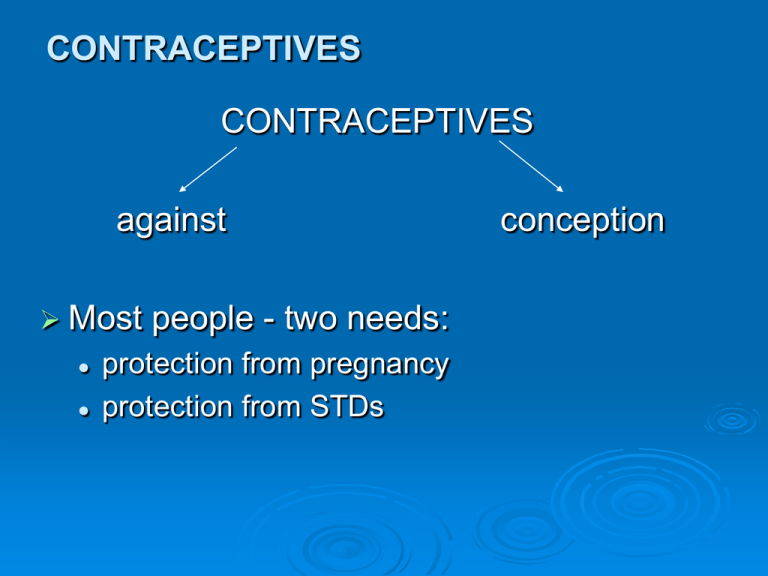
CONTRACEPTIVES
CONTRACEPTIVES
against
Most
people - two needs:
protection from pregnancy
protection from STDs
conception
CONTRACEPTIVES
Contraceptives can fail due to:
method failure (varying %)
user failure
Why?
embarrassment
inhibitions
not spontaneous
memory failure
mood
awkwardness
dulled sensation
alcohol, other drugs
CONTRACEPTIVES
Why? (Cont’d)
fear parents will find out
fear to go to the doctor
heat of the moment
ashamed to buy
expense
takes the danger out of love
embarrassed to ask male partners
lots of guys hate condoms
CONTRACEPTIVES
Before Judeo-Christian era, women used
different mixtures quite effectively.
Ex: camel or crocodile dung, herbal preparations
Knowledge gradually disappeared due to
religious restrictions. (Patriarchal societies)
Most common contraceptive around the world:
Second most common:
breastfeeding!
tubal ligation
Myths about contraception
CONTRACEPTIVES
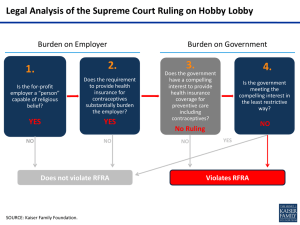
Research
and education hampered by
religious opposition in many countries:
influence on law
jail for contraception providers – Margaret
Sanger
Still an issue in some countries, including
some states in the USA
In Canada: Pierre Trudeau: the state has no
business in the bedrooms of the nation – led
to liberalized laws regarding sexual behaviour
(1969)
CONTRACEPTIVES
BARRIER
METHODS:
Male condom:
• latex (best) or intestinal tissue
of animals (mostly lambs),
lubricated or un
• better: polyurethane, thinner,
stronger, conduct heat but a bit
looser
• relatively cheap – depends on
frequency of use!
• protects against STDs (latex
only)
• no prescription or fittings
• easily available (in urban areas)
now internet
CONTRACEPTIVES
BARRIER
METHODS (Cont’d):
Male condom (Cont’d):
•
•
•
•
•
failure rate 10-12% due to user mistakes
many men dislike it, reduced sensation (?)
spontaneity
damaged by heat (pocket), fingernails
need to be used with other contraceptive methods
to prevent STDs
CONTRACEPTIVES
BARRIER METHODS (Cont’d):
Female condom:
• polyurethane, lubricated, two
rings, one over cervix, one
over vulva
• polyurethane more resistant
to tears and other damage
• female control
• expensive
• high failure rate (preliminary)
• spontaneity
• awkward
CONTRACEPTIVES
BARRIER METHODS (Cont’d):
Diaphragm: no longer available in NL
• rubber with ring
• covers cervix loosely but stays in place
if properly fitted
• used with contraceptive cream/jelly
• failure rate in US 18%, due to misuse,
lower in Europe and Latin America
• can be inserted 6 hrs. before, must be
left in 6 hrs. after
• can be left in place for repeated sex
• need Dr.’s fitting and prescription
• does not protect against STDs
CONTRACEPTIVES
BARRIER METHODS (Cont’d):
Diaphragm (Cont’d):
• must be with owner when needed
• failure due to arousal changes in vagina
(ballooning), large changes in weight, birth, etc.
