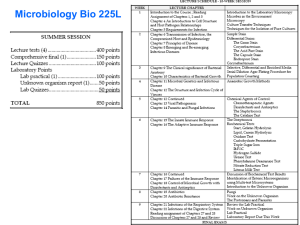
Lecture 5
Infectious process.
Non-specific host defence.
Immunity. Immune system.
Lecture 5
Infectious process.
Non-specific host defence.
Immunity. Immune system.
What Is Infection?
Our environment is full of microorganisms (microscopic
organisms) referred to as microbes (bacteria, fungi,
protozoa and viruses).
Microbes that are capable of causing disease (ie.,
pathogenic) are called pathogens/the infectious or
causative agent.
The interaction between the pathogen microorganism, the
environment and the host is defined as infectious disease
process.
If a pathogen invades the body and the conditions are
favorable for it to multiply and cause injurious effects or
disease, the resulting condition is called an infection.
Infectious process
The process may be thought of as a
circular chain with six links.
The following story illustrates the chain.
I. Chain of Infection
Horton & Parker: Informed Infection Control Practice
I. Chain of Infection
Horton & Parker: Informed Infection Control Practice
Normal Flora
Pathogens
Opportunistic Pathogens
Brady; Paramedic Care Principles & Practice
I. Microorganisms
Types of microbes causing infectious disease
Type
Branch
(Kingdom)
Cellular? Genome Nuclear
membrane?
Example
Metazoan Eucarya
parasites (Animalia)
yes
DNA
yes
Protozoan Eucarya
parasites (Protista)
yes
DNA
yes
Plasmodium
falciparum
Fungi/
yeasts
yes
DNA
yes
Candida
albicans
yes
DNA
no
Bacteria
Eucarya
(Fungi)
Eubacteria
(not Archaea)
Viruses
no
simplex
Prions
no
no genes no
(Mad Cow Disease)
Ascaris
lumbricoides
DNA/RNA no
Streptococcus
pyogenes
Herpes
BSE
Phylogenetic Classification of Bacteria
Oxford Textbook of Medicine
Phylogenetic Classification of Viruses
Oxford Textbook of Medicine
Prions
Mabbott & MacPherson, Nat Rev Microbiol 2006
Two basic types of pathogens
- exogenous pathogen aggressive pathogen, requires acquired immunity for host
defense
- opportunistic (endogenous) pathogen becomes a pathogen when host is compromised
• damage to epithelium
• introduction of bacteria to sites where they are not
normal flora - linked to presence of foreign body,
catheters, biofilms
• disruption of normal flora by antibiotics
• suppression of immune system by drugs
• insufficient host defenses due to infection
II. Chain of Infection
Horton & Parker: Informed Infection Control Practice
Reservoirs
A host that carries a pathogen without injury to
itself and serves as a source of infection for
other host organisms.
Reservoir of infection – ecological niche where the infectious agent
survives and multiplies
ex. person, animal, arthropod, soil, or substance
(asymptomatic infective carriers)
Reservoirs,
examples
Humans
{hepatitis}
Other Vertebrates
{antrax, pesta}
Birds & Bats
{chlamidia, leptospirosis}
soil, or substance
{tetania}
NOT vectors
III. Chain of Infection
Horton & Parker: Informed Infection Control Practice
Portal of exit
Portal of exit - the route by which the disease agent may
While many disease agents have only one portal of exit, others
may leave by various portals.
The portals most commonly associated with human and animal
diseases are:
escape from the human or animal reservoir.
•
•
•
•
Respiratory
Genitourinary
Gastrointestinal
Skin
Superficial lesions
Percutaneous
• Transplacental
Respiratory:
Respiratory:
the route of many disease agents that cause respiratory
illnesses such as
common cold,
influenza, and
tuberculosis.
the route used by many childhood vaccine-preventable
diseases (measles, mumps, rubella, pertussis,
Haemophilus influenzae type b (Hib) and pneumococcal
disease).
the most important portal, but the most difficult to
control.
Genitourinary:
Genitourinary:
This portal of exit is the route of sexually
transmitted diseases, including
syphilis,
gonorrhea,
chlamydia,
HIV.
Schistosomiasis, a parasitic disease and
leptospirosis, a bacterial infection, are both
spread through urine released into the
environment.
Gastrointestinal:
Gastrointestinal:
Examples include:
Hepatitis A
Salmonella, including typhoid
Shigella
Cholera
Giardia
Campylobacter
In general, enteric diseases may be controlled
through good hygiene, proper food preparation
and sanitary sewage disposal.
