- Department of Community Medicine ACME Pariyaram
advertisement

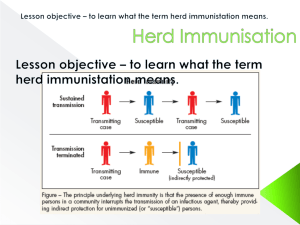
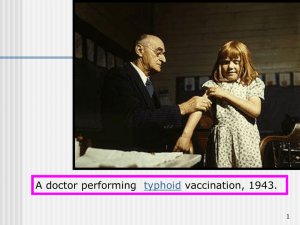
Specific defences : Micro organism-breach local defense systems host recognize, destroy and eliminate antigenic material foreign to its own Specific defenses are 1.Active immunity – humoral, cellular , combined immunity 2.Passive immunity – normal human Ig, specific human Ig, animal antitoxin or antisera Active immunity - Immunity developed as a result of infection or by specific immunization and is usually associated with the presence of Ab or cells having specific action on micro organism or its toxin. - Immunity produced is specific for particular diseases Active immunity may be acquired by following : -clinical infection -sub clinical or in apparent infection -immunization with an antigen THE IMMUNE RESPONSE A. Primary response: -Ag first time administer IgMAb -----IgGAb -Nature and extend of primary response to an Ag is determined by factors like -Dose of Ag, nature of Ag, route of administration, nutritional status of the host etc. Following primary response RES is educated . There s production of memory cells by both B & T lymphocytes These cells are responsible for immunological memory which become established after immunization In fact purpose of immunization is to develop immunological memory. B. Secondary (booster) response: -secondary response involve production of both IgM & IgG antibody Response to booster dose differs in a no. of ways from primary response (a) Production of Ab more rapid (b) Ab response maintained at higher level for a long period of time (c) Ab tends to have a greater capacity to bind to Ag Humoral immunity It comes from B cells (bone marrow derived lymphocytes) which proliferate and manufacture specific Ab after Ag presentation by macro phages Immunoglobulin's are divided into 5 classes – IgG, M,A,D &E . they circulate in body and neutralizes the microbes/toxins Ab are specific- they react with same Ag when provided Cellular immunity Some micro organism like M.Leprae , M.TB escape humoral immunity and can multiply in macrophages . However these macrophages can be stimulated by Tlymphocytes. The activated macrophages perform a much more efficient phagocytic function than non- activated macrophages T cells do not secrete Ab , but they are responsible for recognition of Ag Combination of both In some cases they jointly helps in immunity Vaccine to be effective must ellicit both cell mediated and humoral responses Active immunity takes time to develop . It is superior to passive immunity because (a) duration of protection is long lasting (b) With few exceptions severe reactions are rare (c) Protective efficiency is better than passive (d) Active is less expensive Passive immunity Ab produced in one body ( human / animal ) are transferred to another to induce protection against disease That is, they are ready made Ab Passive immunity may be induced by (a) Ig or anti serum administration (b) Ab through placenta , human milk (IgA) Passive immunity differ from active immunity by (a) Immunity is rapidly established (b) Immunity produced is only temporary ( days to months ), till when Ab is eliminated from the body (c) There is no education of RES Herd immunity It is the level of resistance of a community or a group of people to a particular disease Eg: polio vaccine-------, chickgunya in Alappuzha Elements contributing to herd immunity (a) Occurrence of clinical or sub-clinical infection in herd (b) Immunisation of the herd (c) Herd structure If herd immunity high enough , occurrence of epidemic is highly unlikely Herd immunity is maintained by immunisation Eg: polio , diphtheria With no vaccine for small pox herd immunity is declined Immunising agents Vaccines- substances-designed to produce specific protection against a given disease It stimulate production of protective Ab (a) Live vaccine (attenuated ) Prepared from live organisum . Doesn’t have the property of phathogenicity but retained immunogenicity Should not be administered to immune deficient people, pregnancy If two live vaccine required – either given at two sites simultaneously or with an interval of at least three weeks Should be properly stored Usually require only one dose , exception of polio Eg: polio , BCG , measles , rubella (b) Inactivated / killed vaccine Virus is killed with heat or chemicals and infected into the body to stimulate active immunity They are usually safe but less efficacious than live vaccines Usually require more than two to three primary and even a booster dose to produce adequate Ab response Usually administered i/m or s/c Only severe C/I is severe local or general reaction to