maximum
and all of it is reabsorbed;
none of it is found in the
urine
– In diabetes mellitus tubular
load exceeds tubular
maximum and glucose
appears in urine. Urine
volume increases because
glucose in filtrate increases
osmolality of filtrate
reducing the effectiveness
of water reabsorption
26-48
Urine Movement
• Hydrostatic pressure forces urine through
nephron
• Peristalsis moves urine through ureters from
region of renal pelvis to urinary bladder.
Occur from once every few seconds to once
every 2-3 minutes
– Parasympathetic stimulation: increase
frequency
– Sympathetic stimulation: decrease frequency
• Ureters enter bladder obliquely through
trigone. Pressure in bladder compresses
ureter and prevents backflow
26-49
Anatomy and Histology of Ureters and Bladder
• Ureters: bring urine from
renal pelvis to urinary
bladder. Lined by transitional
epithelium
• Urinary bladder: hollow
muscular container. In pelvic
cavity posterior to symphysis
pubis. Lined with transitional
epithelium; muscle part of
wall is detrusor
•Trigone: interior of urinary bladder. Triangular area between the
entry of the two ureters and the exit of the urethra. Area expands
less than rest of bladder during filling
26-50
Anatomy and Histology of Urethra
• Male: extends from the inferior
part of the urinary bladder
through the penis
• Female: shorter; opens into
vestibule anterior to vaginal
opening
• Internal urinary sphincter: in
males, elastic connective tissue
and smooth muscle keep semen
from entering urinary bladder
during ejaculation
• External urinary sphincter:
skeletal muscle surrounds
urethra as it extends through
pelvic floor. Acts as a valve
26-51
Micturition Reflex
26-52
Effects of Aging
• Gradual decrease in size of kidneys, but only onethird of one kidney necessary for homeostasis
• Amount of blood flowing through gradually
decreases
• Number of glomeruli decrease and ability to
secrete and reabsorb decreases
• Ability to concentrate urine declines and kidney
becomes less responsive to ADH and aldosterone
• Reduced ability to participate in vitamin D
synthesis contributing to Ca2+ deficiency,
osteoporosis, and bone fractures
26-53