Skin:
Skin:
Skin may serve as a portal of exit through
superficial lesions or through percutaneous
penetration.
Superficial skin lesions that produce infectious
discharges are found in
smallpox,
varicella (chickenpox),
syphilis, and
impetigo.
Percutaneous exit occurs through
mosquito bites (malaria, West Nile virus) or through
the use of needles (hepatitis B and C, HIV).
Transplacental:
Transplacental:
This portal of exit from mother to fetus is
important in the transmission of:
rubella,
HIV,
syphilis, and
cytomegalovirus (the most common infectious cause
of developmental disabilities).
It is, fortunately, not a factor for most diseases.
Some Pathogens that cross the Placenta
IV. Chain of Infection
Horton & Parker: Informed Infection Control Practice
Mode/means of transmission
A mode of transmission is necessary to
bridge the gap between the portal of exit
from the reservoir and the portal of entry
into the host.
The two basic modes are:
direct
indirect
Direct transmission
occurs more or less immediately. Many diseases are
transmitted by direct contact with
human,
animal or
environmental reservoir.
Ex. sexually transmitted diseases and enteric diseases such
as shigella, giardia and campylobacter.
Ex. contact with soil - mycotic (fungal) diseases.
Droplet spread is also considered direct transmission.
Infectious aerosols produced by coughing or sneezing can
transmit infection directly to susceptible people up to 2 m.
Indirect transmission
May occur through:
1. animate or
2. inanimate mechanisms.
Animate mechanisms involve vectors.
Ex. flies may transmit infectious agents such as shigella in a
purely mechanical way, by walking on feces and then on food.
Ex. mosquitoes, ticks or fleas may serve as reservoirs for the
growth and multiplication of agents in malaria or Lyme disease.
Arthropod Vectors
Pathogen - Vector
Viruses (Arbovirus) - Mosquitoes
Bacteria (Yersinia) - Fleas
Bacteria (Borrelia) - Ticks
Rickettsias (R. prowazeki) - Lice, ticks
Protozoa (Plasmodium) - Mosquitoes
Protozoa (Trypanozoma) -Tsetse flies
Helminths (Onchocerca) - Simulium flies
Inanimate mechanisms:
• involve environmental vehicles, including
objects,
food,
water,
milk, or
biological products.
Ex. Food - salmonella infections.
Water - cholera outbreaks.
Surgical instruments and implanted medical devices staphylococcal infections.
Modes of Disease Transmission
V. Chain of Infection
Horton & Parker: Informed Infection Control Practice
Portal of entry
The portal of entry into the host is usually the
same as the portal of exit from the reservoir.
In some diseases, however, the exit and entry
portals may differ.
Ex.: staphylococcal bacteria may escape from one person’s
respiratory tract to infect another person’s skin lesion.
If that person is a foodhandler, the staphylococcal bacteria
may escape from the infected skin lesion, contaminate food
where it can incubate, and cause “food poisoning” in people
eating the food.
VI. Chain of Infection
Horton & Parker: Informed Infection Control Practice
Susceptible Host
The last essential component in the chain of
infection is the susceptible host.
A person who cannot resist a microorganism
invading the body, multiplying, and resulting in
infection.
Susceptibility is affected by:
Genetic factors
Non-specific defence
Specific acquired immunity
Genetic factors
The role of genetic factors in
susceptibility to infectious diseases is not
yet well understood.
Genes do seem to play a role in the
progression of HIV disease, and
perhaps in individuals’ susceptibility to
meningococcal meningitis are
described.
Host defense factors
Intact skin and mucous membranes help
us resist disease.
So do the gastric acid in our stomachs,
the cilia in our respiratory tracts and the
cough reflex.
Specific acquired immunity
This immunity is specific to a particular
disease agent, and it may be acquired
naturally
or
artificially
Summarize – 6 chains of infection
Infectious agent
Reservoir
Portals of exit
Means of transmission
Portal of entry
Susceptible host
REVIEW - Chain of Infection
Horton & Parker: Informed Infection Control Practice
The Infectious Disease
Spectrum
The impact of disease agents on human host
populations is very different.
If a large number of individuals are equally
exposed to an infectious agent, they do not all
respond in the same manner.
It may be a broad range of responses.
Exposure to Infectious Agents
Infectious
agents
No infection
Death
Host
Clinical
Carrier
Sub-clinical
Immunity
Outcome
Carrier
No immunity
Manifestations of infectious process
(Infection spectrum)
a.
b.
c.
d.
a.
Clearance of pathogen
Subclinical infection
Clinical infection or apparent infection
Carrier state
- Health carrier - after subclinical infection
- Convalescent carrier - after clinical infection
- Incubatory carrier - before onset of diseases
According to carrier time: - acute (transient) carrier
- chronic carrier.
