10d PPT Herd Immunisation
advertisement
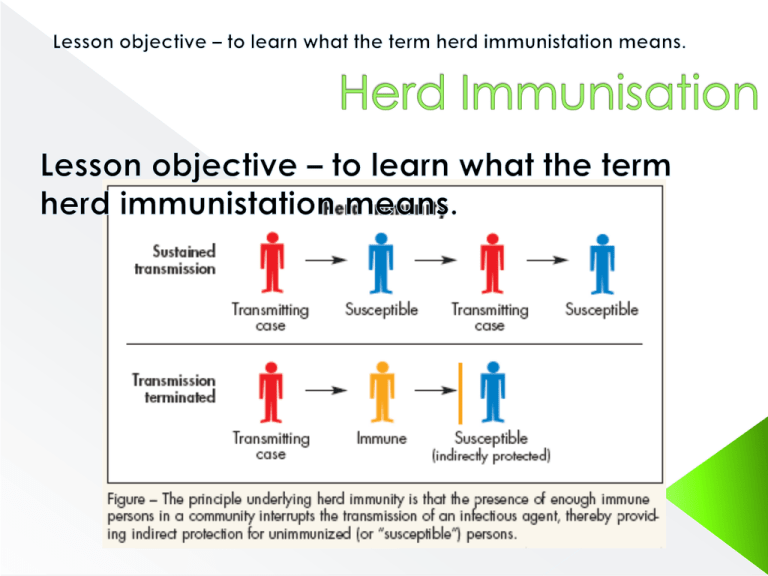
immunisation against various deadly diseases is an important preventive measure which the doctors recommend right from the birth. Behind the program schedule of vaccination there is a definite science and policy and such preventive measures help in the long run to protect the whole human community from diseases and infections. When non immunized people live with community of people who are immunized they are indirectly protected from getting inflicted from any disease. This is called as herd immunity or community immunity. According to herd immunity theory when sufficient amount of people in a particular group or community is immune to a certain type of disease, it acts as a barrier for other non immunized people as well. Due to this people who are not vaccinated too are protected. When my oldest child was a baby, after telling the health visitor I didn’t vaccinate, she promptly exclaimed, “Oh well, she’s lucky as she has herd immunity from the vaccinated children to protect her!” She then went on to say that not everyone had the luxury of my decision because if less than 95% of children were vaccinated, then it wouldn’t work anymore. I thought this was a silly concept because if vaccination truly worked, then any child who was vaccinated would be protected from disease, no matter how many ‘infectious’ unvaccinated kids there were, and if the 95% herd immunity figure was a genuine argument, it only points to one thing: the medical profession don’t really believe in the effectiveness of their own vaccines. What Is The Herd Immunity Theory? The herd immunity theory was originally coined in 1933 by a researcher called Hedrich. He had been studying measles patterns in the US between 1900-1931 (years before any vaccine was ever invented for measles) and he observed that epidemics of the illness only occurred when less than 68% of children had developed a natural immunity to it. This was based upon the principle that children build their own immunity after suffering with or being exposed to the disease. So the herd immunity theory was, in fact, about natural disease processes and nothing to do with vaccination. If 68% of the population were allowed to build their own natural defences, there would be no raging epidemic. Later on, vaccinologists adopted the phrase and increased the figure from 68% to 95% with no scientific justification as to why, and then stated that there had to be 95% vaccine coverage to achieve immunity. Essentially, they took Hedrich’s study and manipulated it to promote their vaccination programmes. Mass immunisation concept deals both with utilitarianism and herd immunity and hence is centrally correlated. Utilitarianism is a sort of faith in which it is believed that that act or rule is of greater use or worth which provides maximum security to optimum number of people. On the other hand herd immunity is the extent of immunity towards a particular disease a group or community of people have. Both the terms hence are applicable and correlated to the concept of mass immunization. Utilitarianism deals with greatest people and security whereas herd immunity believes that if maximum people are immunized against a particular disease, practically all people from that group are protected as well. What is a good example of herd immunity? The most common example in this regard is that of chicken pox which is a contagious disease and spreads rapidly. Children and even adults who never had vaccination of chicken pox are more vulnerable to this disease. But if everyone in the near proximity are immunized against chicken pox, then the possibility of passing of this infection is minimized as the virus of chicken pox is blocked from spreading further. This type of herd immunity works incredibly well in children suffering from leukemia. These children are immunosuppresed children and cannot be vaccinated with the chicken pox vaccination as the vaccine virus and wild virus can prove fatal to the child due to his low immunity. But if such children are kept in immunized group, they can be benefitted by herd immunity protection. Why Vaccine Induced Herd Immunity is Flawed? If vaccination really immunises, then your vaccinated child will be immunised and therefore protected against any disease an unvaccinated child gets. If he isn’t, his shots didn’t work. We should also examine whether or not the vaccines actually do provide immunity and in which populations epidemics occurred. Was it the unvaccinated children spreading