Lynch syndrome
Developed by Dr. June Carroll, Ms. Shawna Morrison, Dr. Sean Blaine and Dr. Judith
Allanson
Last updated April 2014
Disclaimer
• This presentation is for educational purposes only and should
not be used as a substitute for clinical judgement. GEC-KO
aims to aid the practicing clinician by providing informed
opinions regarding genetic services that have been developed
in a rigorous and evidence-based manner. Physicians must use
their own clinical judgement in addition to published articles
and the information presented herein. GEC-KO assumes no
responsibility or liability resulting from the use of information
contained herein.
Objectives
• Following this session the learner will be able to:
– Refer to their local genetics centre and/or order genetic
testing appropriately for Lynch syndrome (LS)
– Discuss and address patient concerns regarding family
history of LS
– Find high quality genomics educational resources
appropriate for primary care
Case
• Jane - healthy 26 year old
• Office visit for a routine pap smear and renewal of
birth control pills
• Family History (any cancer in the family?)
– Mother with breast cancer at 66
– Father’s side of the family:
– uncle - CA kidney age 72
– uncle - CA colon age 56
– aunt - double primary: endometrial CA age 45, colon CA age 68
– 1 cousin - endometrial CA age 40
– 2 cousins - both have colon CA
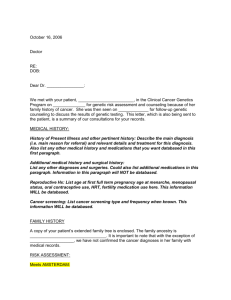
LEGEND
Family history
Kidney
Colon
Endometrial
Breast
Accident
Mary
Dx 45 CA
Endometrial
A&W Bob Dx 56
CA colon
Stroke
Nat Causes
Steve Dx 72
Kevin, 67
CA Kidney
A&W
Paula Dx 66
CA- Br
MI 72
A&W
A&W
A&W
Dx 68 CA Colon
Linda Dx 38
CA - colon
Jeana Dx 40 Ca- Christa Dx 52
Endometrial
CA – Colon
Jane, 26
A&W
A&W
What is Lynch syndrome?
• Lynch syndrome (LS), also known as Hereditary Non-Polyposis
Colorectal Cancer, (HNPCC), is an inherited cancer predisposition
syndrome
• Individuals with LS have a greatly increased risk for certain
cancers
• LS accounts for about 0.7-3.6% of cases of CRC
• Research on LS-related endometrial cancer is still emerging;
current data suggest that in North America between 1.8% and
4.5% of cases are attributed to LS
LYNCH SYNDROME-RELATED CANCERS
Colorectal
Endometrial
Ovarian
Pancreatic
Ureter
Brain
Renal
Gastric
Small bowel
Hepato-biliary
Sebaceous (adenoma or carcinoma)
What do I need to know about the genetics
of Lynch syndrome?
• Autosomal dominant
• Reduced penetrance and variable expressivity
Mismatch
genes play
an inherit
important
role in a cell’s
to repair
– not allrepair
individuals
who
a mutation
in ability
a Lynch
DNA damage as a cell grows and divides, by identifying and removing
syndrome gene will develop cancer (reduced penetrance)
single nucleotide mismatches, insertions and deletion loops. Defects in
– signs
symptoms/type
and onset
of cancerinwill
the
MMR and
pathway
lead to an accumulation
of mutations
a cellvary
which
maybetween
result in aaffected
malignancy
family members (variable expressivity)
• Caused by an inherited mutation in at least one of
four mismatch repair (MMR) genes* (MLH1, MSH2,
MSH6 or PMS2) or in EPCAM
Who should be offered genetic testing?
• Currently the decision to offer genetic testing is
made in the setting of a genetics consult at a
hereditary cancer program or a general genetics
clinic
• If possible, the affected individual in the family at
highest risk to carry a mutation is offered testing first
in order to maximize the likelihood of detecting a
mutation
– This would usually be a young individual with CRC or
another Lynch syndrome-associated cancer
Red Flags for hereditary cancer
• There are multiple family members with cancer
– Same side of family
– Diagnoses occur at a younger than expected age
– Several generations are affected
• Clustering of certain types of cancers
• Multiple primary cancers in same individual
Family history Red Flags
for a CRC syndrome
• A patient is considered to be at high risk for Lynch
syndrome (LS) if he/she has:
– A known LS-causing mutation in the family
OR
– At least three relatives with an LS-associated cancer; the
following criteria should also be present:
• One must be a first degree relative of the other two;
• At least two successive generations must be affected (autosomal
dominant inheritance);
• At least one relative with LS-related cancer should be diagnosed
before age 50;
– Tumour pathology should be verified when possible and other CRC
syndromes should be ruled out
What does the genetic test result mean?