Latent infection
Iceberg Concept of Infection
Clinical features of infectious
disease
Incubation period – the time between exposure to a pathogenic
organism and when first symptoms apparent.
Prodromal period – the time during which a disease process has
begun but is not yet clinically manifest. May appear some prodromal
symptoms.
Period of apparent manifestation - the acute phase when specific
symptoms appear.
Convalescent period - during this time the body systems return to
normal.
Relapse - is the return of a disease after its apparent recovering.
Recrudescence - the recurrence of symptoms after a temporary
abatement.
The distinction between a recrudescence and a relapse is the time
interval. A recrudescence occurring after some days or weeks, a
relapse after some weeks or months.
Dynamics of disease and
infectiousness/contagiosity
Latent period
Infectious period
Contagious period
Incubation period
Infection
Clinical disease
Onset of
symptoms
Non-infectious period
Recovery
Resolution
of symptoms
Time
Common symptoms and
signs
Fever:
Three stages:
effervescence
fastigium
deffervescence
Five kinds of fever: sustained fever,
remittent fever,
intermittent fever,
relapsing fever,
saddle type fever.
And irregular fever
Common symptoms and signs
Rash eruption
Date of eruption
chickenpox
smallpox
typhus
scarlet fever
measles
typhoid fever
Location of eruption
Form of rash
- Exanthema: maculo-papular rash
petechia
vesiculo-pustular rash
urticaria
- Enanthema
Common symptoms and signs
Toxemic symptoms
Mononuclear phagocyte system
reactions
Hepato-splenomegale
Lymphonodus enlarged
Clinical types
acute, subacute, mild, common, severe,
fulminate, typical, atypical, abortive.
Types of Diseases
Diseases are given different names on the
mode of their transmission, geographic area of
distribution, or severity etc.
1.
2.
3.
4.
5.
6.
Communicable Diseases
Noncommunicable Diseases
Endemic Diseases
Epidemic Diseases
Pandemic Diseases
Other type of Diseases
Disease occurrence in populations
Sporadic: occasional cases occurring at irregular
intervals;
Endemic: continuous occurrence at an expected
frequency over a certain period of time and in a certain
geographical location;
Epidemic or outbreak: occurrence in a community or
region of cases of an illness with a frequency clearly in
excess of normal expectancy;
Pandemic: epidemic involves several countries or
continents, affecting a large population.
Factors influencing disease transmission
Agent
Environment
Host
Factors influencing disease
transmission:
Agent
Environment
• Weather
• Infectivity
• Housing
• Pathogenicity
• Geography
• Toxigenicity
• Occupational setting
• Virulence
• Air quality
• Immunogenicity
• Food
Host
• Host defence
• Age, Sex
• Genotype
• Behaviour
• Nutritional status
• Health status
Basic terms frequently used in describing
aspects of pathogen agents:
Infectivity:
Multiplication of an infectious agent within the body.
Multiplication of the bacteria that are part of normal flora
of gastrointestinal tract, skin, etc, is generally not
considered an infection.
On the other hand, multiplication of pathogenic bacteria
(e.g. Salmonella species), even if the person is
asymptomatic, is deemed an infection.
Basic terms frequently used in describing
aspects of pathogen agents:
Pathogenicity:
The ability of an infectious agent to cause disease.
Virulence:
The quantitative ability of an agent to cause disease.
Virulent agents cause disease when introduced into the
host in small numbers.
Virulence involves invasiveness and toxigenicity.
Basic terms frequently used in
describing aspects of pathogenesis:
Toxigenicity:
The ability of a microorganism to produce a
toxin that contributes to the development of
disease.
Invasion:
The process which bacteria, parasites, fungi
and viruses enter the host cells or tissues
and spread in the body.
Bacterial virulence factors
Many
factors
determine
the
virulence of bacteria, or their ability
to cause infection and disease.
Toxins
Enzymes
Antiphagocytic factors
Adherence factors
Toxins
Toxins produced by bacteria are generally
classified into two groups:
Endotoxins
Exotoxins
Endotoxins of gram-negative
bacteria
The endotoxins of gram-negative bacteria are complex
lipopolysaccharides derived from bacterial cell walls
and are often eliberated when the bacteria lyse.
The substances are heat-stable and can be extracted
(e.g. with phenol-water).
The presence of endotoxins in the blood is called
endotoxemia.
It can lead to septic shock, if the immune response is
severely pronounced.