disease as they would have parents believe? Or were those epidemics already in previously vaccinated people? To do this I have listed several epidemics that have occurred in the last 100 years or so, including Smallpox, which medics claim that vaccination eradicated. Vaccines work by stimulating our immune system to produce antibodies (substances produced by the body to fight disease) without us actually becoming infected with the disease. Vaccines trigger the immune system to produce its own antibodies against disease, as though the body has been infected with it. This is called 'active immunity'. If the vaccinated person then comes into contact with the disease itself, their immune system will recognise it and immediately produce the antibodies needed to fight it. Newborn babies are already protected against several diseases, such as measles, mumps and rubella, because antibodies have passed into them from their mothers via the placenta. This is called ‘passive immunity’. When a vaccination programme is introduced, everyone in the population of a certain age or risk group is offered a specific vaccine to try and reduce disease. Vaccination programmes aim to protect people for life. They often concentrate on young children, as they’re especially susceptible to many potentially dangerous infections. Some vaccination programmes are targeted at older people or certain risk groups. When a vaccination programme against a disease begins, the number of people catching the disease goes down. But as the threat recedes it’s important to keep vaccinating, otherwise the disease can start to spread again (scroll down to http://www.nhs.uk/Video/Pages/vaccinationanimation.aspx The first step is to make the organism (called the pathogen) that produces the disease. The pathogen is a virus or a bacterium. Viruses and bacteria can be mass produced in the laboratory by infecting cells grown in tissue culture. The pathogen must then be altered to ensure that it doesn’t trigger the disease itself. This can be done by: weakening, or ‘attenuating’ it by growing it repeatedly to select a strain that's less dangerous. MMR vaccines are attenuated taking out the part of the pathogen that causes the immune response and using this in the vaccine. The Hib vaccine is made in this way using the toxin that the pathogen makes and inactivating it. The tetanus vaccine is produced in this way The treated pathogen is then combined with other ingredients, such as stabilisers and preservatives, to produce a dose of vaccine. How long does a vaccination last? In many cases vaccination provides lifelong protection against a disease but it varies. How long a vaccination lasts will depend on the disease that the vaccine protects against, the vaccine, and the person who is vaccinated. Some vaccines provide very high levels of protection - for example MMR provides 90% protection against measles and rubella after one dose. Others are not as effective – for example typhoid vaccine (a travel vaccine) provides about 70% protection over three years. http://www.nhs.uk/Video/Pages/Vaccinationanimation2.aspx Case Study - A measles outbreak in Gibraltar has infected almost 1 percent of the territory’s 28,000 people in just three months, according to a report by its public health director. The outbreak, mostly in schoolchildren, made it clear that the authorities had been wrong in assuming that more than 90 percent of children had had measles shots, the report said. Gibraltar is a British territory, and resistance to the measles-mumps-rubella vaccine has been high in Britain since a 1998 report in The Lancet speculated that it could cause autism. That report has been widely discredited, and numerous later studies showed no link between vaccines and autism. Nonetheless, as a consequence of dropping vaccination rates, Britain has had several local measles outbreaks. There were 276 cases of measles in Gibraltar from August to October, according to the health director, Dr. Vijay Kumar. There were none in the previous 10 years. The patients’ age range was 4 months to 58 years. Most cases were mild. Gibraltar’s inhabitants live in modern but unusually crowded conditions for Western Europe. Gene analysis suggested that the virus came from an outbreak in the nearby Spanish town of Algeciras. Gibraltar began a vaccination campaign this summer, but the vaccine ran out twice because of shortages in Britain. http://www.historyofvaccines.org/cont ent/herd-immunity-0 Chickenpox is caused by the varicellazoster virus (VZV), which only infects humans and some higher primates.