Renal
advertisement

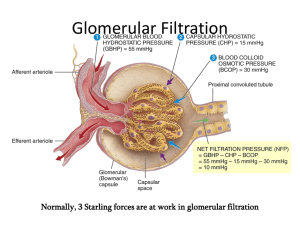
Renal system Factors Measurements Renal blood Nephrons Glomerular Functions affecting ofcapillary supply kidney of GFR GFRmembrane and RBF Kidney consists of 8-10 conical pyramids, bases in outer =cortex, apices toward pelvis, medulla subdivGFR Structural Kf *&filtration (net functional ultrafiltration units, more pressure) than million, in Measurement RBF: increases ofGFR RBF Glomerular GFR rate ﴾GFR﴿ Regulation Substance Three layers: used of capillary ECF to measure vol., endothelium, osmolarity GFR & & RBF BM composition, must: & visceral supplies renal ﴿ 1.25 L\min ﴾ 25% of cardiac output idedincreases into &(Cx) zones, outer zone into outer each kidney, =clearance Kfouter * (PG composed +inner ΠB=–of PB the - –ΠG) following structures: RBF FF: = RPF \(creatinine) (1-hematocrit) GFR Endogenous or exogenous (inulin) Renal GFR TR + TS regulation 1. layer Not of be Bowman's toxic. of BP, acid-base capsule (podocytes). balance, bone metaboli.RPF Renal artery, ﴿ 97% ﴾ tissue, greater flow to cortex GFR = RPF * FF & inner stripes, pyramid pours urine into minor Glomerulus: = Kf * (60 globular + 0 – 18 tuft 32) of capillaries, respectively afferent Cortical renal nephrons: blood flow 70%-80%, ﴾RBF ﴿* outer (1-hematocrit) two thirds of& When Vasoconstriction x is used 100%toextracted ofmeasure afferentfrom arterioles plasma& decreases excreted; substance GFR. sm 2. but Not (excretion ﴾ Endothelial be stored, of calcium or layer: metabolized fenestrated, & phosphate by kidney. even ions proteins & segmental, interlobar, arcuate arteries, interlobular GFR = glomerular filtration rate of x calyx, every 2-3 calyces unite toPrenal form major calyx efferent = Kf arteriole, *tAHL, (+10 mmHg) inside Bowman's capsule, Bd is cortex, no efferent narrower than afferent. its GFR extraction (decreased ratio PG) E = 1.0 & its clearance= C FF = filtration GFR = fraction, C = U RPF * V = \ plasma flow x x in ﴿secreted in art.s in = 1250 ml\min * 0.5 formation 3. can Not pass. be produced, ﴿ not 1, 25 cells dihydroxycholecalcipherol), or reabsorbed by produ,Kf=ultrafiltration afferent arterioles radial or medullary rays ﴾ which unites with other major calyces to form renal filtered & transferred coefficient to renal (=surface tubules: area*capillproximal Juxtamedullary nephrons: inner third of cortex, RPF Slight =tubular vasoconstriction CxC\ inEx==reabsorption Cx \ 1.0 of =C efferent arterioles Where Clearance of inulin TR = of x x ction renal >100 times of tubules. erythropoietin other capillary hormone, ﴾ BM: high excretion permeability, of & glomerular capillaries, efferent arterioles , periGFR = 625 ml\min * 20% pelvis that leads urine through ureter which ary tubule(PCT permeability), or pars P=hydrostatic convoluta& PST pr., Π=smotic or pars recta) pr. long tAHL, = 625 ml\min efferent wider than afferent. Substance increases GFR (x) is (increased not found PG) yet. Instead, substance U = Urinary concentration of inulin in GFR or .of various 4. ﴿ membranes Not affect metabolic waste RBF products, by itself. drugs, toxic tubular capillaries, (vasa recta,) interlobular veins, TS = tubular secretion of x emerges through hilum of kidney from which ,Severe distal colloids, tubule, B=inside JGA, Bowman's ﴿ TAHL ﴾ , ﴿ tAHL capsule, ﴾ , ﴿ tDHL G=inside ﴾renal , called paraaminohippuric vasoconstriction of acid efferent (PAH) arterioles its extraction GFR = 125 V ml\min = Urine flow substances Other filtered & poisons. materials & ions pass easily through arcuate, interlobar, segmental and renal veins. arteryiscollecting enters & renal vein leaves. Ureters pour into glomerular DCT, capillaries. tubules, These collecting are Starling tubes, cortical forces & ratio decreases 0.9 GFR (E (increased = 0.9) ΠG) P = Plasma concentration of inulin in& PAH membrane slit pores between feet of podocytes. urinary fromduct, which urethra emerges. medullary CD, main minor & major calyx. RPF = Cbladder PAH \ EPAH = CPAH \ 0.9 Exit BASIM ZWAIN LECTURE NOTES Home Renal system Tubular Factors Control Body Regulation control affecting of reabsorption GFR tubular ofof ECF blood ECF tubular reabsorption osmolarity volume osmolarity reabsorption and pressure Countercurrent mechanism + reabsorption When GFR is decreased; tubular flow slows down, 1Sympathetic activity: increases Na Highly B-Angiotensin-II: selective process, Produced passive by lungs or