Document
advertisement

MUMPS,
DIPHTERIA,
TETANUS AND
PERTUSIS
Prof. Dr. Ayça
VİTRİNEL
MUMPS
Mumps virus RNA virus of the genus
paramyxovirus in the family paramixoviridae which also includes parainfluenza
viruses.
Spread from human reservoir by direct
contact, airborne droplets fomites
contaminated by saliva and possibly urine.
Peak age: 5-9 yr (before vaccinatum)
MUMPS
Virus has been isolated from as long as 6
days up to 9 days after appereance of
salivary gland swelling.
Isolated from urine from the 1st –14th day
after the onset of salivary gland swelling .
Transmission doesn’t seen to occur more
than 24 hr before the appereance of the
swelling or later than 3 days after it has
subsided.
MUMPS
Clinical Manifestations:
Incubation period 14-24 days
Prodrome : rare
Salivary glands: Pain and swelling in one
/both parotid glands
Swollen tissues push the ear lobe upward
and outward
MUMPS
Angle of the mandible is no longer visible
Swelling subsides within 3-7 days
Swollen area is tender and painful pain being
elicited especially by tasting sour liquids such as
lemon juice or vinegar
Redness and swelling about the opening of the
Stenon duct are common
Edema over the manibrium and upper chest wall
may occur lymphatic obstruction.
MUMPS
Swelling of submandibular glands occur
frequently and usually accompany the
parotid gland.
Least commonly the sublingual glands are
infected.
MUMPS
Diagnosis:
Clinical symptoms
Physical appereance
Laboratory : leukopenia (lymphocytosis)
elevations of serum amylase
Serology: IgM (in the first days) and IgG
Culture: saliva, CSF, blood, urine.
MUMPS
Treatment: no spesific antiviral treatment
Supportive
Complications:
Meningoencephalomyelitis: most frequently
complication. Male/female: 3/1
Primary infection of nerves at the same time or
before primer parotitis
Postinfectious encephalitis with demyelination
follows parotitis by an avarage of 10 days
MUMPS
Orchitis and epididymitis : adolescent and adults.
Follows parotitis within 8 days.
Oophoritis
Pancreatitis
Thyroiditis
Myocarditis
Deafness
Ocular complication
Arthritis
Prevention: mumps vaccine.
TETANUS
Acute spastic paralytic illness caused by
tetanus toxin (tetanospasmin) a neurotoxin
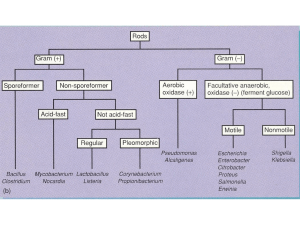
C.tetani Gr (+), spore forming, obligate
anaerobe. Natural habitat is soil, dust,
alimentary tracts of various animals
drumstic/tennis racket appereance microscopically.
TETANUS
1) Neonatal
2) Nonneonatal travmatic injury,
penetrating injury infected by a dirty object
use of contaminated suture material
Tetanus toxin binds at the neuromusculer
junction endocytosed by the motor
nerve axonal transport cytoplasm of
motor neuron prevents neurotransmitter
release
TETANUS
Blocks the normal inhibition of antagonistic muscles {basis of voluntary coordinated
movement} : affected muscles sustain
maximal contraction.
Clinical manifestations:
1) Localized
2) generalized: more common
TETANUS
Incubation period: 2-14 days
Trismus (masseter muscle spasm: lockjaw)
is presenting symptom
Headache, restlessness, irritability
stiffness, difficulty chewing, disphagia,
sardonic smile
Opistotonos : arched posture, neck muscle
spasm
Laringeal and respiratory muscle spasm :
airway obstruction
TETANUS
Patient remains conscious (tetanus toxin
doesn’t affect sensory nerves or cortical
function)
Smallest disturbance by slight sound, touch
: trigger a tetanic spasm
Dysuria, urinary retention, forced
defecation
Fever
TETANUS
Tachycardia, arythmics
Labile hypertension
Tetanic paralysis more severe in the 1st
week stabilizes in the 2nd week
Localized: painful spasm of muscles
adjacent to the wound site
TETANUS
Cephalic tetanus: Rare form of localized
tetanus involving the bulbar musculature
that occurs with wound or foreign bodies
in the head, nostrils or face.
Association with chronic otitis media.
Retracted eyelids + trismus + risus sardonicus + spastic paralysis of tongue and
pharyngeal musculature.
