Developing TCR gene therapy — Gavin Bendle
advertisement

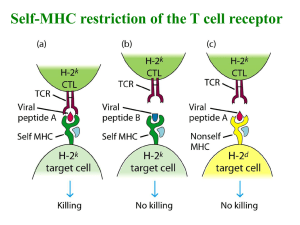
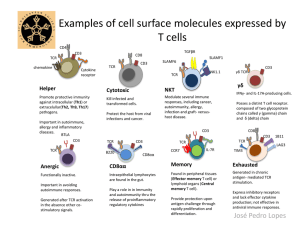
Developing TCR gene therapy for multiple myeloma Gavin Bendle LLR Bennett Senior Fellow School of Cancer Sciences University of Birmingham Overview •Introduction to TCR gene therapy of cancer •Assessing the value of TCR gene therapy in a autochthonous mouse cancer model •Pre-clinical development of TCR gene therapy of MM Multiple myeloma •Plasma cell malignancy that is the second most common haematological malignancy worldwide •Novel agents (e.g. lenalidomide, bortezomib) have contributed to increase in average survival times from 4 to 8 years in the last decade • Despite these advances MM remains largely incurable Need for new therapeutic approaches that not only increase survival times but are also ultimately curative Adoptive T cell therapy • T cell immunity to tumours can be induced by adoptive T cell therapy: • Transfer of T cells • • • T cell replete allogeneic-HSCT & DLI for haematological malignancies Mortality/morbidity due to GVHD limits use Transfer of genes encoding the TCR • • • Ag-specificity of a T cell determined by TCR Endow patient T cells with tumour-reactivity of a defined Agspecificity Destroy tumours without damaging normal tissues TCR gene therapy Cancer patient Removal of peripheral blood lymphocytes Infusion of autologous TCR gene modified T cells Ex vivo transduction process • TCR gene transfer is conceptually attractive: – Generate large numbers of defined antigen-specific patient T cells – Generate tumor-reactive specificities not present in pre-existing T cell repertoire Clinical trials shown feasibility and potential of TCR gene therapy CT scan of liver metastasis in patient treated with TCR-modified T cells Clinical testing of TCR gene therapy for MM has commenced Safety risks associated with TCR gene therapy • Most targets of TCR gene therapy are tumor-associated self-antigens • Toxicity may occur if target antigen is also expressed by some normal tissues • If vital normal tissues express target antigen toxicity can be severe or even fatal Expression profile of target antigen in normal tissues: the critical parameter determining the safety of TCR gene therapy Additional genetic modification of T cells as a strategy to enhance TCR gene therapy efficacy Can additional genetic modification of TCR transduced T cells be used to obtain durable clinical responses with TCR gene therapy? • TCR gene transfer endows patient T cells with desired antigenspecificity • Can additional genetic modification endow these cells with optimal functional properties? Used a mouse model of prostate carcinoma to assess if additional genetic modification of T cells enhances TCR gene therapy efficacy TRAMP mice: prostate tumour model TRansgenic Adenocarcinoma of the Mouse Prostate (Greenberg et al, PNAS 1995) SV40 large T antigen under control of a rat probasin promoter 3 8-12 16 24 Does TGF- signalling blockade in TCR transduced T cells promote tumour regression in TRAMP mice? • Block by co-transducing TCR Td T cells with dnTGFRII • Rationale for blockade of TGF- signalling in TCR transduced T cells: • TGF- signalling inhibits CTL proliferation & effector functions • Elevated TGF-expression in human malignancies including prostate cancer • Elevated levels of TGF- in prostate of TRAMP mice with advanced prostate cancer Does blockade of TGF- signalling in TCR transduced T cells lead to tumour regression in TRAMP mice? Histopathology Week 3 24 8-12 Group I: 16 24 Pre-conditioning (5Gy TBI) + non Td T cells Group II: Pre-conditioning (5Gy TBI) + SV40 TCR Td T cells Group III: Pre-conditioning (5Gy TBI) + dnTGFRII Td T cells Group IV: Pre-conditioning (5Gy TBI) + SV40 TCR & dnTGFRII co-Td T cells 28 Regression of advanced prostate cancer in TRAMP mice after TCR gene therapy and blockade of TGF- signalling Tumour regression in TRAMP mice after TCR gene therapy & TGF- blockade Non-Td SV40 TCR Td SV40 TCR & dnTGFRII co-Td SV40 Large T Ag Immunostaining Ki67 Immunostaining TGF-1 Immunostaining Is the tumour regression observed at 28 wks of age sustained? Sustained regression of advanced prostate cancer in TRAMP mice after TCR gene therapy and blockade of TGF- signalling Does the observed tumor regression lead to enhanced survival? Enhanced