DiGeorge`s syndrome
advertisement

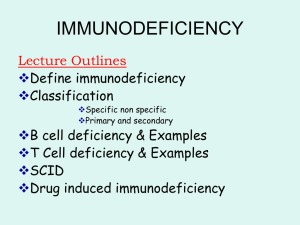
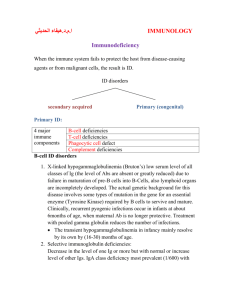
Pathophysiology of Immunodeficiency Diseases Host Defense Mechanisms • • • • • Skin and mucosal barriers Humoral immunity (B cells, plasma cells, Ab) Cell-mediated immunity (T cells) Phagocytosis Complement Overview of Immunodeficiency Disorders. The defect might be In the level of stem cell or in any other level of tree Introduction. • Immunodeficiency diseases are : A diverse spectrum of illnesses due to various abnormalities of the immune system • Prevalence : Primary (congenital) 1 : 10,000 to 1 : 200,000 present at birth . Secondary (acquired) is more common . Origins of Immunodeficiency o Primary or Congenital Inherited genetic defects in immune cell development or function, or inherited deficiency in a particular immune component o Secondary or acquired A loss of previously functional immunity due to infection, toxicity, radiation, splenectomy, aging, malnutrition, etc. Primary or acquired. can affect. Natural immunity (non-specific body defenses). Phagocytic cells. Complement proteins. Acquired immunity. (specific body defenses). T-cells. B-cells. Immunodeficiency / Immunocompromised States Primary – Intrinsic abnormality of one or more components of the Immune System • >150 Conditions Characterised • Individually, uncommon, but important to recognise • Range from global, overwhelming immune failure ( SCID) to subtle defects in individual components of function • 1/ 10,000 live births • Look for infections that are: Frequent Suspecting Immunodeficiency Recurrent/chronic Unusual organisms: aspergillous, nocardia Organisms that respond poorly to therapy Unusual site: liver abcess, brain abcess Severity of infection The Ten Warning Signs of Primary Immunodeficiency 1 8 or more ear infections within 1 year Recurrent, deep skin or organ abscesses 2 2 or more serious sinus infections within 1 year Persistent candidiasis after the age of 1 year 7 3 2 or more months on antibiotics without resolution Need for I.V. antibiotic to clear infections 8 4 2 or more pneumonias within 1 year 2 or more deep-seated infections 9 5 Failure to gain weight or grow normally A family history of Primary Immunodeficiency 6 10 Classification of Primary Immunodeficiency 1. Antibody 2. deficiencies Cellular deficiencies 3. Phagocytic disorders 4. Complement deficiencies 5. Combined Immunodeficiencies HUMORAL Immunodeficiencies (B-cell defects) Antibody deficiencies include: Common variable immunodeficiency (CVID) X-linked agammaglobulinemia (XLA) Selective IgA deficiency (SIgAd) Selective IgG subclass deficiency (SIgGsd) Hyper IgM syndrome (HIgM) Transient hypogammaglobulinemia of Infancy (THI) Functional antibody deficiency Early B-cell differentiation . Lesions can occur at any site in the pathway of B-cell development. B-cell defect could be in any level in the pathway B-cell Defect Onset after maternal antibodies diminish Usually after 5-7 m/o, later childhood to adulthood Bacteria: pneumococci, staphylococci, Hemophilus, campylobacter, mycoplasma Virus: entovirus Recurrent sinopulmonary infections, chronic GI symptoms, malabsorptions, arthritis, entroviral meningoencephalitis X-linked agammaglobulinaemia(bruton) In X-LA early maturation of B cells fails Affect males Few or no B cells in blood Very small lymph nodes and tonsils No Ig Recurrent pyogenic infection IgA deficiency Serum IgA level < 10 mg/dl Prevalence :1:700 , the most common PID Most are asymptomatic , but have Increased rate of respiratory tract infection (R.T.I ) Some have recurrent Symptoms G.I.T. , Urogenital tract Because of lack of secretion of IgA on the mucous membrane of GIT and respiratory tract Increased incidence of allergic and autoimmune diseases Anti - convlusant drugs (phenytoin) may cause secondary deficiency 2- IgA and IgG subclass defeciency About 20% lack IgG2and IgG4 Susceptible to pyogenic infection Result from failure in terminal differentiation of B cells 3- Immunodfeiciency with increased IgM (HIgM) Low or absent levels of IgA, IgG , IgE Production of large amount of IgM >200mg/dl of polyclonal IgM Susceptible to pyogenic infection Due to inability of B cells to isotype switching They have B cell 4- Common Variable Immunodeficiency (CVID) There are defect in T cell signaling to B cells Acquired agammaglobulinemia in the 2nd or 3rd decade of life Pyogenic infection 80% of patients have B cells that are not functioning B cells are not defective but donot differentiate into immunoglobulin producing cell and fail to receive signaling from T lymphocytes Risk of autoimmune disease and malignancy 5- Hypogamaglobulinaemia of infancy Due to delay in in IgG synthesis approximately up to 36 months In normal infants synthesis begins at 3 months Normal B lymphocytes Probably lack help of T lymphocytes Immunoglobulin Levels vs. Age Cellular Immunodeficiencies Cellular deficiencies include: Combined immunodeficiency (CID) Severe combined immunodeficiency (SCID) Ataxia-Telangiectasia syndrome (AT) Wiskott-Aldrich syndrome (WAS) DiGeorge syndrome Chronic mucocutaneous candidiasis (CMCC) DiGeorge's syndrome It the most understood T-cell immunodeficienc Also known as