Types of Pesticides - Pesticide Health Effects Medical Education
advertisement

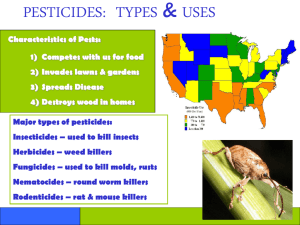
Pesticide Basics Uses, Exposures, Types and Acute Effects Did you know? 5 million at risk population (U.S. EPA, 1992) 250-500 physician-diagnosed cases occur per 100,000 agricultural workers (Blondell, 1997). Migrant and seasonal farmworkers are especially at high risk 84% of American households used pesticides, most commonly insecticides (Whitmore et al, 1992) Homeowners use 5-10 lbs/acre/yr on their lawns and gardens, many x greater than farmers apply to corn and soybean fields (Robinson et al, 1994). Did you know? Non -agricultural pesticide exposure as disinfectants widespread: (e.g., pine oil cleaners, bathroom cleaning products, and cleaning materials for swimming pools). Non-Ag Sector a concern = pest control, nurseries, greenhouses, and landscaping. The medical profession uses disinfectants to sanitize and sterilize surfaces and instruments. Organophosphate and pyrethroid insecticides most implicated for poisonings. Water chlorination is one of the largest (by tonnage) uses of pesticides. Where Are Pesticides Used? Forests to control insects and under-story vegetation; Landscapes, parks, and recreational areas to control weeds, insects, and disease pests; Rights-of-way along railroads and under electric wires to control vegetation; Houses, schools, and commercial and office buildings to control insects, rodents, and fungi; Boat hulls to control fouling organisms; Where Are Pesticides Used? Aquatic sites to control mosquitoes and weeds Wood products to control wood-destroying organisms Food preparation areas to control insects and rodents Human skin to kill or repel insects Household pets to control fleas and ticks Livestock to control insects and other pests. Non Occupational Pesticide Encounters • • • • • • • • Accidental or intentional ingestion Food and water residues Contaminated clothing Treated wood/structures Residues on animals/carpets Garden residues Termite control Hazardous waste sites/spills Agriculture Pesticide Applications Boom sprayer Aerial Enclosed cab Air blast sprayer Backpack wand Agriculture Jobs Orchard thinner Flagger Mixer loader Picker Professions Exposed to Pesticides • • • • • • • • • • • • Aerial equipment maintenance Agronomists Building maintenance work Emergency responders Entomologists Firefighters Forestry workers Formulating end product Greenhouse- nursery workers Hazardous waste workers Landscapers Livestock dippers and veterinarians • • • • • • • • • • • • • Marina workers Medical personnel Park workers Plant pathologists Research chemistry Sewer work Storage/warehouse work Structural application Transporting pesticides Treating contaminated workers Vector control workers Wood treatment workers Work on highway or railroad rights of way Key Household Safety Points “ Partly Trained Gorillas Always Run Down Streets Doing Cartwheels” 1. 2. 3. 4. 5. 6. 7. 8. 9. Proximity Take home Garden Animals Recycle Decant Storage Disposal Child play/daycare ROUTES OF EXPOSURE OP’s are readily absorbed: Across the SKIN with skin contact In the lungs with INHALATION of pesticide contaminated air/dust In the gut by INGESTION of pesticide residue on food/dirt/dust Source: EPA Protect Yourself from Pesticides-Guide of Agricultural Workers Risk Factors for Occupational Pesticide Exposures Concentration of commercial preparations > than diluted final product = greater risk AG workers highest exposure risk in mixing, loading, applying, and flagging. Source: H Murphy - Cambodia Occupational Risk Factors • Pregnant Women: 1st trimester • Field workers entering sprayed field before re-entry interval [REI] • Residuals on skin and