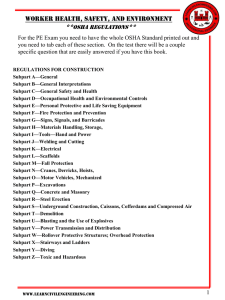
Details of CLIA Final QC
Regulatory Changes
Division of Laboratory Services
CMS
Overview
Consolidates Subpart J, K, and P into:
– J-Facility Administration for Nonwaived
Testing.
– K-Quality System for Nonwaived Testing.
– Creates one set of Nonwaived requirements.
– Parallels the flow of a specimen through the
laboratory.
– Reflects the Total Testing Process:
•
•
•
•
General Laboratory Systems
Preanalytic Systems
Analytic Systems
Postanalytic Systems
Subpart A
General Provisions
Revisions:
– Definitions for calibration, FDA-cleared or
approved, reportable range & test system.
– Replaced National Institute for Drug Abuse
(NIDA) with Substance Abuse & Mental
Health Services Administration (SAMHSA).
Subpart I
Proficiency Testing
Revisions:
– Changed consensus for PT program grading
from 90% to 80%.
• Reduces number of ungradables.
• Permits labs to “get more for their money”.
• Facilitates better laboratory education; e.g., error ID
& correction.
Subpart J
Facility Administration
Revisions:
– Applies to moderate & high testing.
– Facility requirements.
• Safety precautions are accessible.
• Uni-directional workflow for molecular
amplification procedures.
• Comply w/ Federal, State & local laws.
Subpart J
Facility Administration
Revisions:
– Transfusion Services
• Report transfusion reactions/fatalities to laboratory
& authorities.
– Record/Specimen Retention
• Preservation.
• Record retention for closed facilities.
• Keep test procedure & performance specifications
for 2 years after use.
Subpart K
Quality System
Applies to moderate & high testing.
– General Laboratory Systems.
– Preanalytic Systems.
– Analytic Systems.
– Post analytic Systems.
• Emphasizes Quality Assessment.
Subpart K
Quality System
Quality assessment (QA) requirements
–
–
–
–
–
Monitor and assess quality.
Correct problems.
Review effectiveness of correction.
Discuss with staff.
Document assessment activities.
Included in each phase of testing
Subpart K
Quality System
General laboratory Systems:
–
–
–
–
–
–
Confidentiality of patient information.
Specimen identification & integrity.
Complaint investigations.
Communications.
Personnel Competency Assessment Policies.
Evaluation of PT performance.
Subpart K
Quality System
Evaluation of PT Performance:
Verify accuracy of:
- Tests w/ no evaluation or score.
- Tests when PT score doesn’t reflect test
performance.
- Any test not included in Subpart I.
- Regulated analytes for which compatible PT
material isn’t available from PT providers twice
a year.
Subpart K
Quality System
Preanalytic Systems
Test request:
– Solicit patient’s gender, age or DOB.
– Solicit specimen source, when appropriate.
Specimen submission, handling and referral:
– Date and time of receipt in laboratory.
Subpart K
Quality System
Analytic Systems
Procedure Manual:
– Director must sign procedures & changes prior
to use.
– Retain test procedures with the dates of initial
use and discontinuance.
Subpart K
Quality System
Analytic Systems
Test systems, equipment, instruments, reagents,
materials, and supplies:
– Removed the FDA product dating information
to guidelines.
– Follow manufacturer’s instructions for storage
of reagents, specimens & test systems.
Subpart K
Quality System
Analytic Systems
Maintenance and function checks:
– Follow manufacturer’s instructions for
maintenance & function checks.
Calibration and calibration verifications:
– Provides flexibility for calibration verification
material.
Subpart K
Quality Systems
Analytic Systems
Establishment and Verification of Performance
Specifications:
– Applies to new or modified nonwaived tests.
– Verify/establish accuracy, precision, reportable
range.
– Verify/establish manufacturer’s normal values.
– Determine calibration & control procedures.
– Establish analytical sensitivity & specificity.
Subpart K
Quality System
Analytic Systems
Control Procedures:
– Detect immediate errors and monitor over time.
– Requires a control system capable of detecting
reaction inhibition for molecular amplification.
– Test 2 controls/day or acceptable alternative.
– Use of calibrators as controls.
– Rotate QC testing among all operators.
Subpart K
Quality System
Analytic Systems
Bacteriology:
– Check each batch, lot number and shipment of reagents,
disks, stains, antisera, and identification systems when
prepared or opened for positive and negative reactivity
(and graded reactivity, if applicable).
