Genomics in Cancer Diagnosis – Quo Vadem?
advertisement
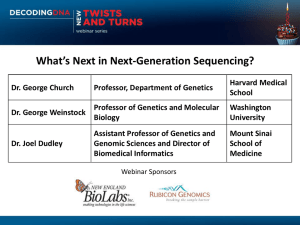
The changing face of cancer diagnosis George Vassiliou November 2011 Overview • • • • Today’s cancer diagnostic lab The era of cancer genomics Novel diagnostic applications Introducing genomics to cancer diagnosis Overview • • • • Today’s cancer diagnostic lab The era of cancer genomics Novel diagnostic applications Introducing genomics to cancer diagnosis The light microscope remains the central cancer diagnostic tool for 400 years Zacharias and Hans Jansen (ca 1595) Modern microscope (ca 1995) Today’s cancer diagnostic lab Cellular Phenotyping Microscopy (histology/cytology) Immunohistochemistry Flow Cytometry Genetic tests Cytogenetics Molecular Genetics Genotyping for specific mutations (PCR/RT-PCR) Minimal Residual Disease monitoring (CGH and SNP/LOH genotyping) (Gene Expression Profiling) Haemato-oncology lab Sample Microscopy Immunophenotyping Cytology Histology Integrated report Immunohistochemistry Diagnostic panels Cytogenetics Karyotyping FISH Molecular Genetics Mutational screening RT-PCR qPCR (MRD) MICROSCOPY: >80% undifferentiated blasts Morphology of acute lymphoblastic leukaemia Eosinophils, basophils and small megakaryocytes suggest blast phase of chronic myeloid leukaemia IMMUNOPHENOTYPE: Blast cells are CD10, CD19, CD79a, CD34, HLA-DR, TdT positive. Weak CD13. They do not express CD33 or myeloperoxidase. DNA index is 1.0 Phenotype of B lymphoblastic leukaemia or B lymphoblastic transformation of CML CYTOGENETICS: Karyotype: FISH: MOLECULAR GENETICS: BCR-ABL fusion transcript type: p210 e13a2 by RT-PCR OVERALL CONCLUSION: B lymphoblastic blast crisis of chronic myeloid leukaemia 46,XY,t(9;22)(q34;q11) in 10 of 10 metaphases BCR/ABL 92% positive Diagnostic CGH/SNP genotyping Diagnostic gene expression profiling n=241 MammaPrint – 70 gene signature (NKI) Lymph node positive breast cancer CR-UK stratified medicines initiative Tumour type Gene Mutation Drug Colorectal KRAS Codons 12, 13, 61, 146 Cetuximab/Panitumumab BRAF V600E/D/K/R/M Sorafenib/Cetuximab TP53 Exons 2-‐11 PI3KCA Exons 9 and 20 PI3Kinase inhibitors UGT1A1 UGT1A1*28 Irinotecan toxicity PI3KCA Exons 9 and 20 Breast Prostate Lung Ovary Melanoma TP53 Exons 2-‐11 PTEN LOH/mutation hotspots mTOR inhibitors CYP2D6 5 SNPs Response to tamoxifen PTEN LOH/mutation hotspots mTOR inhibitors TMPRSS-‐ERG Junction fragment PCR TLR4 2 SNPs EGFR Exons 18-21 Erlotinib/gefitinib EML4-‐ALK Fusion product PF02341066 ALK/c-Met inhibitor XRCC2 5 SNPs Response to platinum agents ERCC1 mRNA expression RRMI mRNA expression PTEN LOH/mutation hotspots PI3KCA Exons 9 & 20 mTOR inhibitors BRAF V600E/D/K/R/M Sorafenib/Braf inhibitors BRAF V600E/D/K/R/M Sorafenib/Braf inhibitors CKIT Exons 11,13,17 Overview • • • • Today’s cancer diagnostic lab The era of cancer genomics Novel diagnostic applications Introducing genomics to cancer diagnosis Advances in DNA sequencing technologies ABI capillary Technologies 454 pyroseq Solexa/ Illumina ABI SOLID ABI Roche/454 Titanium SOLID 3.0 Ion Torrent Illumina HiSeq 1016 1014 12 Output 10 kbp / run 1010 108 Capillary (Sanger) Sequencing Next Generation Sequencing (NGS) 106 104 102 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 Rapid reduction in sequencing costs Sanger Institute Total yield by week (Gigabases) 2008 2009 2010 2011 How Fast is That? 6000 Gb per week (6 Tb) = 10,000,000 bases per second ½ hour per 6Gb (= 1x Human Genome) Genome Sequencing Sanger (capillary) sequencing Next generation sequencing 2000 ~10 years ~$ 3.5 billion 2005 ~3 years ~$ 20million 2010 2008 ~4 months ~1month ~$ 1.5million $9,500 (Illumina) Mouse AML CLL Myeloma Hepatocellular Lung (NSS) Melanoma Small-cell lung Breast AML Cancer Genomics 2015 ? ~1day ?? $100 Analysing cancer genomes From Ding et al, Hum Mol Gen, 2010 Genomic Circos Plot Genomic coordinates Deletions/Insertions Substitution density (het) Substitution density (homo) Coding Substitutions Silent Missense Nonsense Splice site Copy number Regions of LOH Structural rearrangements Intrachromosomal Interchromosomal Circos Plot from Pleasance et al, Nature 2010 This decade • 1000s of individual cancer genomes • 100s of recurrent mutations • Aetiological links • Clinico-pathological correlates • Delineation of effects of many mutations • Development of new therapies > Increasing use of genomics in cancer diagnosis, prognosis & therapy Overview • • • • Today’s cancer diagnostic lab The era of cancer genomics Novel diagnostic applications Introducing genomics to cancer diagnosis The clinical process in oncology Pre-clinical phase Presentation Relapse Diagnosis Follow-up Treatment Assessment of response New diagnostic applications • • • • Whole genome sequencing (~6Gb) Exome sequencing (~60Mb) Selected