ESBLs
advertisement
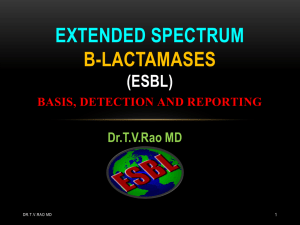
ESBL EXTENDED SPECTRUM BETA LACTAMASES DYNAMICS AND DETECTION Dr.T.V.Rao MD 1 DR.T.V.RAO SURVIVAL OF THE FITTEST Resistant bacteria survive, susceptible ones die Mutant emerges slowly 2 Sensitive cells killed by antibiotic Mutant’s progeny overrun PENICILLIN BETA LACTAM RING BETA LACTAMASES enzymes that inactivate the beta-lactam ring CEPHALOSPORIN Dr.T.V.Rao MD 3 BETA LACTAM RING ACTION OF A B-LACTAMASE S H2O N O Inactive penicilloate COOH S Active penicillin HN Dr.T.V.Rao MD OH COOH 4 O BASIS OF BETALACTAMSE ACTIVITY Dr.T.V.Rao MD 5 Time-delayed Growth. Betalactamase (red) is produced by the central colony, promoting growth of nearby, non-resistant colonies as it deactivates ampicillin (blue). Diffusion of beta lactamase through agar leads to time-delayed growth of non-resistant colonies B-LACTAM ANTIBIOTICS Penicillin's •Ampicillin •Piperacillin Beta-lactam/beta-lactamase inhibitors Dr.T.V.Rao MD 6 •Ampicillin/sulbactam •Amoxicillin/clavulanate •Ticarcillin/clavulanate •Piperacillin/Tazobactam PENICILLINS 1st gen – strep infection (G+) Ex. Penicillin, Cloxacillin Extended-spectrum – have broader spectrum against G- including E.Coli Ex. Amoxicillin With inhibitor would protect against some beta-lactamase producers Ex. Amoxicillin/Clav Dr.T.V.Rao MD 7 Broad spectrum – many Enterobacteriaceae Ex Piperacillin/Tazobactam Some beta-lactamases only inactivate a small number of antibiotics e.g. penicillin extended spectrum to all the penicillins and Others have cephalosporins e.g. cefuroxime, ceftriaxone (ESBLs) Dr.T.V.Rao MD 8 In addition may also carry resistance to other antibiotics e.g. ciprofloxacin. DEFINITION OF ESBL : Dr.T.V.Rao MD 9 Class A by Ambler or Group 2be by Bush classifications Typically, enzymes are plasmidmediated derived from older ßlactamases of TEM and SHV In early 2000s, CTX-M derived ßlactamases are included ESBL EVOLUTION Mid 1980s Variants of TEM and SHV Breakdown 3rd generation cephalosporins Mainly in hospital Klebsiella Dr.T.V.Rao MD 10 Spread world wide WHAT ARE EXTENDED-SPECTRUM Β-LACTAMASES? Dr.T.V.Rao MD 11 ESBLs are enzymes that mediate resistance to extended-spectrum (third generation) cephalosporins (e.g., ceftazidime, cefotaxime, and ceftriaxone) and monobactams (e.g., aztreonam) but do not affect cephamycins (e.g., cefoxitin and Cefotetan) or carbapenems (e.g., meropenem or imipenem). AMBLER CLASSIFICATION OF ΒLACTAMASES β-lactamases Active site Nucleotide sequence Serine-enzymes Zinc-enzymes C B A D Dr.T.V.Rao MD 12 Four evolutionarily distinct molecular classes WHAT IS A BETA-LACTAM? Abx • Penicillin • Cephalosporin • Monobactam • Carbapenem Bacteriocidal Dr.T.V.Rao MD 13 Google Images CEPHALOSPORINS 4th 3rd 2nd Willey, et al., 2008 Dr.T.V.Rao MD 14 1st CEPHALOSPORINS-USES 1st gen: strep, staph, G- including E.coli Ex. Cefazolin 2nd gen: greater spectrum against G- Ex. Cefoxitin 3rd gen: even greater activity, combat narrow-spectrum beta-lactamase producers ESBLs emerged Ex. Ceftazidime Dr.T.V.Rao MD 15 4th gen: effective against G- bacilli expressing Xm AmpC resistant to 3rd gen Ex. Cefepime OTHERS Monobactams Monobactams very active against Gincluding E.coli Ex. Aztreonam Carbapenems