Effects of endotoxins
fever
leukopenia
hypotension
acidosis
activation of C3 and complement cascade
disseminated intravascular coagulation (DIC)
death
Exotoxins
Many gram-positive and gram-negative
bacteria produce exotoxins of considerable
medical importance.
Some of these toxins have had major role in
world history (e.g. toxin of Clostridium
tetani).
Exotoxin
Excreted by a microorganism, including bacteria, fungi, algae, and
protozoa.
Can cause damage to the host by destroying cells or disrupting
normal cellular metabolism.
Exotoxin may be secreted, or may be released during lysis of
the cell.
Most exotoxins can be destroyed by heating.
They may exert their effect locally or produce systemic effects.
Exotoxins are susceptible to antibodies produced by the
immune system, but many exotoxins are so toxic that they may
be fatal to the host before the immune system has a chance to
mount defenses against it.
Well-known exotoxins include the botullinum toxin produced by
Clostridium botulinum.
Ex. Botulotoxin (toxin of Clostridium botulinum)
Clostridium botulinum is found in soil or water and
may grow in foods if the environment is appropriately
anaerobic.
An exceedingly potent toxin (the most potent toxin
known) is produced by Clostridium botulinum strains. It is
heat-labile and is destroyed by sufficient heating. There
are eight disctinct serological types of toxin. Types A, B
and E are most commonly associated wih human disease.
Toxin is absorbed from the gut and carried to motor nerves,
where it blocks the release of acetylcholine at synapses
and neuromuscular junctions. Muscle contraction does not
occur, and paralysis results.
Ex. Tetanospasmin (toxin of Clostridium tetani)
Clostridium tetani is an anaerobic gram-positive rod that is
widespread in the environment.
Clostridium tetani contaminates wounds, and the spores germinate in
the anaerobic environment of the devitalized tissue. The vegetative
forms of Clostridium tetani produce toxin tetanospasmin.
Toxin reaches the central nervous system by retrograde transport
along axons and through the systemic circulation.
The toxin acts by blocking release of an inhibitory mediator in motor
neuron synapses. The result is initially localized then generalized,
muscle spasms. Extremely small amount of toxin can be lethal for
humans.
Ex. Streptococcal erythrogenic toxin
Some
strains
of
hemolytic
lysogenic
streptococci produce a toxin that results in a
punctate maculopapular erythematous rash,
as in scarlet fewer.
Production of erythrogenic toxin is under the
genetic control of temperate bacteriophage. If
the phage is lost, the streptococi cannot
produce toxin.
Ex. Toxic shock syndrom toxin - 1 (TSST-1)
Some Staphylococcus aureus strains growing on
mucous membranes (e.g. on the vagina in association
with menstruation), or in wounds, elaborate TSST-1.
Although the toxin has been associated with toxic shock
syndrome, the mechanism of action in unknown.
The illness is characterized by shock, high fever, and a diffuse
red rash that later desquamates; multiple other organs
systems are involved.
Toxins associated with diarrheal
diseases
Vibrio cholerae toxin
Staphylococcus aureus enterotoxin
Other enterotoxins are also produced by some
strains of:
Yersinia enterocolitica
Vibrio parahaemolyticus
Aeromonas species
Enzymes
Many species of bacteria produce enzymes that are
not intrinsically toxic but play important role in the
infectious process.
Collagenase:
degrades collagen, the major protein of fibrous
connective tissue, and
promotes spread of infection in tissue.
Coagulase:
Staphylococccus aureus produce coagulase, which
works in conjuction with serum factors to coagulate
plasma.
contributes to the formation of fibrin walls around
staphylococcal lesions, which helps them persist in
tissues.
Enzymes
Hyaluronidases:
hydrolyze hyaluronic acid, a constituent of the ground
substance of connective tissue
produced by many bacteria (e.g. staphylococci,
streptococci and anaerobes)
aid in their spread through tissues.
Streptokinase (fibrinolysin):
by many hemolytic streptococci,
activates a proteolytic enzyme of plasma.
able to dissolve coagulated plasma and probably aids in
the spread of streptococci through tissues.
used in treatment of acute myocardial infarction to
dissolve fibrin clots.
Enzymes
Hemolysins and leukocidins:
Many bacteria produce substances that are cytolysins they dissolve red blood cells (hemolysins) or kill tissue
cells or leukocytes (leukocidins).
Streptolysin O, for example, is produced by group A streptococci
and is letal for mice and hemolytic for red blood cells from many
animals.
Antiphagocytic factors
Many bacterial pathogens are rapidly killed by
polymorphonuclear cells or macrophages.
Some pathogens evade phagocytosis by
adsorbing normal host componets to their
surfaces.