previous dose Eg: pertusis , IPV, typhoid Toxoid: Exotoxins produced by certain organisum are detoxicated and used to prepare vaccines These Ab produced neutralises the toxin moiety produced during infection and not the organism Highly efficacious and safe Eg : tetanus and diphtheria Cellular fraction: Prepared from extracted cellular fractions like cell wall, capsule etc Efficacy and safety high Eg : meningiococcal, pneumococcal Combination: Simplify administration, reduce cost, minimise no. of contact of patient with health system Eg : DPT , MMR, Pentavalent Polyvalent : prepared from two or more strains of same species . Eg : polio infuenza Autogenous vaccine : organism in vaccine is obtained from the same patient Vaccine can be plain , adjuvant , freeze dried preparation Adjuvant is added to vaccine with an intent of potentiating the immune response.eg : aluminium phosphate, aluminium hydroxide Freeze dried vaccines ( BCG , Measles , YF) are more stable preparations than liquid vaccines Immunoglobulin Composed of five major classes and its sub units- IgG,M,D,A,E Ig preparations : two types (a) Normal human Ig (b) Specific human Ig – usually made from plasma of patients who have recently recovered from infection Live vaccine should not be given normally for 12 weeks after giving normal human Ig and if already given NHIg should be differed for 2 weeks Eg : Hep A, Hep B, Tetanus, Rabies Antisera and antitoxins They are materials prepared in animals ( horses) Passive immunization is achieved Eg: tetanus, snake bite, diphtheria Cold chain It is the system of storage – transportation of vaccines from the manufature to the actual vaccination site Polio is most sensitive to heat among vaccines requires storage at -20 degree C. Vaccine stored in freezer compartment are polio and measles Vaccine in cold part but never allow to freeze are ‘T’ series vaccine, DPT, TT,DT,BCG & diluents Vaccine should be protected from sunlight and anti septics If refrigerated temperature is kept between 2 and 8 degree C vaccines (except polio) can be stored upto 5 weeks Reconstituted BCG and measles are kept +2 to +8 degree C for max, of 4 hours and JE vaccine upto 2 hours Return the unused vaccine vial to PHC from site on the same day in cold chain Discard vaccine that are unused more than 3 times Cold storage equipment (a)Walk-in cold room: Located at regional level meant to store up to 3 months Serve 4 to 5 districts (b) Deep freezer: supplied to all districts (large) & PHC (small) Cabinet temperature is -15 to -25 degree C In case of power failures they can maintain cabinet temperature upto 18 to 22 hours At PHC level deep freezer are used only for ice pack preparation and not for vaccine storage ( c) Ice lined refrigerator ( ILR): Kept at district ( large) and PHC (small) Cabinet temperature is maintained at +2 to +8 At PHC, ILR are used to store vaccines ILR are lined with tubes or ice packs to maintain internal temperature ILR can keep vaccine safe with 8 hours of continuous electricity supplied in a 24 hour period They are top opening – can hold cold air inside better than front opening Vaccine kept in basket along with diluents Keep spaces with boxes A dial thermometer is kept in ILR and temperature is recorded twice a day In case of electric supply failure or during defrosting vaccines transferred to cold boxes DO’S - keep away from direct sunlight and 10 cm away from wall , keep voltage stabiliser, keep equipment levelled , keep space between vaccines for air circulation, open only when necessary, defrost periodically DONT’S – Not to keep anyother equipments drugs ,food, water inside it Discard expired vaccine (d) Cold boxes : Supplied to all peripheral centers Used mainly for transportation of vaccines Ice pack are placed at bottom and sides Vials of DPT , DT , TT & diluents should not be placed in direct contact with frozen ice packs (e) Vaccine carrier: Used to carry small quantities of vaccine ( 16 to 20 vials) 4 frozen ice pack are used for lining the sides (f) Day carrier : Used to carry small quantity (6 to 8 vials) 2 frozen ice packs are to be used Used only for few hours (g) Ice packs: Only water is filled upto the level marked If leaking discarded -risk of cold chain failure is greatest at sub-centre level. Hence , vaccines are not stored there. Vaccine vial monitor(VVM) Adverse events following immunization(AEFI) (a) Vaccine reaction (b) Programme error (c) Coincidental (d) Injection reaction (e) Unknown --precautions to be taken Contra indications of vaccine NIS- national immunization schedule UIP – universal immunization programme – infancy EPI – expanded programme on immunization – till 5 years Pulse polio immunization Catch up- keep up- follow up