Dr.T.V.Rao MD 16 Carbapenems have an extremely broad spectrum. Cross-reactivity with penicillins or cephalosporins Ex. Imipenam THE FIGHT GOES ON .. Beta-lactam Beta-lactamase Beta-lactamase inhibitor Google Images Dr.T.V.Rao MD 17 ESBL COMMON ESBL PRODUCERS Klebsiella pneumoniae Escherichia coli Proteus mirabilis Enterobacter cloacae Dr.T.V.Rao MD 18 Non-typhoidal Salmonella (in some countries) THE FIGHT BETA-LACTAM PG Dr.T.V.Rao MD cell LYSIS 19 O N THE FIGHT BETA-LACTAMASE PG beta-lactamase Dr.T.V.Rao MD cell 20 O N THE FIGHT BETA-LACTAMASE PG O NH OH Dr.T.V.Rao MD 21 cell THE FIGHT BETA-LACTAMASE INHIBITOR PG beta-lactamase Dr.T.V.Rao MD Inhibitor cell 22 O N THE FIGHT BETA-LACTAMASE INHIBITOR PG beta-lactamase Inhibitor Dr.T.V.Rao MD cell LYSIS 23 O N ESBLS Enterobacteriaceae Resistance to oxyimino-cephalosporins and Monobactams but not cephamycins and carbapenem • Susceptible to beta-lactamase inhibitors •Genes SHV TEM CTX-M OXA Oteo, et al., 2010 Dr.T.V.Rao MD 24 AmpC Evolution of -Lactamases Plasmid-mediated TEM and SHV -lactamases Ampicillin 1963 1965 Extended-spectrum Cephalosporins 1970s 1983 1988 2000 Look and you will find ESBL D r . ESBL in Europe ESBL in USA > 130 ESBLs Worldwide 25 TEM-1 TEM-1 E.coli Reported in S.paratyphi 28 Gm(-) sp CLASSIFICATION OF Β LACTAMASES Richards and Sykes (1971) • substrate Ambler (1969) • structure Bush, Jacoby, Medeiros (1995) • Substrate; correlation with molecular structure • • • • • 150 TEM; 88 SHV; 88 OXA, 53 CTX-M; 22 IMP; Dr.T.V.Rao MD 26 • 12 VIM + smaller number of other enzymes (http://www.lahey.o CLASSIFICATION Ambler Classification • Molecular class A – D •A Bush-Jacoby-Medeiros Classification • Functional group 1 – 4 Paterson and Bonomo, 2005 Dr.T.V.Rao MD 27 •2 • 2b • 2be BETA-LACTAMASE INHIBITORS Dr.T.V.Rao MD 28 Resemble β-lactam antibiotic structure Bind to β-lactamase and protect the antibiotic from destruction Most successful when they bind the βlactamase irreversibly Three important in medicine •Clavulanic acid • Sulbactam • Tazobactam TEM ESBL CTX-M K1 Ceftazidime AmpC Hi-level R R v S Cefotaxime R v R S Cefoxitin R S S S Aztreonam R v v R Synergy + clav No +++ +++ No Dr.T.V.Rao MD Know the species 29 RESISTANCE AND GENETICS Why Test for β-lactamases ? Improve clinical outcome Inappropriate treatment leads to poor outcome Each 1 hour delay increases mortality by 7.6% in septic shock1 Encourage antimicrobial stewardship Spare carbapenems.. Reduce C. difficile / antibiotic associated diarhoea Enhanced surveillance Identify emerging resistance problems Develop structures to prevent dissemination Infection Control ‘Search and Destroy’ analogous to MRSA ? Laboratory Detection is not always easy… OR Rapid 1Kumar, Crit Care Med, 2006 TYPES OF ESBLS TEM SHV CTX-M Mutations OXA Dr.T.V.Rao MD 31 Plasmid-mediated ESBL Phenotype CHOICE OF INDICATOR CEPHALOSPORIN TEM & SHV – obvious resistance to ceftazidime, variable to cefotaxime CTX-M – obvious resistance to cefotaxime, variable to ceftazidime All ESBLs – obvious resistance to cefpodoxime Cefuroxime, cephalexin and 32 cephradine are unreliable indicators Livermore D and Woodford N HPA Guidance 2004 CURRENT MODERN METHODS CLSI – Clinical Laboratory and Standards Institute