For example, Staphylococcus aureus has surface
protein A, which binds to the Fc portion of IgG. Other
pathogens have surface factors that impede
phagocytosis, e.g. Streptococcus pneumoniae and
many other bacteria have polysaccharide capsules.
Adherence factors
Once bacteria enter the body of the host, they
must adhere to cells of a tissue surface. If they do
not adhere, they would be swept away by mucus
and other fluids that bathe the tissue surface.
Adherence (which is only one step in the infectious
process)
is
followed
by
development
of
microcolonies and subsequent complex steps in the
pathogenesis of infection.
Factors influencing disease
transmission
Agent
Environment
• Weather
• Infectivity
• Housing
• Pathogenicity
• Geography
• Toxigenicity
• Occupational setting
• Virulence
• Air quality
• Immunogenicity
• Food
Host
• Immunity
• Age, Sex, Genotype
• Behaviour
• Health status, Nutritional
status
• Host defence
Lecture 5
Infectious process.
Non-specific host defence.
Immunity. Immune system.
The action of immune reaction of
host in infectious process
Non
specific host-defence
Specific
immunity
HOST DEFENSE MECHANISMS
1st LINE OF DEFENSE
2nd LINE OF DEFENSE
intact skin
mucous membranes & their secretions
phagocytic white blood cells
inflammation
-complement
fever
-interferon
nonspecific
3rd LINE OF DEFENSE
B & T lymphocytes
antibodies
specific
1st LINE OF DEFENSE
1.
2.
3.
PHYSICAL BARRIERS
CHEMICAL BARRIERS
GENETIC BARRIERS
PHYSICAL BARRIERS
First line of defense are barriers
that shield interior of body from
external surroundings
Anatomical barriers include
skin and
mucous membranes
Provide physical separation
Membranes bathed in antimicrobial
secretions
PHYSICAL BARRIERS
Physical barriers
Skin is most visible barrier.
Covers majority of surfaces
in contact with environment.
Mucous membranes
barrier that lines digestive
tract, respiratory tract and
genitourinary tract
Mucous protect these
surfaces from infections.
PHYSICAL BARRIERS
Skin
Provides the most difficult barrier to penetrate
Composed of two main layers
Dermis
Contains tightly woven fibrous connective tissues
Makes extremely tough
Epidermis
Composed of many layers of epithelial cells
As cells reach surface, they become increasingly flat
Outermost sheets of cells embedded with keratin
Makes skin water-repellent
Outer layers slough off taking microbes with it
SKIN
Dermis
Inner thicker portion
Outer, thinner portion
Epidermis
Keratin (waterproofing)
SKIN INFECTIONS
Rare in unbroken skin
Sweat washes microbes off
Cuts and burns may get infected
Subcutaneous infections
Staphylococcus spp.
MUCOSAL MEMBRANE
Epithelial layer
Connective tissue
Bronchi
Intestine
MUCOSAL SURFACES (cont.)
1
2
1. Reproductive tract
2. Urinary tract
3. Gastrointestinal tract
4. Respiratory tract
3
4
PHYSICAL BARRIERS
Mucous membranes
Constantly bathed with
mucus
Helps wash surfaces
Some mucous membranes
have mechanisms to propel
microorganisms and
viruses to areas where they
can be eliminated
MUCOSAL SURFACES (cont.)
Mucosal irritation or damage facilitates
infection (smoking)
Substances produced by pathogens
Treponema pallidum
CHEMICAL BARRIERS
Sebaceous secretions
Lysozyme, an enzyme
that hydrolyzes the cell
wall of bacteria, in tears
High lactic acid &
electrolyte
concentration in sweat
CHEMICAL BARRIERS
Skin’s acidic pH
Hydrochloric acid in stomach
Digestive juices and bile of
intestines
Semen contains
antimicrobial chemical
Vagina has acidic pH
CHEMICAL FACTORS
Skin
Sebaceous glands
Unsaturated fatty acids
pH 3-5
SPECIALIZED CHEMICAL BARRIERS
Antimicrobial substances
Both skin and mucous membranes are protected by variety of
antimicrobial substances including
Lysozyme
Peroxidase
Found in saliva, body tissues and phagocytes
Breaks down hydrogen peroxide to produce reactive oxygen
Lactoferrin
Enzymes that degrade peptioglycan
Found in tears, saliva, blood and phagocytes
Sequesters iron from microorganisms
Iron essential for microbial growth
Found in saliva, some phagocytes, blood and tissue fluids
Defensins
Antimicrobial peptides inserted into microbial membrane
Found on mucous membranes and in phagocytes
LYSOZYME
Enzyme that degrades peptidoglycans
Gram + are more susceptible than Gram -
Secreted in
Sweat
Saliva
Tears
Nasal secretions
GASTRIC JUICE
Hydrochloric acid (pH 1.2 to 3)
Helicobacter pylori
Neutralizes acidic pH
Enzymes
Mucus
NORMAL FLORA
Normal flora
Defined as microorganisms found growing on
body surfaces of healthy individuals
Not technically part of immune system
However, provides significant protection
Protects through competitive exclusion
Covers binding sites
Pathogens can’t bind
Competes for nutrients
Nutrients unavailable for pathogens
GENETIC IMMUNITY
Some hosts are genetically immune to
the diseases of other hosts.