need resizing
• cream or jelly can be irritating to women or partner
• not advisable during menstruation
• needs to be washed and dried thoroughly after
each use
• no harmful side effects
• inexpensive
CONTRACEPTIVES
BARRIER METHODS (Cont’d):
Cervical Cap: not available in NL
• similar but more difficult to
insert
• fits more snugly over cervix
• doctors in North America not
trained to fit it or instruct patient
• can be left in longer but risk of
TSS and infections
• high failure rate in the US
• no STD protection
CONTRACEPTIVES
BARRIER
METHODS (Cont’d):
Lea’s Shield (now there are different brand names)
• is a one-size-fits-all reusable vaginal barrier
contraceptive device. Approximately the size of a
diaphragm, it is composed entirely of medical
grade silicone rubber. The device is washable and
reusable.
• does not compare with any other mechanical
device on the level of form, volume or matter.
Unlike other barrier contraceptives, it does not
depend on vaginal dimensions or cervical size
which vary from woman to woman.
CONTRACEPTIVES
INTRAUTERINE
DEVICES
Different shapes, materials.
Inserted inside uterine cavity by physician.
Can work by preventing sperm from
swimming up or by preventing implantation.
Unknown.
Very old method.
Some brands caused PID (pelvic
inflammatory disease) leading to permanent
infertility, ectopic pregnancies and
hemorrhaging.
CONTRACEPTIVES
INTRAUTERINE
DEVICES (Cont’d):
Can perforate uterine wall.
If woman becomes pregnant, high risk of
miscarriage.
Periods heavier, cramping, bleeding between
periods.
No protection against STDs.
Can be expelled by uterine contractions.
Some women very happy with this method.
CONTRACEPTIVES
CHEMICAL CONTRACEPTIVES:
Spermicides:
• Chemical substances that kill sperm.
Ex: nonoxynol-9. Cream, jelly or foam.
• Irritation or allergic reaction.
• Also added to other contraceptives.
• By itself high failure rate
Sponge:
• Combination barrier and spermicide. 25% failure
rate.
• No prescription needed, intercourse can be
immediate or within 24 hrs.
• Increases rate of TSS and UTIs.
• Currently off market.
CONTRACEPTIVES
HORMONAL CONTRACEPTIVES:
Pill:
• Estrogen and progestin (synthetic progesterone)
• After period estrogen low, prompts FSH. Pill blocks
this by elevating estrogen. 95% effective. (ideal
users)
• Progestin helps by
inhibiting production of LH
thickening cervical mucus (sperm get stuck)
changing the endometrium so implantation is unlikely
• Different types of pill, see text.
• “Mini pill”: progestin only, less effective
CONTRACEPTIVES
HORMONAL
CONTRACEPTIVES:
Norplant: currently not available
•
•
•
•
•
•
•
Subcutaneous implants of silicone cylinders
Small surgical procedure (upper arm)
Contains progestin
Inhibits ovulation
Thickens vaginal mucus
Prevents thickening of endometrium
Removal is difficult (scar tissue grows around it)
same pros and cons as pill except forgetting, so
highest effectiveness.
CONTRACEPTIVES
HORMONAL CONTRACEPTIVES (Cont’d):
Depo-Provera:
• Injectable progesterone (medroxyprogesterone) prevents
ovulation and changes mucus
• Breast cancer risk
• Osteoporosis
• Irregular menstruation
• Amenorrhea
• Weight gain
• Headaches
• Anxiety
• Stomach pain, cramps
• Dizziness
• Weakness, fatigue
• Loss of libido
CONTRACEPTIVES
HORMONAL
CONTRACEPTIVES
(Cont’d):
Quarterly shots of estrogen and progestin
Lunelle, Cyclo-provera, Cyclofem
100% effective
Same pros and cons
Yasmin: ethinylestradiol + drospirenone (type
of progesterone) synthetic – recalled – unsafe
Patch: on fleshy body parts
CONTRACEPTIVES
Seasonale
taken continuously for 3 months
low dose estrogen and progestin
only 4 menstrual periods per year
what long-term consequences???