clothes – How to remove PPE – How to clean PPE – Showering after use Evidence? Agriculture Risk Factors • Indonesia: – – – – Cocktail mixture of multiple products Spray frequency Skin contact > wet clothing Use of toxic products (1a/Ib, II) Source: H Murphy - Indonesia • Washington state: – – – – – Protective: Chemically resistant boots Protective: Full face respirators Risk: Mixing and loading pesticides Risk: Cleaning equipment Protective: Using a workplace locker for PPE Preventing Pesticide Illness Primary Non-chemical Alternatives Secondary Engineering Controls Tertiary It’s the law Personal Protective Equipment [PPE] Risk factors for pesticide exposures at home • • • • • • Migrant families > risk Children’s vulnerability Location near fields Take home pathway Pesticide storage and use in homes Multiple chemical sensitivities (MCS) Migrant Families • Living conditions: quality and location • Communication: language and literacy • Immigration status • Access to health care • Diet Unintentional (Accidental) • GI absorption from accidental ingestion = acute poisonings • Respiratory and dermal absorption from surrounding environment • Hand to mouth activity in children Occupational • Dermal is most important • Inhalation is a common pathway • Ingestion less common but can occur if not use gloves or poor hygiene Intentional (Suicide/Homicide/Abuse) • Ingestion is primary pathway • Inhalation is another pathway, although primary agents of abuse in this manner are nonpesticide chemicals (aromatic solvents). Agricultural vs. Non-Agricultural Cases of Poisonings 120 113 100 111 99 90 72 80 cases 68 62 75 73 60 58 40 20 0 Non Agricultural 1999 2000 Agricultural 2001 2002 2003 Source: 2004 Pesticide Incident Reporting and Tracking (PIRT) Annual Report Occupational versus Non-Occupational Cases of Pesticide Poisoning NonOccupational 48% Source: 2004 Pesticide Incident Reporting and Tracking (PIRT) Annual Report Occupational 52% Proportion of Poisonings Ranked 8th Cause of Poisonings = 102,754 cases in 2005 (4.2%) Children Adults Source: Watson WA. 2004 Annual Report of the American Association of Poison Control Centers Toxic Exposure Surveillance System US: Intentional vs. Accidental Accidental 84% Suicide 8% 6 suicide attempts used pesticides out of 196,164 WHO Sentinel Surveillance Country Time period Reporting sites Cases Circumstances identified Intentional Accidental Occupational INDIA 12 mo 10 1531 95% 89% 5% 6% NEPAL INDONESIA THAILAND MYANMAR PHILIPPINES 10 mo 12 mo 6 mo 6 mo 6 mo 38 8 9 8 5 327 208 130 126 256 99% 94% 98% 96% 93% 87% 86% 62% 43% 92% 8% 8% 8% 16% 1% 4% 0% 28% 37% 0% Pesticide ‘cide = to kill Fumigants Insecticides Types of Pesticides Herbicides Fungicides Disinfectants Rodenticides Pesticide Chemical Families -grouping based on similarities1. 2. 3. Similar chemically (similar structure) Attacks pests in a similar way (toxicity) Common treatment + antidote Organophosphate OP Organochlorine OC Carbamate C Chlorophenoxy Pyrethroid PY Paraquat Diquat Pesticide Sample Label Type of pesticide (used for?) Company name Brand name Common/generic name (active ingredient) Chemical family (? atropine under 1st aid) Signal word (hazard level) Pesticide Classification Table # Type 1. Insecticide Company Name Gowen Brand Name Common Name Supracide methidathion Chemical Family OP (Organophosphate) Signal Class DangerPoison Ib Exercise: Classifying Pesticides Pesticide Labels COMPANY BRAND COMMON TYPE FAMILY SIGNAL Who 1. Bayer Temik Aldicarb Insecticide Carbamate Danger-poison la 2. Verdicon Sevin Carbaryl Insecticide Carbamate Caution ll 3. UCP Alliance Thiodan Endosulfan Insecticide Organochlorine Warning ll 4. Bayer Guthion Azinophos methyl Insecticide