Assessment of perioperative hemodynamics
advertisement
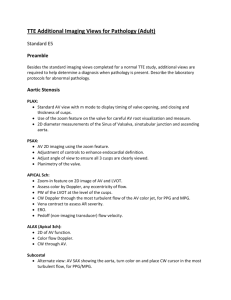
Assessment of perioperative hemodynamics S.Zahra Ojaghi Haghighi .MD, FACC Hemodynamic Data Obtainable with 2-D Doppler Echocardiography Volumetric measurement Pressure gradients Valve area Intracardiac and pulmonary artery pressures Ventricular dp/dt Assessment for Accurate Doppler Stroke Volume Calculations Blood flow is laminar with a spatially flat flow velocity profile. Measurements of the velocity-time integral and cross-sectional area(i.e,diameter) are made at the same anatomic location. The velocity-time integral measurement represents the average velocity-time integral(several measurements shouId be averaged for a patients in normal sinus rhythm,whereas 8 to 10 should be averaged for a patient in atrial fibrillation. The velocity- time integral is measured with doppler beam parallel to blood flow Calculation of Cardiac Output Usually measured at LVOT or aortic valve in the absence of AI. Correlate well with thermodilution. Doppler TEE has been used for continuous measurement of CO CO=SV*HR SV=CSA*VTI CSA=0.785*D(LVOT)*D(LVOT) Method LVOT(probe in the stomach,turned leftward,in the flexed position): 1-Parallel pulse Doppler of LVOT 2-Diameter obtained from either the stomach or the midesophageal 120degree view RVOT by pulse wave Pulmonary artery by pulse wave Aortic valve by continuous wave(cross-setional area of the aortic valve during mid systole) Mitral valve(CSA=0.785*D1*D2) LVOT Stroke Volume Calculation Pulse wave SV in LVOT proximal to the AV(approximately 1cm) Determination of the LVOT VTI: Transgastric long axis view or deep transgastric long axis view Diameter of LVOT: midesophageal long-axis view of aortic valve(approximately 1 cm) SV=CSA*LVOT VTI Practical consideration For intraoperative TEE ,LVOT is the most reproducible. Accuracy is improved by assessing multiple Doppler flow profiles,typically 3-5 for a regular rhythm and 10 for an irregular rhythm. Pulmonary –Systemic Flow Ratio(QP/QS) Indicates: Magnitude of a shunt(ASD,VSD, PDA) Timing of surgery Method Systemic SV(at LVOT or AV) Pulmonic SV(at PA or RVOT) Qp/Qs=(PA SV * HR) / (LVOT SV * HR) QP/Qs=PA SV / LVOT SV Doppler Measurement of Regurgitant Volume and Fraction Volumetric Method Proximal Convergence Method Assessment of Mitral Regurgitation by Volumetric Method RVmv=SV mvi – SV lvot RVmv(%)=(RVmv/SVmvi)*100% Perform infrequently during TEE due to time and possible error in SVmvi Assessment of Mitral Regurgitation by Proximal Convergence Method(PISA) PISA flow=MR flow 2* 3.14 * r2 * PISA velocity=EROA * MRv 6.28 * r2 * Aliasing velocity=EROA * MRv EROA=PISA flow rate/Regurgitant velocity EROA=(6.28 * r2 *Aliasing velocity)/MRv RV=EROA * VTI(reg jet)= (6.28 * r2 *Aliasing velocity * VTIreg jet)/MRv Method Color flow imaging of PISA from MR PISA radius Aliasing velocity Continuous Dopplerof MR jet to measure peak velocity and VTI of MR Simplified proximal convergence method Based on the assumption: MR velocity =5 m/s Aliasing velocity is set at 40 cm/s EROA=r2/2 Doppler Measurments of Pressure Gradients Bernoulli euation: dP= 4(V2-V1)2 dP=4(V2)2 Doppler Determination of Valve Area Continuity equation: SV1=SV2 CSA1 * VTI1=CSA2 * VTI2 CSA2=CSA1 * (VTI1/VTI2) Doppler Determination of Valve Area Flow Convergence Method: CSA=PISA flow/peak velocity CSA= (6.28 * r2 * Aliasing velocity/VMS) Pressure Half-time Defined as the time required for the peak pressure gradient to decline by 50% MVA(cm2)=220/PHT PHT(msec)=0.29 * DT(msec) AI severity and acute AI(<250msec) Intracardiac Pressure RVSP=4(VTR)2+RAP RVSP=SBP - 4(Vvsd)2 MPAP=4(Vearly PI)2 + RAP PADP=4(V late PI)2 +RAP LAP=SBP – 4(VMR)2 LVEDP=DBP – 4(Vend AI)2 PVR PVR=TRV / VTI RVOT* 10 + 0.16 TRV/VTI RVOT <0.2 = low PVR LVEDP PVa duration>MVA duration PVa >35CM/S Mean LAP=35-0.39 * (systolic fraction) DTof MV Systolic fraction of PV E/Em >15 ,E/Vp>2.6 LAP=(1.24 * E/Em) +1.9 PAWP PAWP=5.27 * (E/Vp) + 4.6 PAWP=1000 / (2 * IVRT)+Vp Estimation of RAP Doppler Measurement of dp/dt Calculated from time interval between 1m/s and 3m/s on MR Doppler velocity using simplified Bernoulli equation to calculate the LA-LV pressure gradients. LVdp/dt=32mmHg/dt LV dp/dt Normal >=1200mmHg/sec Reduced LV dysfunction<1000mmHg/sec Positioning of Intravascular Devices Intra-aortic Balloon Pump LV assist device RV assist Device(to avoid impingement on the tricuspid valve LV Vent(to drain excess ventricular volume on bypass. Assessment of preload(LV volume) Doppler estimation of LA pressure 1-SBP-MRgradient=LA pressure 2- systolic fraction in PVinflow 3-TDI(1.24*E/E1)+1.9 2-D measurement ofLV cross-sectional area