Plan B
emergency contraception
two progestin pills
within 24 hours of unprotected sex:
• 95% effective
the longer the interval, the lower the effectiveness
Plan B is now available prescription-free in most
provinces
alternative: two or more pills of any contraceptive pill
CONTRACEPTIVES
Drugs that interact with oral contraceptives
(partial list):
acetaminophen: pill lessens pain relief
alcohol: pill enhances alcohol effects
anticoagulants: pill decreases their effect
antidepressants: pill enhances their effect
barbiturates: interfere with pill effectiveness
penicillin: decrease pill effectiveness
tetracycline: ditto
More
& more people on prescription drugs:
potential for dangerous interactions
CONTRACEPTIVES
Side effects of hormonal contraceptives:
blood clots, can lead to heart attack and
stroke
can lodge in lungs (respiratory difficulties)
carcinogens:
•
•
•
•
•
mixed data
need more long term studies
increased breast cancer, ovarian & endometrial
decreased cervical cancer
different studies yield different data
increased infertility after long term (over 10
years) but could be due to age
CONTRACEPTIVES
Side effects of hormonal contraceptives:
liver tumors, can lead to death
Difficulty:
• so many different formulations, ever changing
• controversial, contradictory results
• who funded the research?
of most done by pharmaceutical companies (biased)
• how is the data obtained?
many based on self-report. Long term vs. short term
increased monilia and trichomona vaginal infections
more susceptible to STDs (vaginal pH altered)
nausea
migraines or severe headaches
drug interactions: either increase or decrease
effectiveness
CONTRACEPTIVES
Side effects of hormonal contraceptives (Cont’d):
depression
lower interest in sex
bloating and/or weight gain
interfere with milk production
cost
forgetting
infrequent sex
smokers
break-through bleeding
no STD protection
Environmental effects: the urine of users of hormonal
contraceptives gets into the water systems affecting
animals and possibly humans.
Remember “ACHES” for the Pill: Symptoms of
Possible Serious Problems With the Birth Control Pill
Initial
Symptoms
Possible Problem
A
Abdominal pain (severe)
Gallbladder disease, liver
tumour, or blood clot
C
Chest pain (severe) or
shortness of breath
Blood clot in lungs or
heart attack
H
Headaches (severe)
Stroke, high blood
pressure, or migraine
headache
E
Eye problems: blurred
vision, flashing lights, or
blindness
Stroke, high blood
pressure, or temporary
vascular problems at
many possible sites
S
Severe leg pain (calf or
thigh)
Blood clots in legs
CONTRACEPTIVES
NEW DEVELOPMENTS
The vaginal ring (which may also have estrogen)
is a flexible polymer ring, inserted into the vagina
for three weeks at a time. Removal at the start of
fourth week brings on period
Skin patch:
•
•
•
•
•
emits estrogen and progestin
same as pill
applied anywhere, once a week
four week cycle (three on, one off)
Not effective in heavy women (thick fat pad under skin
prevents good absorption)
Methotrexate (kills embryo) + misoprostol (a
prostaglandin) causes uterine contractions. In
Dr.’s office. It’s an abortifacient.
CONTRACEPTIVES
NEW
DEVELOPMENTS (Cont’d):
Essure coil:
• inserted into Fallopian tubes through
the vagina and uterus
• tissue grows around coil in 3 months,
results in total blockage
• sterility ($1,000, not covered)
• not 100% effective
CONTRACEPTIVES
NEW
DEVELOPMENTS:
Male Contraceptives
Testosterone enanthate:
• inhibits sperm production (injection)
Vaccines, FSH stops sperm production
Male reversible contraceptive
• IntraVas device
• two flexible silicon plugs inserted into vas deferens
• new method being tested in India: a polymer
injected into the vas, disables sperm
CONTRACEPTIVES
Natural
Methods: How good are they?
breastfeeding: only under certain conditions
rhythm or calendar: “Vatican roulette”
withdrawal (coitus interruptus)
avoid ejaculation (coitus reservatus)
sympto-thermal method: basal body
temperature + vaginal mucus
abstinence
SYMPTOTHERMAL METHOD
+ovulatory mucus observation
CONTRACEPTIVES
PERMANENT (MORE OR LESS) SURGICAL
METHODS:
Tubal ligation:
• Fallopian tubes cut, several methods, some failures.
• Usual surgical risks.
• Some evidence of increased incidence of hysterectomy for
various problems.
Vasectomy:
•
•
•
•
Much simpler surgery: vas deferens cut or blocked.
Can be done for reversibility (50-70% success).
Two months wait for sperm already there to die.
Very small % of men experience post-surgery discomfort for
a few months, most OK in 48 hrs.
Both methods still require condoms for STDs.
ABORTION:
Widely used for centuries.
Even early Christianity did not condemn it.
Until 20th century:
• quickening
Canadian laws not like U.S.
ABORTION
(Cont’d):
First trimester:
• Very early (2-3 weeks):
RU-486 – methotrexate + misoprostol
D & C (dilatation and curettage)
D & E (dilatation and extraction)
ABORTION
(Cont’d):
Second trimester: (10%)
• Saline injection:
Fetal death, delivery follows within 24 hrs.
• Prostaglandin injection:
Causes labour
• D & E:
Under general anesthetic.
Fetal skull may need to be crushed for passage
• Hysterotomy:
Like a Cesarean section
• Hysterectomy:
Removal of uterus and contents