ARMRL - Antibiotic Resistance Monitoring and Reference Laboratory, Health Protection Agency Centre for Infections, London Commercial methods – Etest, BD Phoenix, Vitek Neo tabs & others Slide 33 EUCAST- European Society of Clinical Microbiology & Infectious Diseases DETECTION OF ESBLS Seek ceph/clav synergy in ceph R isolates Dr.T.V.Rao MD 34 •Double disc •Combination disc •Etest CHALLENGES FOR THE DIAGNOSTIC LAB Detection…. Hemophilus, Neisseria etc. Predicting -lactamase types. Have GNB got ?: ESBL, AmpC Metallo types, VIM, IMP etc… Spotting unusual patterns; knowing what to refer ??? DETECTION STRATEGY: STEP 1 Screen Enterobacteriaceae with : • Cefpodoxime- best general ESBL substrate Dr.T.V.Rao MD 36 • Cefotaxime & ceftazidime- good substrates for CTX-M & TEM/SHV, respectively COMBINATION DISK METHOD CARTER MW ET AL: J CLIN MICROBIOL 2000; 38: 4228 - 4232 Dr.T.V.Rao MD 37 Difference > 5 mm 38 Dr.T.V.Rao MD 39 Dr.T.V.Rao MD KLEBSIELLA PNEUMONIA PRODUCING A HIGHER The higher level of ESBL production is indicated by the inhibition of the β-lactamase by clavulanic acid and the resulting elliptical inhibitory zone between cefotaxime (CTX 5) and Augmentin (AMC 60). Dr.T.V.Rao MD 40 ACTIVITY ESBL Double disc antagonism for inducible AmpC Dr.T.V.Rao MD Ceftazidime 41 Cefoxitin AMPC INDUCIBILITY- WHEN TO LOOK Rarely!!!!! Risk is mutation, not inducibility per se Best to identify & predict risk from species Biggest risk Enterobacter & C freundii Avoid cephalosporins against them Identify means identify TO SPECIES LEVEL all Enterobacteriaceae (‘coliforms’) ex serious infections ESBLS DETECTION METHODS: INHIBITION BY CLAVULANIC ACID Co-amoxiclav disc surrounded by cefotaxime, ceftriaxone, ceftazidime and aztreonam discs (30 mcg each) 43 ESBL DETECTION Dr.T.V.Rao MD 44 – Screen cefpodoxime ; cefotaxime & ceftazidime – Synergy test with ceph/clav Combination discs are most cost effective synergy tests; Etests a good alternative.. or automate ESBL Confirmatory Test Positive for ESBL Ceftaz Dr.T.V.Rao MD Cefotax 45 Ceftaz/CA Cefotax/CA 45 ESBL CONFIRMATORY TEST NEGATIVE FOR ESBL Ceftaz Dr.T.V.Rao MD Cefotaxime/CA Cefotax 46 Ceftaz/CA 46 ESBL CONFIRMATORY TEST Dr.T.V.Rao MD Ceftaz 47 Etest Ceftaz/CA 47 ESBLS: TIMES A’ CHANGING WITH CTX-M Old advice- test ceftazidime; ESBL test if R New advice- test ceftazidime & cefotaxime; ESBL test if R to either • Still true- Only testing cefuroxime is inadequate Dr.T.V.Rao MD 48 • Alternative- test cefpodoxime; ESBL test if R COMPARING DISK DIFFUSION WITH MINIMUM INHIBITORY CONCENTRATIONS MICs cefpodoxime < 22 mm cefpodoxime > 2 µg/ml ceftazidime < 22 mm ceftazidime > 2 µg/ml aztreonam < 27 mm aztreonam > 2 µg/ml cefotaxime < 27 mm cefotaxime > 2 µg/ml ceftriaxone < 25 mm ceftriaxone > 2 µg/ml Dr.T.V.Rao MD 49 Disk diffusion ESBL CONFIRMATORY TESTS • 5 mm enhancement of the inhibition zone of antibiotic/CA combination vs antibiotic tested alone = ESBL Dr.T.V.Rao MD 50 Double-disk synergy (DDS) test • CAZ and CAZ/CA disks • CTX and CTX\CA disks • Confirmatory testing requires using both CAZ and CTX alone and with CA SYNERGY TESTS WITH 4-GEN CEPHALOSPORINS Cefepime/clav (Mast & AB Biodisk) Cefpirome clav (Oxoid) • Devt. driven by spread of clonal E. aerogenes