TETANUS
Neonatal tetanus: 3-12 days after birth
Difficulty in feeding
Paralysis or diminished movement
Stiffness to the touch
Diagnosis:
Clinically
CSF: NORMAL
TETANUS
Differential diagnosis: acute encephalitis
Rabies: CSF pleocytosis, hydrophobia
Strychnine poisoning
Hypocalsemia
Retropharengeal, dental abscess: trismus
TETANUS
Treatment: eradication of C. tetani
Neutralization of all accessible tetanus
toxin
Control of seizure
Supportive care
Prevention of recurrences
TIG (longer half life): Neutralizes the toxin
in the circulation before binding [30006000 U IM recommended ]
TETANUS
TAT: bovine derived 50.000 – 100.000 U
½ IM + ½ IV risk of serum sickness.
IVIG: Contains 4-90 U/ml TIG optimal
dosage is not known
Antibiotics: Pen G : 100.000 U/kg/ 24 hr :
4-6 hr intervals 10-14 days
Metronidazole: 500 mg of 8 hr equally
effective
Erythromycin and tetracycline are
alternative for penicillin allergic patients.
TETANUS
Muscle relexants: diazepam: relexation and
seizure control [0,1-0,2 mg/kg every 3-6 hr
IV: 2-6 weeks] { 2yr ; 8mg/kg/day }
Baclofen : only in intensive care unit
Neromuscular blocking agents M.V.
Phenobarbital and morphine may also be
used as an adjunctive therapy
TETANUS
Prognosis: recovery in tetanus occurs
through regeneration of synapses, within
the spinal cord and restoration of muscle
relexation . Episode of tetanus doesn’t
result in the production of toxin
neutralizing Abs : active immunization
with tetanus toxoid at discharge
TETANUS
Favorable prognosis: long incubation
period, absence of fever, localized disease
Prevention: active immunization, maternal
immunization with at least 2 doses of
tetanus toxoid, tetanus prophylaxis in
wound management
Clean minor
wound
Other
wounds
Prior tetanus
doses
Td
TIG
Td
TIG
Uncertain or
3
Yes
No
Yes
Yes
Three or
more
No
No
No
No
Yes if 10 yr
since last
dose
Yes if 5 yr
since last
dose
DIPHTERIA
Acute toxicoinfection caused by Corynebacterium diphteriae
Gr (+) bacilli, aerobic
Three biotypes mitis, gravis-least, intermediusmost common
Spread by airborne respiratory droplets , direct
contact with respiratory droplets, direct contact
with respiratory secretions of symp individuals.
Exudate from infected skin lesions
Asymtomatic respiratory tract carriers are
important in transmission.
DIPHTERIA
Entry of C. Diphtheriae in nose/mouth
localized on the mucosal surface of URT toxin
is adsorbed to cell membrane tissue necrosis
patchy exudate initially be removed
As the toxin production increases the area of
infection widens and deepens and a fibrinous
exudate develops tough adherent pseudomembrane is formed that varies from gray to
black attemps to remove it are followed by
bleeding.
DIPHTERIA
Edema of the soft tissues bull neck
appereance
Clinical manifestations: depend on the site
of infection
Incubation period: 1-6 days
Nasal diphteria: mild rhinorrhea nasal
discharge serosaguineous mucopurulent
excoriates the nares, upper lip
DIPHTERIA
White membrane on the nasal septum
Most often in infants
Slow absorbtion of toxin lack of
systemic symptoms
Tonsillar and/or pharyngeal diphteria: most
common site of disease
Anorexia, malaise, low grade fever, pharangitis [1-2 days] thin-gray membrane
DIPHTERIA
adherent membrane may spread to cover
the tonsils and pharyngeal wall may
progress [bleeding] in to the larynx and
trachea
Cervical lymphadenitis : bull neck appereance
Respiratory and circulatory collaps may
occur
Palatal paralysis may occur
Stuppor, coma, death : wihin 7-10 days
DIPHTERIA
Laryngeal diphteria: represents a downward
extension of the membrane for the pharynx
Occasionally only laryngeal involvement is
present
Noisy breathing
Progresive stridor, hoarseness
Suprasternal, subcostal, supraclavicular
retractions
DIPHTERIA
Cutaneous diphteria: an ulcer with a sharpy
defined border ,important source of person
to person transmission
Conjunctival lesions: red, edematous,
membranaeous , corneal erosion
Aural diphteria: otitis externa with a
persistenly purulent and frequently faul
smelling discharge
DIPHTERIA
Diagnosis: isolation of C. diphteria (
Loeffler, tellurite and blood agar)
WBC N/
Anemia; result of rapid hemolysis
Toxigenicity by inoculating 2 guinea pigs
ID suspension of microorganism (
antitoxin/no antitoxin) 24 hr inflamatory
lesion , 72 hr necrotic lesion
DIPHTERIA
Complications: Myocarditis: 2nd week (1-6 wk)
ST-T changes 1st degree heart block, hearth
failure, myocardial enzymes
Neurologic complications: Bilateral, usually
resolve competely. Paralysis of the soft palate
and pharengeal muscles (1-3 wk ). Ocular muscle
and ciliar paralysis (5th wk). Paralysis of
diaphragm (5-7 wk). Paralysis of the limbs with
loss of deep tendon reflexes (2-7 wk)
Elevation of CSF protein, pleocytosis
Hypotension, cardiac failure, gastritis, hepatitis,
nephritis
DIPHTERIA
Prevention: Immunization
Contacts: Isolation of patient; three consecutive
(-) cultures. Cultures schould be taken from close
contacts, observed for 7 days if C. diphteria is
recovered treatment schould be instituted
Asymptomatic immune close contacts: receive a
booster of DT, Td, if they haven’t received
booster within 5 yr.