• Less stringent for catalase, Cefinase,Tm coagulase,
oxidase, bacitracin, optochin, ONPG, X,V and XV
disks or strips
– Check each batch, lot number and shipment of antisera
for positive and negative reactivity when prepared or
opened, and once every 6 months thereafter.
• Less stringent
Subpart K
Quality System
Analytic Systems
Mycobacteriology:
– Check fluorochrome acid-fast stains for
positive and negative reactivity each time of
use.
• More stringent
– Check acid-fast stains for positive and negative
reactivity each day of use.
• More stringent
– Each day of use check all reagents, test
procedures for mycobacterial identification
using positive and negative acid-fast organisms.
• More stringent
Subpart K
Quality System
Analytic Systems
Mycology:
– Check each batch, lot number and shipment of reagents
and fungal identification tests (germ tube) when
prepared or opened for positive and negative reactivity
(and graded reactivity, if applicable).
• Less stringent - frequency
• More stringent - added negative control
– Check each batch, lot number and shipment of
lactophenol cotton blue when prepared or opened for
intended reactivity with a control organism(s).
• Less stringent
Subpart K
Quality System
Analytic Systems
Parasitology:
– No changes.
Virology:
– No changes.
Routine Chemistry:
– No changes.
Subpart K
Quality System
Analytic Systems
Syphilis Serology and Immunology:
– Control testing reduced to each day of testing.
Hematology:
– Reduced automated hematology QC to
once/day.
– Manual hematology requires QC each 8 hours
of testing.
– No change to QC for coagulation (manual or
automated).
Subpart K
Quality System
Analytic Systems
Immunohematology:
– Includes only specific cites for FDA BB
(21 CFR) requirements under CLIA.
Histopathology:
– Check immunohistochemical stains for positive
& negative reactivity each time of use.
– Allows individuals trained in neuromuscular
pathology to report neuromuscular path results.
Subpart K
Quality System
Analytic Systems
Cytology:
– Workload limit for liquid-based slide
preparatory techniques reduced from 200 to
100 for gynecologic preparations.
– Provision for automated, semi-automated
screening devices added to require
manufacturer’s instructions (including
individual workload limits) be followed.
Subpart K
Quality System
Analytic Systems
Clinical Cytogenetics:
– Resolution is appropriate for type of tissue or
specimen & study required based on clinical
information provided.
– Requires full chromosome analysis for sex
determination.
– Utilize the International System of Cytogenetic
Nomenclature on report.
Subpart K
Quality System
Analytic Systems
Histocompatibility:
– Requires in-house prepared reagent typing
inventory to indicate reagent specificity.
– Requires a technique that detects HLA specific
antibody w/ a specificity equivalent or superior
to the basic microlymphocytotoxicity assay.
– Requires using a method that distinguishes
antibodies to HLA class II antigens from
antibodies to Class I antigens.
Subpart K
Quality System
Analytic Systems
Histocompatibility cont’d:
– Have available monthly specimens for periodic
antibody screening & crossmatch on all
potential transplant recipients; and develop a
policy consistent w/ clinical transplant
protocols for frequency of such antibody
screening.
– Define test protocols for each type of cell,
tissue or organ to be transfused or transplanted.
Subpart K
Quality Systems
Analytic Systems
Histocompatibility cont’d:
– Follow policies that address when HLA testing
& final crossmatches are required for presensitized non-renal transplant recipients.
– Establish technique to optimally define HLA
Class I & II specificity.
– Eliminates monthly evaluation of a specimen as
an unknown by each testing person.
Subpart K
Quality System
Postanalytic Systems
Test Report:
– State date of test report on report & include
specimen source, if applicable.
– Include name & ID no. or unique patient
identifier & ID no.
Subpart M
Personnel
Applies only to doctoral degree (non-MD)
qualifications:
– Represents only remaining complexitydependent requirements.
– As of 2/24/03 “grandfathers” individuals
currently as high complexity directors.
– Requires board certification for new directors.
– Approved Boards to be listed in Appendix C of
Surveyor Guidelines and on website.
CLIA FINAL QC REGULATIONS
CONTACT INFORMATION:
– CMS WEB SITE: www.cms.hhs.gov/clia
– CMS LAB DIVISION: 410-786-3531(phone)
410-786-1224 (fax)
THE END
THANK YOU!!
QUESTIONS????