with TEM-24 in Belgium & France • Cefpirome & cefepime products need comparison Dr.T.V.Rao MD 51 • Sensitivity for weak ESBLs remains to be proven PITFALLS IN ESBL DETECTION •Methods optimised for E. coli & Klebsiella •More difficult with Enterobacter – clavulanate induces AmpC; hides ESBL Dr.T.V.Rao MD 52 •Best advice is to do synergy test (NOT SCREEN) with 4th gen ceph RISK FACTORS FOR ESBL INFECTION Length of hospital stay Severity of illness Time in the ICU Intubation and mechanical ventilation Urinary or arterial catheterization Previous exposure to antibiotics 53 Dr.T.V.Rao MD BACTERIA NOT TO TEST FOR ESBL’S Acinetobacter – Often S to clavulanate alone S. maltophilia Dr.T.V.Rao MD 54 – +vet result by inhibition of L-2 chromosomal lactamase, ubiquitous in the species ESBL REPORTING RULE The rule (CLSI =NCCLS) M100-S15)… • “Strains of Klebsiella spp. E. coli, and Proteus mirabilis that produce ESBLs may be clinically resistant to therapy with penicillin's, cephalosporins, or aztreonam, despite apparent in vitro susceptibility to some of these agents.” The message… • Report “confirmed” ESBL-producing strains as R to all Dr.T.V.Rao MD 55 penicillin's, cephalosporins, and aztreonam 55 WILL CLSI CONFIRMATORY TEST DETECT ALL ESBL-PRODUCING GNB? No - some isolates have ESBLs plus other resistance mechanisms that mask ESBL detection in the confirmatory test, e.g., • > 1 ESBL • ESBL + AmpC • ESBL + porin mutation Dr.T.V.Rao MD 56 ESBLs occur in species other than E. coli, Klebsiella spp., and Proteus mirabilis which CLSI does not currently address 56 ESBL DETECTION: AUTOMATED SYSTEMS (AS) Dr.T.V.Rao MD 57 144 putative of ESBL producers ESBL detection: •AS: Microscan, Vitek2, Phoenix •Phenotypic tests: Etest, DDS •Molecular tests: PCR, IsoElectric Focusing (IEF) Molecular identification: the reference method THE RESISTANCE BECOMING COMPLEX Beta-lactamases are getting more complex Full I/D needs complex molecular methods Much can be inferred from simple tests. Needs I/D Knowledge of what’s unusual Dr.T.V.Rao MD 58 Testing wide panels of antibiotics; synergy tests ANTIBIOTIC POLICY CHANGES PRACTISED Nitrofurantion substituted for quinolones in UTIs Imipenem substituted for quinolones in serious sepsis Ertapenem introduced for ESBL sepsis Gentamicin substituted for cephalosporins in surgical prophylaxis Dr.T.V.Rao MD 59 Return to amoxycillin in respiratory tract infections MICROBIOLOGY LABORATORIES AND ESBL’S Dr.T.V.Rao MD 60 Unfortunately, many clinical laboratories lack of understanding regarding ESBLs and Ampc ß-lactamase and their detection .This has been documented in a study in Connecticut USA, where it was found that 21% of laboratories failed to detect extended –spectrum cephalosporins and Aztreonam in ESBLs and Ampc. The true prevalence of ESBLs is not known and is probably underestimated because of difficulties encounter in their detection. However, it is clear that ESBLs –producing organisms are distributed worldwide and their prevalence is increasing. Dr.T.V.Rao MD 61 HAND WASHING STILL CAN REDUCE THE ESBL SPREAD The programme created by Dr.T.V.Rao MD for basic understanding by Medical Microbiologists in the Developing World Email Dr.T.V.Rao MD 62 doctortvrao@gmail.com