An elderly woman with nausea, vomiting, diarrhea, fatigue and chills
advertisement
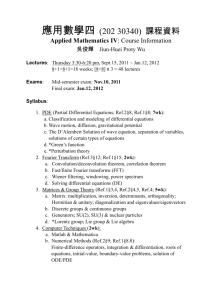
An elderly woman with nausea, vomiting, diarrhea, fatigue and chills Case Presentation , DR M Haghighi MD History of Present Illness A woman in her seventies was admitted to the hospital because of nausea, vomiting, weakness, diarrhea, abdominal pain, fatigue and chills. The patient had been well, with a history of diabetes mellitus and vascular disease, until approximately 4 weeks before when, in mid-summer, she was scratched and bitten numerous times on the arms, legs, and trunk by a stray or feral cat she had taken in. She was seen at another hospital where amoxicillinclavulanate, a tetanus booster, and rabies vaccination were reportedly administered, followed by additional rabies immunizations on days 4, 7, and 14. She reported no subsequent warmth, swelling, pain, or swollen glands in the arms, legs, axillae, or groin following the incident. One week before this presentation, in late summer, nausea, vomiting (without hematemesis), abdominal pain, watery non-bloody diarrhea, anorexia, weakness and fatigue developed, associated with intermittent chills. She came to the emergency department. She reported no known fever, headache, numbness, tingling, dyspnea, chest pain or rash. Past Medical History She had insulin-dependent diabetes mellitus (with average capillary glucose levels of 160 mg/dl), peripheral neuropathy, , hyperlipidemia, hypertension, peripheral vascular disease with recent angioplasty in the left leg, and chronic knee and wrist pain. Medications Medications included diltiazem, valsartanhydrochlorothiazide, insulin, acetaminophen and acetylsalicylic acid (81 MG). Allergies She was allergic to sulfa, gemfibrozil, and erythromycin, which had caused rashes. Family History There was a family history of diabetes mellitus and coronary artery disease. Epidemiological History She did not smoke, drink alcohol or use illicit drugs. She had not traveled recently. Physical Examination She was fully oriented. The temperature was 101.4°F (38.6°C), blood pressure 178/80 mm Hg, pulse 79 beats per minute, respirations 18 per minute and oxygen saturation 98% while breathing ambient air. There was a grade 1-2/6 systolic ejection murmur at the left lower sternal border, and heart sounds were otherwise normal. The abdomen was soft, minimally tender to palpation in left lower quadrant, without masses, and there were numerous scratches on her limbs and torso, without erythema or fluctuance. During the physical examination, she often repeated "I am tired" and "I can't remember". The remainder of the examination was normal. Studies The white cell count was 12,500 per cubic millimeter (reference range 4500-11,000; leukocytes 85%, lymphocytes 11%, monocytes 4%), hematocrit 32.9% (ref 36.0-46.0); hemoglobin 11.8gm/dl (ref 12.0-16.0), platelets 142,000 per cubic millimeter (ref 150-400). Tests of coagulation were normal. The blood level of sodium was 133 mmol/L (ref 135-145), potassium 3.1 mmol/L (ref 3.4-4.8), carbon dioxide 22.4 mmol/L (ref 23.0-31.9), glucose 166mg/dl (ref 70-110) and urea nitrogen 26mg/dl (ref 8-25); the estimated glomerular filtration rate was 57mL/min/1.73m2 (ref abnormal if <60 mL/min/1.73m2). Levels of chloride, calcium, phosphorus, magnesium, lactic acid, creatinine, were normal. Testing for antibodies to platelet factor 4 was negative. Urinalysis revealed 2+ glucose and protein, with few bacteria and squamous cells. Computed tomography (CT) of the abdomen and pelvis with the administration of intravenous contrast was normal. Culture of the stool grew normal enteric flora, without evidence of enteric pathogens. There was no evidence of Clostridium difficile toxin, protozoa, or helminth ova, and cultures of the blood and urine were sterile. She was admitted to the hospital. Intravenous fluids were administered for rehydration, and her other medications continued, with gradual improvement in most symptoms. Fatigue persisted, and on physical therapy evaluation, tremulousness and loss of balance were noted. On the fourth day, a neurological consultant obtained additional history that increased tremor was present for one week, and she had recent mid-to-lower back pain that did not radiate, without bowel or bladder incontinence, headache, neck stiffness or photophobia. On the fifth day, computed tomography (CT) of the head without the administration of contrast revealed central volume loss and chronic microvascular changes, without evidence of acute disease. Magnetic resonance imaging (MRI) of the lumbosacral spine with the administration of gadolinium showed focal T11-12 disc enhancement, thought to be related to degenerative joint disease, without abnormal enhancement. CT of the brain, without contrast. A lumbar puncture was performed; analysis of the cerebrospinal fluid revealed a glucose level of 99 mg/dl and total protein level 26 mg/dl, with 20 white cells per cubic millimeter (96% lymphocytes and 4% monocytes) and 4 red cells per cubic millimeter in Tube 1. Gram stain of the CSF showed very few mononuclear cells and no organisms. Infectious disease consultation was obtained. Her relatives reported that her speech was slower and wordfinding difficulties more severe than at baseline, and that she had been relatively confused on admission, with partial improvement since admission. Testing for antibodies (IgM) to Eastern Equine encephalitis (EEE) was negative. Testing of the CSF for Herpes simplex virus (types 1 and 2) DNA and enterovirus RNA was negative, as was testing the blood for antibodies to Bartonella henselae and Bartonella quintana (IgG and IgM) and Treponema pallidum. Culture of the CSF was sterile. Stool specimens were negative for C. difficile toxin and viruses.