Some pathogens have great specificity.
Some genetic differences exist in
susceptibility.
1st LINE OF DEFENSE
2nd LINE OF DEFENSE
intact skin
mucous membranes & their secretions
phagocytic white blood cells
inflammation
-complement
fever
-interferon
nonspecific
3rd LINE OF DEFENSE
B & T lymphocytes
antibodies
specific
2nd LINE OF DEFENSE
A HEALTHY IMMUNE SYSTEM IS
RESPONSIBLE FOR:
1.
Recognition of
foreign material
1.
Surveillance of the
body
1.
Destruction of
foreign entities
SYSTEMS INVOLVED IN IMMUNE
DEFENSE
The reticuloendothelial system
The blood
The lymphatic system
The extracellular fluids (ECF) - spaces
surrounding tissue cells
SYSTEMS INVOLVED IN IMMUNE
DEFENSE
RETICULOENDOTHELIAL SYSTEM
This system is formed of
reticular fiber which form a
support network for each
cell.
This network connects one
cell to another within a
tissue or organ.
Provides phagocytic white
blood cell (WBC) the ability
to move within and between
tissues
CELLS OF THE IMMUNE SYSTEM
Always found in normal blood
Numbers increase during infection
Some cells play dual roles in both innate
and adaptive immunity
Blood cell formation called hematopoiesis
Blood cells including immune cells originate from
hematopoietic stem cells in bone marrow
Blood cells stimulated to differentiate by colonystimulating factor
CELLS OF THE IMMUNE SYSTEM
General categories of blood cells
Red blood cells (RBC)
Platelets
erythrocytes
carry oxygen in blood
fragments of megakaryocytes
important component in blood clotting
White blood cells (WBC)
leukocytes
important in host defenses
divided into four categories
Granulocytes
Dendritic cells
- Mononuclear phagocytes
- Lymphocytes
BLOOD CELLS
CELLS OF THE IMMUNE SYSTEM
Granulocytes
Contain cytoplasmic granules
Divided into three types
Neutrophils
Basophils
Eosinophils
CELLS OF THE IMMUNE SYSTEM
Neutrophils
Basophils
Most abundant and important in
innate response
Sometimes called
polymorphonuclear neutrophilic
leukocytes (PMNs)
Involved in allergic reaction
Eosinophils
Important in expelling parasitic
worms
Active in allergic reactions
CELLS OF THE IMMUNE SYSTEM
Mononulcear phagocytes
Constitute collection of
phagocytic cells called
mononuclear phagocyte
system
Include monocytes
Circulate in blood
Macrophages
differentiate from
monocytes
Present in most tissues
Abundant in liver,
spleen, lymph nodes,
lungs and peritoneal
cavity
CELLS OF THE IMMUNE SYSTEM
Dendritic cells
Branched cells involved
in adaptive immunity
Function as scout in
tissues
Engulf material in
tissue and bring it to
cells of adaptive
immunity
CELLS OF THE IMMUNE SYSTEM
Lymphocytes
Involved in adaptive
immunity
Two major groups
B lymphocytes
T lymphocytes
B cells
T cells
Another type
Natural killer
Lacks specificity of B
and T cells
LYMPHOCYTES
LEUKOCYTES
Neutrophils- 55-90% - lobed nuclei with
lavender granules; phagocytes
Eosinophils – 1-3% - orange granules & bilobed
nucleus; destroy eucaryotic pathogens
Basophils, mast cells – 0.5% constricted nuclei,
dark blue granules; release potent chemical
mediators
Lymphocytes – 20-35% - large nucleus B & T
cells involved in the specific immune response
Monocytes, macrophages – 3-7%- large
nucleus; phagocytic
CHARACTERISTICS OF
LEUKOCYTES
Diapedesis – migration of cells out of
blood vessels into the tissues
Chemotaxis – migration in response to
specific chemicals which have passed
through the 1st line of defense
Diapedesis
Chemotaxis
CHARACTERISTICS OF
LEUKOCYTES
Group 1 - Toll-like
receptors and NOD
proteins
Found on variety of
cells
Recognize families of
compounds
Enable cells to sense
invasion
Send signal to body
to respond
LYMPHATIC SYSTEM
1.