survival of TRAMP mice after TCR gene therapy & TGF- blockade Summary • Blockade of TGF- signalling in TCR transduced T cells promotes tumour regression in TRAMP mice with advanced prostate cancer • Demonstrates potential of additional genetic modification of TCR transduced T cells to enhance TCR gene therapy efficacy • Elevated expression of TGF- in many human malignancies including MM suggest that this approach warrants clinical testing Pre-clinical development of TCR gene therapy for MM TCR a- & -chains are generated by genetic rearrangement TCR α-chain TCR β-chain • Sequence information in TCR a- & -chain genes that defines TCR specificity: – – – • V element used J element used Nucleotide sequence at the junction between V-J elements Cloning of TCR genes is a bottleneck in production of new TCRs – Developed high throughput strategy to isolate TCR gene sequences for TCR gene therapy TCR gene capture technology Identify potentially clinically relevant T cell specificities in biological material using multiplexing technology FACS sort single T cells of desired specificity, expand in vitro for 14 days and extract gDNA Reconstruction of TCR a- & -chain genes Align sequence pairs to reference genome to identify rearrangements at TCR a & loci Shear gDNA & enrich for gDNA fragments encoding TCR a & loci Paired-end deep sequencing Linnemann et al. Nature Med in press A library of cancer-testis antigen-specific TCRs assembled using TCR gene capture Target antigen Restriction Peptide # TCRs Material MAGE-C2 A2 ALKDVEERV 2 PBMC MAGE-C2 A2 LLFGLALIEV 1 TIL MAGE-C2 A2 KVLEFLAKL 3 PBMC MAGE-A10 A2 GLYDGMEHL 2 TIL SSX-2 A2 MLAVISCAV 3 PBMC MAGE A2 A2 YLQLVFGIEV 3 PBMC NY-ESO-1 A2 SLLMWITQA 1 PBMC LAGE-1 A2 MLMAQEALAFL 1 TIL MAGE-A1 B7 RVRFFFPSL 1 TIL HERV-Kmel A2 MLAVISCAV 2 TIL TAG A3 RLSNRLLLR 2 TIL Rapidly assembled a panel of tumor-reactive TCRs with the potential to be used for TCR gene therapy of a variety of malignancies Cancer-testis antigens •Cancer-testis (C/T) antigens: • Expressed in human germ line & variety of human malignancies • Attractive targets for TCR gene therapy of MM: • Expression in MM cells in a high frequency of patients • Examples: • MAGE C1: ~ 70% • MAGE C2: ~ 50% • Absent from normal tissues accessible to immune system Validation and characterisation of C/T Ag-specific TCRs C/T Ag-specific TCRs isolated to date Target antigen Restriction Peptide # TCRs Material MAGE-C2 A2 ALKDVEERV 2 PBMC MAGE-C2 A2 LLFGLALIEV 1 TIL MAGE-C2 A2 KVLEFLAKL 3 PBMC MAGE-A10 A2 GLYDGMEHL 2 TIL SSX-2 A2 MLAVISCAV 3 PBMC MAGE A2 A2 YLQLVFGIEV 3 PBMC NY-ESO-1 A2 SLLMWITQA 1 PBMC LAGE-1 A2 MLMAQEALAFL 1 TIL MAGE-A1 B7 RVRFFFPSL 1 TIL TAG A3 RLSNRLLLR 2 TIL •Assess which C/T Ag-specific TCRs are best suited to clinical translation of TCR gene therapy for MM: – C/T Ag expression frequency in MM patient population – Efficacy & safety of T cells transduced with different C/T Ag-specific TCRs Blockade of TGF- signalling in C/T Ag-specific TCR transduced T cells •Additional genetic modification of TCR transduced T cells to tailor their activity can enhance TCR gene therapy efficacy •TGF- in MM dysregulation microenvironment leads to myeloma-induced T cell •Selectively block TGF- signalling in C/T Ag-specific TCR transduced T cells – Generate and validate a retroviral construct encoding the relevant C/T Ag-specific TCR and a dominant-negative TGF- receptor Primary benefit: novel clinical trials of TCR gene therapy in MM patients in B’ham Summary •TCR gene therapy holds promise as a treatment for cancer •Additional genetic modification of TCR transduced T cells to tailor their activity and enhance therapeutic efficacy •TCR gene capture utilized to assemble a library of C/T Ag-specific TCRs that can be used for TCR gene therapy of various cancers •Assessing which TCRs are best suited to clinical translation of TCR gene therapy for multiple myeloma •Pre-clinical development will be followed by clinical testing in B’ham Acknowledgements •NKI, Amsterdam – – – – – – – – – – – Carsten Linnemann Laura Bies Kaspar Bresser Bianca Heemskerk Pia Kvistborg Roel Kluin Ron Kerkhoven Marja Nieuwland Ji-Ying Song John Haanen Ton Schumacher •Cancer Sciences, B’ham – Guy Pratt – Paul Moss •Shemyakin & Ovchinnikov Institute, Moscow – Dmitriy Chudakov – Dmitriy Bolotin •MDC, Berlin – Xioajing Chen – Thomas Blankenstein