• If your patient has been found to carry a mutation in a Lynch
syndrome gene (a positive result)
– he/she has an increased lifetime risk to develop certain cancers
– family members are at risk of carrying the same mutation and of
having similar cancer risks
• If a mutation is not identified and testing was for a known
familial mutation (true negative)
– Your patient is not considered to be at increased risk of developing
hereditary cancer
• If a mutation is not identified in an affected patient who has
no known familial mutation (uninformative result) or when a
variant of uncertain significance (VUS) is identified
– The diagnosis of Lynch syndrome is not confirmed or ruled out, even in
families with a strong history of CRC
A VUS is a gene change that has not yet been classified as pathogenic or benign
Cancer type
Colorectal
Endometrial
Stomach
Ovarian
Hepato-biliary tract
Urinary tract (ureter
and renal pelvis)
Small bowel
Brain/ central nervous
system
Sebaceous neoplasm
Pancreas
Lynch syndrome lifetime cancer risk
(carrier of a MLH1 or MSH2 gene
mutation)
General Population
lifetime cancer risk
to age 70
Risk
Mean age at
diagnosis
Risk
52-82%
25-60%
6-13%
4-12%
44-61 years
48-62 years
56 years
42.5 years
5.5%
2.7%
<1%
1%
1-4%
1-4%
Not yet reported
55 years
<1%
<1%
3-6%
1-3%
49 years
50 years
<1%
<1%
1-9%
1-6%
Not yet reported
Not yet reported
<1%
<1%
How do I order the genetic test?
• Genetic testing is generally performed on a
blood sample
• Specifics will depend on your region. Details
can be found at www.geneticseducation.ca
How will genetic testing help you
and your patient?
• Positive result:
– Clinical intervention may improve outcome
– Family members at risk can be identified
– Positive health behaviour can be reinforced
– Reduction of uncertainty
• True negative:
– Avoidance of unnecessary clinical interventions
– Emotional - relief
– Children can be reassured
Are there harms or limitations of genetic
testing?
• Positive result:
– Adverse psychological
reaction
– Family issues/distress
– Uncertainty - incomplete
penetrance
– Interventions may carry
risk
– Discrimination
• Job, insurance
– Privacy, confidentiality
• True negative:
– Adverse psychological
reaction (i.e. survivor guilt)
– Dysfunctional family
dynamics
– Complacent attitude to
health
• Uncertain result:
– Complacent attitude to
health
– Uncertainty
– Continued anxiety
Screening and surveillance
• In general, for high risk individuals (carriers of a Lynch
syndrome gene mutation and their first degree relatives who
have not yet had genetic testing):
• Colorectal Cancer
– Colonoscopy every 1-2 years beginning between ages 20 and 25 or 2-5 years
prior to the earliest colon cancer in the family if that diagnosis was made
before age 25 years, whichever is earlier
• Endometrial and Ovarian cancer
– Education about the symptoms of endometrial cancer
– Annual transvaginal ultrasound and endometrial biopsy (limited evidence)
– Prophylactic hysterectomy and bilateral salpingo-oophorectomy (for women
who have completed childbearing)
• Other Extracolonic cancers
– Family history dependent
Screening and surveillance
• For patients who have a known mutation in a Lynch
syndrome gene
– Genetics healthcare provider or oncologist may provide
recommendations specific to the patient and his/her family history
• For patients who have a true negative result
– Provincial guidelines for population risk CRC screening should be
followed i.e. Fecal Occult Blood Test every two years from age 50
– For those individuals who have a family history of CRC unrelated to the
mutation in their family (i.e. on the other side of the family), screening
recommendations would be based on family history.