DIPHTERIA
Asymptomatic close contact is not
immunized or the immunization status is
unknown. He/she should be closely
observed and started erythromicin (7 days)
or benzathine pen G : culture should be
obtained before and after treatment ,active
immunization should be given.
DIPHTERIA
Treatment : Antitoxin must be administired
as early as posible by IV route and in a
dose sufficient to neutralize all free toxins
Desensitization must be done
20.000-40.000 U for pharyngeal/laryngeal
40.000-60.000 U nasopharyngeal
80.000-100.000 U extensive disease
DIPHTERIA
Penicillin (procain 300.000/600.000 U IM)
erythromicin (40 mg/kg/day) 14 days
End point of therapy : three consecutive
negative culture
Bed rest 2-3 wk
Hydration
Laryngeal diphteria; tracheostomy
PERTUSIS = WHOOPING
COUGH
Acute respiratory infection
Bordetella pertusis (B. Parapertusis, B.
Bronchiseptica) Gr (-) cocobacils
Recovered best in Bordet Gengou media
(glyserin, patato, blood agar)
Humans are the only known host
Spread occurs by direct contact, by
respiratory droplets
PERTUSIS
Transplacental passage of maternal Ab
does not protect the NB
Severe neonatal pertusis can be acquired
from a mildly symptomatic mother.
Pathology: peribronchial lymphoid
hyperplasia necrotizing process
Bronchopneumonia develops with necrosis
and desquamation of superficial epithelium
of small bronchi.
PERTUSSIS
Bronchiolar obstruction and atelectasis
accumulation of mucus secretions
Bronchiectasis may develop
Microscobic or gross cerebral hemorrhages
may be seen, cortical atrophy has been
observed
Fatty infiltration of the liver
B. Pertussis produces many biologically
active factors that are responsible for
disease
PERTUSIS
Pertussis toxin, filamentous hemaglutinin etc
Clinical manifestations: inc period : 6-20 days
1) catarhal stage: 1-2 wk rhinorhea, conjuctival
injection, lacrimation, mild cough, low grade
fever
2) paroxysmal stage: 2-4 wk
Repetitive series of 5-10 forceful cough during a
single expiration sudden massive inspiratory
effort.
PERTUSIS
Prominent during attack:
Facial redness/cyanosis
Bulging eyes
Protrusion of tongue
Lacrimation, salivation
Distention of neck veins
PERTUSIS
Attacks may be trigerred : yawning,
sneezing, eating, drinking
Petechial/ conjuctival hemorrhages may be
noted on the head and neck
Diagnosis: cough more than 2 wk duration
with posttussive emesis is an important
diagnostic clue.
PERTUSIS
Leukocytosis (20.000-50.000 /mm³)
Absolute lymphocytosis
Chest roentgen: perihilar infiltrates,
atelectasis, emphysema
Spesific diagnosis: recovery of the
organism nasopharingeal swabs
ELISA (IgM, IgG, IgA)
PCR
PERTUSIS
Complications:
1) respiratory: pneumonia, atelectasis,
emphysema, pneumothorax, bronchiectasis, otitis
media, epistaxis
2) pressure: intracranial hemmorhagea,
subconjuctival hemmorhagea, epistaxis, rupture
of diaphragma, umbical hernia, inguinal hernia,
rectal prolapsus
3) other: convulsions, dehydration, nutritional dis
PERTUSIS
Prevention: vaccination
Erythromycin effective in preventing
pertusis.
Close contacts of less than 7 yr of age who
have been immunized previously
booster dose, erythromicin 14 days
7yr , immunized erthromycin 14 days
Treatment: erythromycin 50 mg/kg/day
(d4) 14 day