Organophospate Danger-poison lb 5. Dow Dursban Chlorpyrifos Insecticide Organophospate Warning ll 6. Syngenta Gramoxone Paraquat Herbicide Paraquat Danger-poison ll 7. Helena Weed Rhap 2, 4-D Herbicide Chlorophenoxy Danger-poison ll 8. DuPont Asana Esfenverlate Insecticide Pyrethroid Warning lV 9. Bayer Captan Captan Fungicide Danger-poison II 10. Max Roundup Glyphosate Herbicide Caution U-IV 11. Dow Dithane Mancozeb Fungicide Caution U-IV Ziram Fungicide Danger III 12. Cerexagri-Nisso Ziram How toxic is it? Source: Richards, Kerry Penn State University Extension Service Source: Richards, Kerry Penn State University Extension Service LD50 Lethal dose = Amount of chemical it takes to kill 50% of an experimental population Source: Richards, Kerry Penn State University Extension Service * * DANGER/POISON = extremely toxic by ingestion DANGER = extremely toxic high potential for skin and eye irritation Adapted from Richards, Kerry Penn State University Extension Service Source: Richards, Kerry Penn State University Extension Service Insecticides • ChE Inhibitors: – Organophosphates – n-methyl carbamates • Pyrethroids – Pyrethrins (ocloresin extract of chrysanthemum) – Pyrethroids (the synthetic derivative) • • • • • • Organochlorines (e.g. DDT) DEET Boric Acid Fluorides Nicotine Arsenicals Herbicides • Chlorophenoxy herbicides (e.g. 2-4D) • Paraquat and diquat • Pentachlorophenol and dinitrocresol (wood preservatives) • Copper chromium arsenate ( decks, fences, and children’s wood playground sets – d/c 2003) Fungicides • • • • Hexachlorobenzene Thiram Maneb Methylmercury compounds Fumigants • • • • • • Cyanide 1, 3-dichloropropane Metam sodium Methyl bromide Naphthalene Phosphine gas (from aluminum phosphide) Rodenticides • Warfarin-related compounds: – – – – Warfarin Coumarins Brodifacoum Difenacoum (so-called “super warfarins”) • Others: – Thallium – Zinc phosphide – Sodium fluoroacetate Disinfectants • Agents used for sanitization and sterilization in the home and hospital • Registered as pesticides by the U.S. EPA • Examples include – – – – – – Alcohols Chlorhexidine Hypochlorites Iodines Phenols Pine oil Organophosphates: 30”-240 & Carbamates: 15”-30 General central nervous system • Fatigue • Dizziness • Headache • Tremors • Ataxia • Convulsions (uncommon w/carbamate) • LOC (uncommon w/carbamate) • Coma (uncommon w/carbamate) From muscle over stimulation: • Muscle weakness • Muscle cramps • Muscle fasciculations From gland over stimulation: • Salivary gland- excessive salivation • Sweat gland- excessive sweating • Lachrymal gland-excessive eye tearing From organ over-stimulation: • Eyes • Gastrointestinal • Pulmonary •Blurred vision (constricted pupils) • Stomach cramps • Nausea • Vomiting • Diarrhea • Chest tightness • Wheezing • Cough • Runny nose Pyrethroids Pyrethroids: are irritants to the eyes, skin and respiratory tract. The symptoms last from 1-2 hours. Systemic toxicity from inhalation or dermal absorption is low. Normal use: * * * * Paresthesias (cyno pyrethroids) Shortness of breath (wheezing) Mucous membrane irritation (throat nose) Skin itching If ingested: • • Loss of consciousness/coma Seizures (cyno-pyrethroids) High doses: • • • • • Vomiting Diarrhea Excessive saliva Muscle fasciculation Ataxia • Irritability: to sound ~ touch Cyno-pyrethroids: fenverlate, flucythrinate, fluvalinate cypermethrine, deltapermethrin, Organochlorines: 10 - 480 lipophylic The nerves stimulating glands are not affected so you will NOT see: • excessive salivation • excessive sweating • excessive eye tearing (or over-stimulation of small muscles like) • twitching eyelids CNS Effects • Muscle Weakness • Dizziness • Headache • Numbness • Nausea/vomiting • LOC • Seizures • Tremors • Ataxia • Anxiety/restlessness • Confusion Paraquat Paraquat is very toxic to the skin and mucous membranes. Particles are too large to get deep into the lungs*, but once in the blood it collects in the lungs. If ingested high case fatality rate. • Skin: • • • • dryness, cracks erythema blistering ulcerations • Nails: • • • discoloration splitting nails loss of nails • Respiratory tract: • • • cough nosebleeds sore throat • Eyes: • • conjunctivitis ulceration, scarring, blindness • Ingestion: • • lung fibrosis (stiff lungs) multi-system organ failure, specifically respiratory failure kidney failure • • DEET DIETHYLTOLUAMIDE • Few toxic cases - given the widespread use • Toxic if ingested • Children: toxic encephalopathy w/ heavy use on large surface area on kids (+ ETOH - isopropyl or ethyl) • Dermal problems: tingling, irritation, desquamination, contact dermatitis, exacerbate pre-existing skin dz • Kids: use 5-6.5% formulations Boric Acid Ants, Cockroaches in Residences “broiled lobster appearance” Boric Acid Respiratory tract irritant Moderate skin irritant Historic antibacterial: poisonings from burn compresses, diaper powder, irrigation solutions Targets: GI tract, skin, vasculature, brain Chronic ingestion more toxic than acute (13 ½ life) Absorption: via gut and abraded skin Fluorides • Transformed in stomach to corrosive hydrofluoric acid: thirst, nausea-vomiting, diarrhea, abdominal pain • Fluoride ion reduces extra-cellular fluid concentrations of Ca+ and Mg hypocalcemic tetany • Cardiac arrythmias- shock 2ndary to fluid/electrolyte imbalances, hypokalemia and the fluoride itself • CNS H.A. muscle weakness, stupor, seizures and coma Focus on OP’s Children at risk for neurodevelopmental problems Most commonly used insecticide in agriculture Common cause of poisoning Normal Electrical Nerve Impulse Transmission nerve cell After electrical nerve impulse transmission is completed, the body produces cholinesterase. Electrical nerve impulse coming from nerve cell stimulates the body to produce acetylcholine. Cholinesterase breaks up acetylcholine into acetate and choline. Acetylcholine acts as a bridge transmitting the electrical charge to the muscle cell. acetate choline Muscles and glands contract. Once acetylcholine is broken, it can no longer transmit electrical nerve impulses. Electrical nerve impulses stop and the muscles and glands are quiet muscle cell Organophosphate-Carbamate Disruption of Electrical Nerve Impulse Transmission Therapeutic Effect of Atropine nerve cell If an organophosphate (Op) or carbamate is present, they bind with cholinesterase. [This is an irreversible effect with an Op but not with a carbamate] Atropine relieves the over stimulation of the muscles and glands by reducing the amounts of acetylcholine. The effect only lasts 15 minutes. Therefore the dose must be repeated until the organophosphate binding effect has worn off. The bound cholinesterase cannot penetrate acetylcholine to break it up. The body continues to produce acetylcholine unimpeded. Electrical nerve impulse acetate This results in a build up of acetylcholine with continuous electrical nerve impulse transmission and over stimulation of muscle and glands. choline cholinesterase organophosphate atropine muscle cell Signs and Symptoms in Adults Exercise: Body Mapping Eye • Miosis • Blurring CNS • • • • • • • • • • Fatigue Dizziness Headache Tremors Ataxia Seizures LOC Coma Insomnia Mental Δ Lungs Tightness Wheezing Cough Rhinorrhea GI Abd. cramps Nausea Vomiting Diarrhea Glands Drooling Muscle Heart Weakness Cramps Tachy Fasciculations Sweating Brady Tearing BP ↓ BP Signs of Pesticide Poisoning in Children Lethargic sleepy Seizures Coma Can be confused with the flu