• For patients with an uninformative result or a VUS
– Recommendations will be based on a combination of factors, such as
family history and, in cases where a VUS was identified, information
about the VUS
VUS – Variant of uncertain significance
Screening and surveillance
• Screening recommendations for individuals at increased risk to
develop CRC and who do not meet high risk, Lynch syndrome criteria
Criteria
Recommendation
One 1st degree relative with a CRC diagnosis less than
age 50 (older than age 35)
Colonoscopy beginning at age 40 OR 10 years younger than the youngest
CRC diagnosis. Repeat every 3-5 years depending on family history and
findings.
OR
Two 1st degree relatives with CRC diagnoses at any age
A 1st degree relative with a CRC diagnosis at age 50 or
older
Colonoscopy beginning at age 50 OR 10 years younger than the earliest CRC
diagnosis. Repeat every 5 years, depending on family history and findings.
One 2nd degree relative with a CRC diagnosis less than
age 50
Colonoscopy beginning at age 50. Repeat depending on findings.
A 1st degree relative with advanced adenomas
Colonoscopy beginning at age 50 OR at age of detection, whichever is first.
Repeat depending on findings.
A personal history of colorectal adenomatous polyps
Colonoscopy repeated every 3-5years depending on findings.
A personal history of inflammatory bowel disease
Initiate screening 8-12 years after onset of symptoms (consult specialist),
with colonoscopy every 1-2 years. Management is dependent upon
findings.
Screening and surveillance
• For patients who are at general population
risk (no symptoms of CRC and no family
history of CRC, or negative test result for a
known Lynch syndrome gene mutation in the
family), recommendations should follow
provincial guidelines
– i.e. Fecal Occult Blood Test q2 years from age 50
Pearls
• Lynch syndrome (LS) is the most common hereditary colorectal
cancer predisposition syndrome
• It is an autosomal dominant condition that results in an
increased lifetime risk of CRC in addition to other cancers
• Individuals at high risk of LS should be referred for a genetic
consultation for consideration of genetic testing
– Consult your local genetics or hereditary cancer centre if you are unsure
of your patient’s eligibility
• Surveillance and management of CRC and other cancers should
be guided by genetic test results and/or family/ personal history
– Studies show that conversations between patients and their healthcare
providers are the strongest drivers of screening participation
LEGEND
Family history
Kidney
Colon
Endometrial
Breast
Accident
Mary
Dx 45 CA
Endometrial
A&W Bob Dx 56
CA colon
Stroke
Nat Causes
Steve Dx 72
Kevin, 67
CA Kidney
A&W
Paula Dx 66
CA- Br
MI 72
A&W
A&W
A&W
Dx 68 CA Colon
Linda Dx 38
CA - colon
Jeana Dx 40 Ca- Christa Dx 52
Endometrial
CA – Colon
Jane, 26
A&W
A&W
References
•
•
•
•
Kohlmann W, Gruber SB. Lynch Syndrome. 2004 Feb 5 [Updated 2012 Sep 20]. In:
Pagon RA, Adam MP, Bird TD, et al., editors. GeneReviews™ [Internet]. Seattle
(WA): University of Washington, Seattle; 1993-2013. Available from:
http://www.ncbi.nlm.nih.gov/books/NBK1211/ [Accessed April 4, 2014]
Referenced with permission from the NCCN Clinical Practice Guidelines in
Oncology (NCCN Guidelines®) for Colorectal Cancer Screening V.2.2013© National
Comprehensive Cancer Network, Inc 2013. All rights reserved. Accessed [Month
and Day, Year]. To view the most recent and complete version of the guideline, go
online to www.nccn.org. NATIONAL COMPREHENSIVE CANCER NETWORK®,
NCCN®, NCCN GUIDELINES®, and all other NCCN Content are trademarks owned by
the National Comprehensive Cancer Network, Inc.
Leddin D et al. Canadian Association of Gastroenterology and Canadian Digestive
Health Foundation: Guidelines on colon screening. Can J Gastroenterol 2004;
18(2): 93-99
Lynch HT et al. Review of the Lynch syndrome: history, molecular genetics,
screening, differential diagnosis, and medicolegal ramifications. Clin Genet 2009;
76(1):1-18.