active, from Some 4TR Human Plasma = Kfosmolarity body * levels (netmust reabsorption of amino getosm rid acids of pressure) not&less glucose: than 600 tubular Plasma (P ) calculated from plasma 1-Sympathetic nervous activity:Strong sympathetic Many There DThirst Atrial substances is center glomerulotubular natriuretic in brain are peptide reabsorbed stem balance, increases (ANP): along when Produced the with desire GFR other by for increased tubular reabsorption of NaCl, decrease b.Myogenic mechanism: Increased RBF that causes 2Hormonal activity: 3-Autoregulation: According Descending Osmoreceptor to & equation, ascending cells lie in when limbs anterior no of conc. Henle's hypothalamus urine; loop the and & substances angiotensin-I completely (produced reabsorbed: in liver from aa angiotensino& glucose, Tm About of glucose(TmG) 15% of water reabsorption is about 325 mg\min, occurs in its tDHL ideal reabsorption mosm = Kf of metabolic * (Pif of – amino Pc wastes + Πc acid per Πif) and day. glucose So, it is is unlimited very Starting The Remaining Small major increase from active reabsorption tAHL, in reabsorption Bd vol., all the processes large following of increase electrolytes of electrolytes segments in CO.... are + conc. sodium (P +GFR )…. P = 2.1 * P + activity decreases e.g., in severe hemorrhage Urea recirculation is responsible for about 40% of Na osm Na Na intake ECF volume Blood pressure substances increases; cardiac water intake atria tubular like & in chloride increase response reabsorption ions secretion to any which increases. increase of follow ADH. in sodium But Thirst Bd vol. Chronic increase in BP is balanced by decrease in + NaCl near osmoreceptors, macula densa send increase in GFR; at the same time causes distension A-Aldosterone: adrenal cortex, acts on principal a.Juxtaglomerular minimum vasa sensitive recta to obligatory run any long increase feedback distance urine in Na volume parallel, mechanism: conc., will counter send increase Juxtaglosignals & in 1-Sympathetic Ability of kidney nervous to conc. activity urine requires presence of some gen or are called mostly renin). reabsorbed: Renin is formed bicarbonates in kidneys. & some It renal which threshold is carried is back 325\125 to the =2.6 systemic mg\ml circulation = 260 mg\dL via 1-Osmoreceptors-ADH feedback ,Small necessary when = Kf plasma * to (6 excrete – levels 13 + 32 not of – amino less 15) than mmHg acids 0.5 and respectively liters glucose of highly impermeable occurs (about increase 5%) in TAHL occur to in water (about CO, in distal large in 30%) absence segments. increase which of ADH is in Net mainly BP.. result but Small very due is The major bulk of tubular reabsorption of water & But, in patients with renal diseases, plasma conc.s Normal ECF osmolarity is about 280-300 mosm\L & cerebral ischemia while role of parasympathetic the process of urine concentration when urea is ions, active center acts sodium transport is especially also chloride stimulated processes on collecting salt by which may decreased ducts be follows saturated to ECF decrease water. volume, when + angiotensin II production results in decrease impulses to JG cells to relax, vasodilatation of of afferent arterioles and stretch of smooth muscles cells of distal tubules, increase Na reabsorption & merular resulting close to supraoptic proximity apparatus in excessive nuclei to each (JGA): to loss stimulate other. of specific body Descending posterior fluids distal (diabetes tubular limbs pituitary are 2-Hormones hyperosmotic and medulla autacoids created by countercurrent electrolytes, acts directly some (or indirectly are mostly after reabsorbed stimulation in the of But ascending actual vasa renal recta. threshold But tDHL for glucose is impermeable is about 180 to 2-Thirst center in brain stem increase; concentrated = Kf * tubular (+10 urine mmHg) reabsorption daily: increase, decreased Angiotensin II Baroreceptors little to hyperosmotic increase 1Na+-2Cl¯-1K+ amounts in BP, medulla of large solutes active increase which are cotransport passively favours in urine further reabsorbed process excretion. water in solutes (about 65%) occurs in proximal tubules. So, of urea & glucose are also calculated. and it is mostly dependant on sodium ions conc. + (vagal) innervations is yet unknown. reabsorbed from medullary colleting tubules to the Some tubular sodium decreased substances and lumen BP, water angiotensin overloaded. 