Provides an auxiliary route for return of
extracellular fluid to the circulatory
system
1.
Acts as a drain-off system for the
inflammatory response
1.
Renders surveillance, recognition, and
protection against foreign material
LYMPHATIC FLUID
Lymph is a plasmalike liquid carried by
lymphatic circulation
Formed when blood components move out of
blood vessels into extracellular spaces
Made up of water, dissolved salts, 2-5%
proteins
Transports white blood cells, fats, cellular
debris & infectious agents
LYMPH NODES
Small, encapsulated, bean-shaped
organs stationed along lymphatic
channels & large blood vessels of the
thoracic and abdominal cavities
Contains both T and B lymphocytes
RESULTS OF A MICROBE PASSING
THE 2ND LINE OF DEFENSE
CELL COMMUNICATION
In order for immune system to respond to
trauma or invasion, cells must communicate
with environment and with each other
Cell surface receptors are the “eyes” and
“ears” of the cell
Cytokines are the “voice”
Adhesion molecules act as the “hands”
CELL COMMUNICATION
Surface receptors
Membrane proteins to which signal molecules
bind
Receptors specific to molecule to which it bonds
Binding molecules called ligands
When ligand binds, receptor becomes modified
and sends signal to cell
Cell responds by initiating some action like
chemotaxis
CELL COMMUNICATION
Cytokines are proteins made by certain cells as a
mechanism to communicate with other cells.
Cytokines bind to surface receptors; and regulate cell
function
Binding of a cytokine to its receptor induces a change in the
cell such as growth, differentiation, movement, or cell
death.
They can act locally, regionally, or systemically
CYTOKINES
Numerous cytokine classes
Chemokines – important in chemotaxis
Colony stimulating factors – Important in
multiplication and differentiation of leukocytes
Also associated with inflammatory response
Interleukins – produced by leukocytes
During immune response, directs immature leukocytes to
correct maturation pathway
Interferons – important in control of viral
infections
Enhance ability of cells to migrate to appropriate site in body
Important in innate and adaptive immunity
Tumor necrosis factor – kill tumor cells
Instrumental in initiation of inflammation
CELL COMMUNICATION
Adhesion molecules
Allow cells to adhere to each other
Responsible for the recruitment of
phagocytes to area of injury
Causes phagocytes to slow and leak out of vessels
to area of injury
SENSOR SYSTEMS
Systems within blood detect signs of
tissue damage or microbial invasion
Responds to patterns associated with
danger by
Directly destroying invading microbe
Recruiting other host defenses
SENSOR SYSTEMS
Toll-like receptors (TLR) and
NOD proteins
Pattern recognition receptors
TLR allow cells to “see” molecules
signifying presence of microbes
outside the cell
TLR found in variety of cell types
Recognize distinct “danger”
compounds
Signal is transmitted
Results in change of gene
expression of cell
NOD proteins are intracellular
receptors that recognize bacterial
cell wall components within
cytoplasm
SENSOR SYSTEMS
Complement system
Series of proteins circulating in blood and fluids
Augment activities of adaptive immune response
Stimulation of inactive proteins initiates cascade of reactions
Circulate in inactive form
Results in rapid activation of components
Complement system composed of nine proteins
C1 – C9
Numbered as discovered, not order of activation
Certain proteins split into “a” and “b” fragments after activation
C3 can spontaneously split to C3a and C3b
Insures enough C3b for activation of alternative pathway
Complement activation
Three pathways of activation of the
complement system
Classical pathway
Alternative pathway
Lectin pathway
SENSOR SYSTEMS
Classical pathway
Activation requires
antibodies
Antibodies interact
complement C1
Activates protein
Leads to
activation of all
complex
proteins
SENSOR SYSTEMS
Alternative pathway
Quickly and easily initiated
Relies on binding of complement
protein C3b to cell surface
Initiates activation of other
complement proteins
Allows formation of complement
complex
C3b always circulating in blood
so nearly any cell automatically
triggers the pathway unless the
body’s own cells stop the
process
SENSOR SYSTEMS
Lectin pathway
Activation requires
mannose/mannan-binding
lectins (MBL) on host cells
MBLs are pattern recognition
molecules
Detect mannane
Polymer of mannose
Found in microbial cells
MBL attaches to surface of the
microbe if mannan is present
Activates complement
proteins
SENSOR SYSTEMS
Activation of complement leads to major protective outcomes
Inflammation
Opsonization
Lysis of foreign cells
SENSOR SYSTEMS
Inflammation
Complement components C3a and C5a
induce changes in endothelial cells
Effects vascular permeability associated with
inflammation
Opsonization
C3b binds foreign material
Allows phagocytes to easily “grab” particles
SENSOR SYSTEMS
Lysis of foreign cells
Complexes of C5b, C6, C7,
C8 and multiple C9
spontaneously assemble
Forms donut-shaped
structure called membrane
attack complex (MAC)
Creates pores in membrane
Most effective on Gram +
Little effect on Gram + cells
ACTIVITIES OF PHAGOCYTES
1.
