Document
advertisement

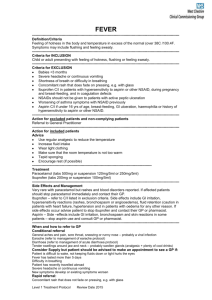
Pediatric Pain Management Assessment & Interventions 4/10/2015 1 Introduction Definition of pain: an unpleasant sensory and emotional experience associated with actual or potential tissue damage Always subjective and is learned through experiences R/T injury in early life Circumcision study Can be assessed by verbal, behavioral and physiological indicators 4/10/2015 2 Need to differentiate “PAIN” from “DISTRESS” Pain related to fear and anxiety Often exhibited by children Highly correlated with the degree of pain in children May reflect other emotional reactions 4/10/2015 3 Neonatal Pain Perception Peripheral and central structures required for pain reception and function in 1st & 2nd trimesters EEG patterns/ cortical evoked potentials Cerebral glucose utilization Newborn infants have well-developed H-P axis Pain impulses in newborns conducted by unmyelinated C-type fibers Newborns lack descending inhibitory neuro transmitters RESULT: Infants cannot modulate their pain well. 4/10/2015 4 Developmental Reactions to Pain Infants Rely on caregivers to notice pain Give behavioral signs that they are hurting Change in activity—restlessness, clinging or whining, appetite Physiologic indicators—tachycardia, tachypnea, BP 4/10/2015 5 Developmental Reactions to Pain Toddlers Have poor body boundaries Intrusive experiences, even if not painful, are anxiety producing Often react intensely and physically resist Biting, kicking, hitting, running away Help parents understand reactions and avoid punishment Use play activities & distraction Use bandages but be aware of anxiety when they are removed 4/10/2015 6 Developmental Reactions to Pain Preschoolers (3-6 yrs) Need reassurance that pain is not a punishment Magical thinking & egocentric 4/10/2015 Exaggerated ideas about illness that are worse than reality Can lead to feelings of shame guilt, fear May view illness as punishment for something Resist during painful procedures: fear of mutilation and bodily injury Concrete thinkers; may misinterpret words Allow to express feelings – provide play opportunities Give simple explanations: short,simple, clear 7 Developmental Reactions to Pain Preschoolers (3-6 yrs) cont’d 4/10/2015 Praise for good behavior Cannot always indicate source or location of pain Believe in the magical nature of pain—allows for effectiveness of some therapies e.g. kiss, bandaid. It works because they believe in it. 8 Developmental Reactions to Pain School Age (6-12 years) Able to locate pain in terms of body parts Main concern: body integrity; < concern for pain than disability or death Feel that injury is r/t guilt (so they deserve pain) Want factual info & reasons for things Adolescent (13-19 years) 4/10/2015 Afraid of looking like a baby Often hesitant to express feelings of pain Main concern: body image Fear death as well 9 Pediatric Pain Scales http://www.med.umich.edu/yourchild/topics/pai n.htm Excellent link with LOTS of great information on pediatric pain management from the University of Michigan. 4/10/2015 10 Neonatal Infant Pain Scale NIPS used at BroMenn for infants 1-10 scale Pain score of > 6 is considered reflective of pain Another resource that describes this scale from Cincinnati Children’s Hospital 4/10/2015 11 Non-Pharmacological Pain Management Infants Tactile: touching, stroking, patting, swaddling Motion: rocking, bouncing Comfort: sucking/ pacifier, sucrose— 24% sucrose solution just before procedure Environment: 4/10/2015 quiet, soft music, low lights 12 Non-Pharmacological Pain Management Toddlers & Preschoolers Preparation: simple, sensory, developmentally appropriate Caregiver presence Distraction: bubbles, glitter wands, books, rain stick Praise: offered freely, for trying (not for succeeding) Simple choices “One voice”—allows distraction without over stimulating 4/10/2015 13 Non-Pharmacological Pain Management School Age Preparation/ rehearsal—have “practice kits” with real equipment to feel and get familiar with procedure ahead of time. Distraction Relaxation techniques 4/10/2015 14 Non-Pharmacological Pain Management Adolescents Preparation—allow adequate time Distraction Relaxation techniques Often need lots of reassurance and clarification of the procedure. 4/10/2015 15 EMLA/LMX-4 Cream Dosage: 0-3months: 1 gram maximum, 10 sq.cm surface area, 1 hour duration. 3-12 months, > 5 kg: 2 grams max, 20 sq. cm surface area, 4 hour duration. 1-6 years, > 10 kg: 10 grams max., 100 sq.cm. Surface area, 4 hour duration. 7-12 years, >20 kg: 20 grams max., 200 sq. cm. Surface area, 4 hour duration. 4/10/2015 16 EMLA/LMX-4 Cream--techniques Individuals with darker pigmented skin or who are dehydrated may require longer application time. Longer application required on thick skin Removal of stratum corneum layer of skin may facilitate absorption Although maximum analgesia occurs after 1 hour, shorter times partially effective Application of warm compresses will lessen blanching and bring the veins back to visibility. 4/10/2015 17 Pediatric Doses for Acetominophen and Ibuprofen Accepted doses for Acetominophen 10-mg/kg/dose is considered in neonates 15-mg/kg/dose is WNL in older children If child weighs 12 lbs, how much would you tell mom to give per dose? Accepted doses for Ibuprofen 10-mg/kg/dose is considered WNL. Some pediatricians insist the child must be able to eat or drink to avoid irritation to the stomach. If child weighs 22 lbs, how much would you tell mom to give per dose? 4/10/2015 18 How Acetaminophen is packaged Infant Drops= 100mg/ml NO LONGER AVAILABLE Elixir= 160mg/5ml most common Tylenol Chewables= 80mg/tab Tylenol Junior Strength Chewable or Gelcap= 160mg/tab Give Acetaminophen every 3-4 hours prn. 4/10/2015 19 How Ibuprofen is packaged Pediatric Drops= 100mg/2.5ml Children’s Suspension= 100mg/5ml Children’s Chewables= 100mg/tablet Give Ibuprofen every 6-8 hours, not to exceed 4 doses/day Acetaminophen and Ibuprofen may be safely given alternately to enhance antipyretic effects of combined meds. 4/10/2015 20 A final thought Use a balanced approach to pain management Incorporate nonpharmacologic and pharmacologic therapy Try multiple analgesics which work by different mechanisms. Use developmentally appropriate communication & methods for providing comfort Be aware of signs of pain at different ages 4/10/2015 21