50% reabsorption reabsorbed II Maximum & dryness and (50% so, tubular increase of excreted) mouth, load + excretion. Na reabsorption directly or indirectly by decreasafferent arterioles, increase Bd flow to glomerular lining their walls. This stretch results in myogenic K It increases permeability of luminal epithelial insipidus). called gland to countercurrent increase cells Excessive (macula secretion intake multipliers densa: of of ADH hyperosmotic osmoreceptors, because (vasopressin) they fluids to 3-Autoregulation mechanism & urea recirculation & ADH. presence aldosterone) of hormones:water to increase sodium reabsorption ions reabsorption. increases mg\dL, solutes which this difference stay within may thin be segment due to that not not all of 3-Salt appetite center in brain stem amounts Kf is constant NaCl depends near osmoreceptors on surface area, of thickness macula & tAHL. which reabsorption Acute increase works So, tubular against (about in BP fluid 19%) as balanced much reaches from as by collecting the 200 direct following mosm\L increase ducts conc. in in tubular fluid reaches the thin segments within its When P decreases; excretion of large amounts of (142 mEq\L). Normal daily sodium ions intake 2-Hormones&autacoids:Adrenaline, noradrenaline medullary interstitium to be secreted again from + osm like just urine pharynx urea. before excretion & Some saturation esophagus to substances restore is & transport vice normal completely versa. Bd maximum Inhibited vol. excreted (Tm). also like + + + ing aldosterone production from adrenal cortex. capillaries, increase GFR & vice versa contraction of smooth muscles & vasoconstriction 600 mosm\day Na excretion Pressure natriuresis Brain stem membrane to Na & stimulates Na -K pump in sensitive like continuously increase sea water water to changes bring will reabsorption. seriously new in conc. NaCl increase of ADH to NaCl) medulla is P stimulated in contact while & min. by 4-Plasma levels of amino acids and glucose + in C-Antidiuretic presence of antidiuretic hormone (vasopressin): hormone, sodium produced ions renal reabsorbed. tubules So, have tubular the same fluid Tm reaches and that the ascending some of osm densa, permeability, send impulses P is hydrostatic to JG cells pr., to Π relax is osmotic resulting pr. segment gradient. presence Na excretion still of So, ADH hyperosmotic tubular due & to only increase fluid about reaches (900 GFR 1% mosm\L). distal & of decrease filtered tubules water in original osmolarity (300 mosm\L). diluted urine (down to 50 mosm\L) while when P must equals its daily output = 10-20 mEq ,by angiotensin II, aspirin& endothelin decrease GFR. the tubular cells of thin segments to their lumen osm creatinine Maximum E-Parathyroid gastric distension. and plasma some hormones:Produced conc. drugs before and poisons. a substance by parathyroid starts to = 0.5 L\day this is the minimum obligatory urine volume Renin is also produced by JG cells in response to of afferent arterioles & decreased RBF & GFR. basolateral membrane. Adrenal insufficiency with obligatory ascending decreased specific Bd vasa urine smooth vol., recta vol. decreased muscle even are called with cells BP, maximum countercurrent nausea, in wall of vomiting, urine afferent +filtered +acts reabsorption from posterior in pituitary presence gland of aldosterone and it and\or on distal the limbs highly glucose hyperosmotic molecules (1200 before mosm\L). Tm bypass in of colloids, vasodilatation c is peritubular of afferent arterioles, capillaries, increase and if Bd isto hypoosmotic excreted Na reabsorption in urine. (100 with While mosm\L). increase in absence in Na of ADH, leak back about increases; excretion of small amounts of highly 1200 mosm\L Nitric oxide, prostaglandin & bradykinin increase where the cycle is repeated again and again. appear glands Salt appetite & in act urine center especially its in renal the on brain TAHL threshold=Tm\GFR stem (& DCT) increases the + to increase in GFR or RBF, production of angiotensin (Addison's disease) results in excessive Na loss & arterioles, conc. exchangers morphine resulting & juxtaglomerular because nicotine in death they & from vice continuously cells. versa. dehydration. ADH draw inhibited back + angiotensin and collecting II tubules hormones. and ducts to increase water reabsorption. flow interstitial to glomerular fluid capillaries, increase GFR. 20% tubular