To survey tissue compartments &
discover microbes, particulate matter &
dead or injured cells
1.
To infest and eliminate these materials
1.
To extract immunogenic information
from foreign matter
PHASES OF PHAGOCYTOSIS
PHAGOCYTOSIS
Process of phagocytosis
Chemotaxis
Cells recruited to
infection
Recognition/attachment
Use receptors to bind
invading microbes
Engulfment
Phagocyte engulfs
invader forming
phagosome
Phagosome lysosome
fusion
Phagosome binds
lysosome, forming
phagolysosome
Destruction and digestion
Organism killed due to lack
of oxygen and decreased
pH
Exocytosis
Phagocyte expels material
to external environment
INFLAMMATION
STAGES OF INFLAMMATION
1.Blood vessels dilate in response to chemical mediators
and cytokines.
1.Edema swells tissues, helping prevent spread of
infection
3. WBC’s, microbes, debris and fluid collect to form pus
4. Pyrogens may induce fever
5. Macrophages and neutrophils engage phagocytosis
INFLAMMATION
Inflammation occurs in
response to tissue damage
Four cardinal signs
Heat
Pain
Redness
Swelling
Loss of function
Fifth sign that can also be
present
INFLAMMATION
Factors that initiate inflammatory
response
Microbial products trigger toll-like receptors
of macrophages
Microbial cell surface can trigger complement
Causes release of pro-inflammatory cytokines
Leads to the production of C3a and C5a
Tissue damage results in enzymatic cascade
Cascades initiate inflammation
INFLAMMATION
The inflammatory process
Initiation leads to a cascade of
events
Results in dilation of blood
vessels, leakage of fluid from
vessels and migration of
leukocytes and phagocytes
Leakage of phagocytes from
blood vessels called diapedesis
Certain pro-inflammatory
mediators cause the diameter
of blood vessels to increase
Results in increased blood
flow
Increased blood flow
responsible for cardinal signs
of inflammation
INFLAMMATION
Outcomes of inflammation
Intent is to limit damage and restore function
Inflammation itself can cause considerable damage
Release of toxic products and enzymes from phagocytic
cells is responsible for tissue damage
If inflammation is limited to area of injury,
damage is usually nominal
If inflammation results in delicate systems,
consequences are more severe
Inflammation around brain and spinal cord can lead
to meningitis
FEVER
One of the strongest indicators of infection
Important host defense mechanism
Temperature regulation center of body responds
to fever-inducing substances called pyrogens
Especially of bacterial infection
Fever-inducing cytokines termed endogenous pyrogens
Microbial products termed exogenous pyrogens
Resulting fever inhibits growth of pathogens by
Elevating temperature above maximum growth temperature
Activating and speeding up other body defenses
Summary of Innate Immunity
External and mechanical barriers
Receptors for pathogen
Soluble antimicrobial proteins
Pattern of cytokines produced influences
adaptive response
Natural immunity
“active natural immunity” - may be acquired by
experiencing an infection. Many diseases confer
immunity after a single infection, but many others do
not.
For ex. a single bout of measles or chickenpox, confers
lifelong immunity to that disease. Influenza and salmonella
are examples of infections that do not confer immunity and
therefore may recur.
“passive natural immunity” - the transfer of
antibodies from the mother to the newborn child, via the
placenta and/or breast milk. It is diminishes after
varying lengths of time. It is very important in giving
infants a good head start in life.
Artificial immunity
may be acquired through the use of vaccines, toxoids
and immune globulins.
Active immunity: Receiving a vaccine or toxoid
stimulates “active” immunity, since the recipient
responds by producing his/her own antibodies.
Passive immunity: Receiving an antitoxin or immune
globulin confers “passive” immunity, essentially by
borrowing the antibodies of other people.
Passive immunity lasts for only a short time, while active
immunity usually lasts much longer, even for a lifetime.