gene/exon DNA sequencing Residual disease monitoring (plasma DNA) Whole genome sequencing A B C D Diagnostic whole genome sequencing Constitutional genome Cancer genome Compare Inherited mutations & polymorphisms Somatic mutations Subclonal heterogeneity Other diagnostic data Clinical Report Substitutions Indels Copy number changes Translocations Exome sequencing: target enrichment Chr1 NRAS “Baits” or PCR amplicons regions covered Diagnostic whole exome sequencing Constitutional exome Cancer exome Compare Inherited mutations & polymorphisms Somatic mutations Subclonal heterogeneity Other diagnostic data Clinical Report Substitutions Indels Copy number changes Translocations Selective sequencing example: an AML toolkit • ~20 genes known to be recurrently mutated • Prognostic/treatment implications known for some • Target enrichment by “pull down” Can detect: Sequence changes Copy number (UPD/LOH) ASXL1 NF1 BRAF CBL NPM1 IKZF1 CEBPA NRAS HPRT1 CSF1R RUNX1 PAX5 DNMT3A TET2 PIK3CA FLT3 WT1 UGT1A1 IDH1 EZH2 CYP2D6 IDH2 KIT TLR4 JAK2 KDM6A KRAS TP53 MLL PTPN11 EGFR XRCC2 PTEN Selective sequencing example: an AML toolkit AML1 Type A (Transcription Factor) Type B (DNA modification) Type C (Signal transduction) PROGNOSIS NPM1 DNMT3A R882C FLT3-TKD Intermediate TET2 KRAS K117N Intermediate NRAS G12D Intermediate FLT3-TKD Favourable KRAS G12D Poor AML2 AML3 CEBPA AML4 NPM1 AML5 ASXL1 AML6 IDH1 R132H IDH2 R172K Poor Plasma DNA Normal tissues Cancer DNA with tumour-specific mutation Slide courtesy of Dr Peter Campbell Tumour-specific rearrangements Chr10 1st round PCR Nested real-time PCR Individual Breast Cancer Genome Chr20 Relapsing breast cancer Non-rearranged genomic region Tumour-specific rearrangement Undiluted patient plasma 1:10 1:100 1:1000 1:10,000 1:100,000 1 0.5 Normal Water 1 Intensity Intensity 0.5 0.1 0.1 0.05 0.05 0.01 0.01 0 5 10 15 20 25 30 Cycles of real-time PCR Slide courtesy of Dr Peter Campbell 35 40 0 5 10 15 20 25 30 Cycles of real-time PCR 35 40 Serial measurements CT scan: Localised deposits around T9-10 CT scan: Widespread soft-tissue metastases Estimated tumour DNA / mL serum (pg) Chemotherapy: 150 First-line chemotherapy Second-line Paclitaxel 125 100 75 Rearrangement 1 Rearrangement 2 50 25 Detectable at limit of sensitivity Undetectable 5 6 7 8 Slide courtesy of Dr Peter Campbell 9 10 11 12 13 Months after diagnosis 14 15 16 17 Other applications of NGS • • • • Multiple biomarker MRD Methylomics Transcriptomics (RNAseq) Cancer screening / Biomarker assays Overview • • • • Today’s cancer diagnostic lab The era of cancer genomics Novel diagnostic applications Introducing genomics to cancer diagnosis Hurdles to the introduction of diagnostic cancer genome sequencing • • • • Sample choice/compatibility Cost Sample to sequence delay Mutation calling FFPE, other $10,000/genome 8-10 days Specificity / Sensitivity Technology • Clinical relevance/utility • Personal genomes/Ethics Evolving Being tested Clinic • • • • Choice/Cost Bioinformaticians Petabytes (1015) Pathologists, Clinicians Laboratory Sequencing equipment New personnel Computer storage Education/training Data storage & analysis Genome Campus Research Support Facility Data Centre Sulston Building Morgan Building European Bioinformatics Institute Training of pathologists • • • • • • Core training in genomics New sub-specialty e.g. Molecular Pathology? Impact on other aspects of training How will the training be delivered? Training/role of laboratory scientists Keeping control of the agenda Diagnostic reporting of genomic data • Communicating the cancer genome to the clinician – – – – – – – – – Diagnosis Recurrently mutated genes Non-recurrent/private mutations / pathways Prognostic relevance Therapeutic relevance Pharmacogenomics Constitutional genome Mutational signatures Summary / Imagery Implications for cancer classification Cellular origin Morphology Differentiation/grading Mutations: Unified Classification? Diagnosis Prognosis Treatment Acute Myeloid Leukaemia – a paradigm of evolving classification Morphology Single entity Various 1950s Morphology & cytochemistry M0-M7 FAB 1976 Morphology, AML with recurrent cytogenetic translocations WHO 2002 Immunophenotyping & AML with multilineage dysplasia Cytogenetics AML, therapy related WHO 2008 AML not otherwise categorized Morphology, AML with recurrent genetic abberations Immunophenotyping , Provisional entity: AML with mutated NPM1 Cytogenetics & Provisional entity: AML with mutated CEBPA Genetics Otherwise as 2002 Will there be a paradigm shift ? ? Summary • The advent of cancer genomics is changing cancer medicine • Changes will transform cancer diagnosis and the role of pathologists • Pathologists need to understand what is coming in order to lead and formulate the future for cancer diagnosis