congenital thymic aplasia/hypoplasia Associated with hypoparathyroidism, congenital heart disease, fish shaped mouth. Defects results from abnormal development of fetus during 6th-10th week of gestation when parathyroid, thymus, lips, ears and aortic arch are being formed Combined T & B Immunodeficiencies SEVERE COMBINED IMMUNODEFICENCY In about 50% of SCID patients the immunodeficiency is xlinked whereas in the other half the deficiency is autosomal. Early onset( 2-6 m/o) Lymphopenia((< 2500 in infants) They are both characterized by an absence of T cell and B cell immunity and absence (or very low numbers) of circulating T . Very small thymus, no lymph node , no tonsil Patients with SCID are susceptible to a variety of bacterial, viral, mycotic and protozoan infections. The x-linked SCID is due to a defect in gammachain of IL-2 also shared by IL-4, -7, -11 and 15, all involved in lymphocyte proliferation and/or differentiation. The autosomal SCIDs arise primarily from defects in adenosine deaminase (ADA) or purine nucleoside phosphorylase (PNP) genes which results is accumulation of dATP or dGTP, respectively, and cause toxicity to lymphoid stem cells Ataxia-telangiectasia A complex of immunologic, neurologic, endocrinologic, hepatic and cutaneous abnormalities ataxia(10-12y/o) ,telangiectasis (3-6 y/o) Mutation in ATM gene T-cells and their functions are reduced to various degrees. B cell numbers are normal to low. Low levels of IgA, IgE, high level of IgM There is a high incidence of malignancy, particularly lymphoreicular & adenocarcinoma Wiskott-Aldrich syndrome (immunodeficiency with thrombocytopenia and eczema) X-linked xp11.22-11.23 WASP ; assemby of actin filaments required for microvesicle formation downstream of protein kinase C and tyrosine kinase signaling Low plaletlet, small size platelet Associated with normal T cell numbers with reduced functions, which get progressively worse. IgM concentrations are reduced but IgG levels are normal Both IgA and IgE levels are elevated. Boys with this syndrome develop severe eczema,bleeding tendency They respond poorly to polysaccharide antigens and are prone to pyogenic infection. Defects of the phagocytic system • Defects of phagocytic cells (numbers and/or functions) can lead to increased susceptibility to a variety of infections. • Bacteria,fungal infection • Skin and mucus membrane Cyclic neutropenia Autosomal dominant Mutation in ELA2(neutrophil elastase gene2) It is marked by low numbers of circulating neutrophil approximately every three weeks. The neutropenia lasts about a week during which the patients are susceptible to infection. The defect appears to be due to poor regulation of neutrophil production. Tx: r-GCSF ( granulocyte stimulating factor) Severe congenital Neutropenia (Kostman) Arrest in promyelocyte stage Neutrophil count< 200 Mutation ELA2 or HAX1, autosomal recessive or dominant Severe infections 20% prone to AML Tx: r-GCSF Shwachman Diamond Syndrome Mutation in SBDS gene Diarrhea, FTT, malabsorption till 4 m/o Eczema, recurrent infections Neutrophil count< 1000, pancytopenia Risk of AML Chronic granulomatous disease (CGD) • • • • • Defect in intra cellular killing Normal chemotaxis, ingestion Normal neutrophil count x-linked (65%)& autosomal recessive CGD is characterized lymphadenopathy, hepatosplenomegaly and chronic draining lymph nodes. • In majority of patients with CGD, the deficiency is due to a defect in NADPH oxidase that participate in phagocytic respiratory burst. • Infection with catalase positive organism: e coli, staph areus , fungal , nocardia, serratia Leukocyte Adhesion Deficiency LAD1, LAD2,LAD3 Autosomal recessive Defect in chemotaxis These molecules are involved in diapedesis and hence defective neutrophils cannot respond effectively to chemotactic signals. Neutrophilia >12,000 , with infection >100,000 Delayed umblical cord separation > 2 wk They don't have sign of inflammation such as swelling, warmth or pus formation Chediak-Higashi syndrome (granule sorting disorder) Mutation in lyst gene Giant granule in cytoplasm of neutrophils Respiratory burst is normal. Associated with NK cell defect, platelet and neurological disorders • • • • • Albinism(oculocutaneous) Repeated infections Mild bleeding tendency Peripheral neuropathy Prone to hemophagocytic syndrome Disorders of complement system Complement abnormalities also lead to increased susceptibility to infections. There are genetic deficiencies of various components of complement system, which lead to increased infections. The most serious among these is the C3 deficiency which may arise from low C3 synthesis or deficiency in factor I or factor H. Defect in classic pathway; AUTOIMMUNE DISEASE Congenital deficiency of C5, 6, 7, 8: > 50% MENINGOCOCCAL or GONOCOCCAL INFECTION( neisseria) Hyper IgE (Job) syndrome Autosomal dominant Symptoms/signs Coarse facial features/skeletal abnormalities Recurrent staph infections Impetigo (resistant) Pneumonia with pneumatocele formation Elevated IgE, Eosinophilia, Eczema PID - treatments • • • • • • Immunoglobulin replacement Bone Marrow Transplantation Gene-based therapies Antimicrobial management and prophylaxis Nutritional Support Patient Support Groups