of filtered lumen (pressure water is excreted. natriuresis) which is Aldosterone Na reabsorption Sympathetic activity conc. urine (up to 1200 mosm\L). GFR increase desire for calcium salt intake. and magnesium ions reabsorption + IK & angiotensin II to decrease GFR & RBF. retention while adrenal hyperactivity (Cushing water by alcohol from intake. medulla to the systemic circulation. reabsorption and urine concentration. always accompanied by pressure diuresis and decrease phosphate +reabsorption. + depletion syndrome) results in Na retention & K Home Exit BASIM ZWAIN LECTURE NOTES Renal system Body regulation Physiology of micturition of acid-base balance Urine enters bladder in spurts synchronous with +] will Buffer The first internal systems: urge urethral to void is sphincter, felt at all volume smooth ofmuscles 150 ml & on Any change in [H affect cellular and body 2-Phosphate buffer system: important buffer in regular peristaltic contractions ofacidic ureteric smooth 1-Bicarbonate the either marked sides, sense plays buffer of no fullness role system: inonmicturition, ismany the at 400 most ml. important in But male thisitis c. Renal regulation: excretion of or alkaline functions due to its effects reactions. intracellular & renal tubular fluids. Its pK is 6.8 + When 4-Ammonium Respiratory HCO regulation: ¯ buffer decreases; system: stimulation metabolic the last acidosis of choice respiratory system + muscles (1-5/minute), of ureters +property 3renal buffer relieved prevents system by retrograde inECF ECF. ejaculation ofoblique when plasticity. [Hinsertion ](reflux isis Micturition increased: semen isso; it urine. Daily secretion of H 4400 mmol. Normal [H ] in is only 0.00000004 mol\L, + 2 When [H+] increases: H + HPO ¯ → H PO ¯ 4 2 4 + ¯ When in center renal PCO bytubules central increases; when chemosensitive bicarbonate respiratory areas and acidosis which phosphate areof into vicinity of bladder walls prevents back flow +](expired) 2 H initiated +HCO urinary after → bladder). relaxation H CO External → of H muscles O + sphincter, CO of pelvic skeletal floor, Bicarbonates system buffers 4320 mmol & other 80 is better to use pH (which is –log [H = 7.4). 3 2 3 2 2 When [OH¯] is increased: When systems bilateral HCO are aggregations saturated. ¯ increases; of Ammonium neurons metabolic beneath is alkalosis formed ventral from urine. Bladder parasym.:S2, S3& S4 with pelvic nn. 3 While downward muscle, when contracts pull [OH-] on voluntarily, detrusor is increased: muscle, delay micturition excitation ofor mmol buffered by phosphates & then ammonium Nobody can survive more than hours when pH 2 OH¯ + H PO ¯ → HPO ¯ + H O +&P 2 4 4 2 When metabolism surface PCO of medulla of decreases; glutamine sensitive respiratory inside to changes renal alkalosis tubular in H cells. Sym. from L1, L2 &L3 via hypogastric nn after + 2 CO2 OH¯ stretch interrupt + receptors HMost its CO starting. → in H its O Delay wall, + HCO micturition reflex ¯ (excreted) contraction. is learning The systems. renal tubular cells utilize secondary raises to 8.0 or falls to 6.8 Regulation of [H ] is by 2 3 2 3 3-Protein buffer systems:the most available intra+ + NH ++& raises When Double [H+] alveolar increases: ventilation H reduces → NH P + + relay intransport ganglion. 3micturition; CO2 4 for The afferent ability power ofinferior &brain efferent ofofdissociation inmesenteric adults. limbs After of constant voiding (pK) reflex run female thiswith active to secrete H like Na -H antiport, one or more the following systems: Chemical cellular systems but also work the th extracellularly. When pH from [OH-] 7.4 to is 7.63 increased: while 1\4 OH¯ alveolar + NH4+ ventilation → NH4OH Somatic sensory & motor from S2, S3 & S4 viaby system pelvic urethra nerves is empties 6.1, to so sacral Henderson-Hasselbalch by gravity cord, while threshold male is urethra adjusted equation: but the intercalated cells of distal tubules utilize acid-base buffer systems in body fluids, respiratory most important is hemoglobin in RBCs. raises Pcontractions & facilitatory reduces pH tovia 6.95 pudendal nn. Sensory also pelvic & hypogastric CO2 pH by several =renal 6.1 + of log [HCO of ¯]\0.03 bulbocavernosus (pons PCO & posterior muscle. hypothprimary active transport called proton pump andactivity regulation of acid-base balance.` + 3 2 H + Hb → HHb alamus) & inhibitory (midbrain) centers. Home Exit BASIM ZWAIN LECTURE NOTES