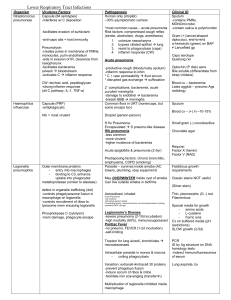
Respiratory tract infection
advertisement

Dr A.J.France RESPIRATORY TRACT INFECTION © A.J.France 2010 Objectives Define the range of conditions Recognise the common clinical presentations Understand the significance of pre-existing respiratory disease Look at the different features seen in immuno-compromised patients © A.J.France 2010 Range of conditions – Upper tract Common cold - coryza Sore throat - Pharyngitis Sinusitis Epiglottitis © A.J.France 2010 Range of conditions – Lower Acute bronchitis Acute exacerbation of chronic bronchitis Pneumonia Influenza © A.J.France 2010 Vocal cords – the dividing line Upper Resp Tract Lower Resp Tract Air conditioning Gas exchange Filtration Usually sterile Commensal organisms Temperature regulation Shared with Gastro – Intestinal tract © A.J.France 2010 Common cold - coryza Acute viral infection of the nasal passages Often accompanied by sore throat Sometimes a mild fever Spread by droplets and fomites Complications can include Sinusitis Acute bronchitis – see later © A.J.France 2010 Treatment for coryza © A.J.France 2010 Acute sinusitis Preceded by a common cold Purulent nasal discharge Treatment…. © A.J.France 2010 Special conditions Acute tonsillitis and quinsy – go to ENT lecture Diphtheria Life threatening due to toxin production Characteristic pseudo-membrane Not seen in UK due to vaccination Acute epiglottitis in children Life threatening due to obstruction © A.J.France 2010 Acute bronchitis The cold which goes to the chest Preceded by common cold Clinical features Productive cough Fever – minority of cases Normal chest examination Normal chest X-ray May have a transient wheeze © A.J.France 2010 Acute bronchitis -Treatment Antibiotics are NOT indicated Unless they have underlying chronic lung disease. © A.J.France 2010 Acute exacerbation of chronic bronchitis Remember – pre-existing lung disease with excess sputum and broncho-constriction. Clinical features Usually preceded by upper resp tract infection Worsening of sputum production which is now purulent More wheezy Breathless © A.J.France 2010 Acute exacerbation of chronic bronchitis On examination Breathless Wheeze Coarse crackles May be cyanosed In advanced disease – ankle oedema © A.J.France 2010 Acute exacerbation of chronic bronchitis Management in primary care Antibiotic. e.g. doxycycline or amoxicillin Bronchodilator inhalers Short course of steroids in some cases Refer to hospital if Evidence of respiratory failure Not coping at home © A.J.France 2010 Acute exacerbation of chronic bronchitis Management in hospital – same as before AND Measure arterial blood gases CXR to look for other diseases Give oxygen if has respiratory failure © A.J.France 2010 Right upper lobe Lobar pneumonia Pneumonia: Introduction Significant risk of fatal outcome 5-10% mortality from pneumococcal pneumonia 30% if bacteraemic 2600 deaths from pneumococcal pneumonia in UK every year © A.J.France 2010 Middle lobe. Lobar pneumonia Lobar pneumonia Normal Red hepatisation Lobar pneumonia Lung biopsy - autopsy Symptoms of pneumonia Malaise Cough Anorexia Pleurisy Sweats Haemoptysis Rigors Dyspnoea Myalgia Preceding URTI Arthralgia Abdominal pain Headache Diarrhoea Confusion © A.J.France 2010 Right lower lobe pneumonia - abdominal pain ? Pneumonia Signs Investigations Fever Blood culture Rigors Serology Herpes labialis Tachypnoea Arterial gases Crackles Full blood count Rub Urea Cyanosis Liver function Hypotension Chest X-ray © A.J.France 2010 Herpes simplex stomatitis Cyanosis CURB 65 severity score for pneumonia C New onset of confusion U Urea >7 R Respiratory rate >30/min B Blood pressure Systolic <90 OR Diastolic <61 65 age 65 years or older Score 1 point for each of above © A.J.France 2010 Pneumonia. Other severity markers Temperature < 35 or > 40 Cyanosis PaO2 < 8 kPa WBC < 4 or > 30 Multi-lobar involvement © A.J.France 2010 Pathogens in pneumonia Strep pneumoniae (pneumococcus) H. influenzae Mycoplasma pneumoniae Influenza Chicken pox – in adult smokers Legionella Coxiella burnetti Chlamydia psittaci © A.J.France 2010 Community acquired pneumonia: Management Antibiotics Amoxicillin + Doxycycline (see “antibiotic man” for details) Oxygen Maintain SaO2 94-98 % Fluids Bed rest No smoking © A.J.France 2010 Complications of pneumonia Respiratory failure Pleural effusion Empyema Death © A.J.France 2010 Empyema © A.J.France 2010 Empyema © A.J.France 2010 Special cases of pneumonia Hospital acquired Need extended gram negative cover Aspiration pneumonia Need anaerobic cover Legionella Chest symptoms may be absent GI disturbance is common © A.J.France 2010 History taking in pneumonia Cough Foreign travel Breathless Pets, including birds Chest pain Contact history Fever Other medical conditions Pre-existing chest disease Smoking history Lifestyle Prescribed drugs © A.J.France 2010 Prevention of pneumonia Influenza and pneumococcal vaccines Over 65 Chronic chest or cardiac disease Diabetes Immunocompromised e.g. splenectomy Influenza vaccine Health care workers © A.J.France 2010 Coffee break © A.J.France 2010