Journal Club Slides
advertisement

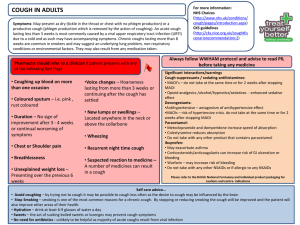
JAMA Pediatrics Journal Club Slides: Treatment of Acute Cough in Infants and Toddlers Paul IM, Beiler JS, Vallati JR, Duda LM, King TS. Placebo effect in the treatment of acute cough in infants and toddlers: a randomized clinical trial. JAMA Pediatr. Published online October 27, 2014. doi:10.1001/jamapediatrics.2014.1609. Copyright restrictions may apply Introduction • Background – Cough is a frequent symptom in infants and toddlers and is one of the most common reasons children visit a health care provider. – Little evidence supports use of over-the-counter medicines for acute cough, particularly in younger children. – Several studies have demonstrated the effectiveness of honey for treatment of acute cough, but honey cannot be safely consumed by children younger than 1 year. – Agave nectar has physical properties similar to honey but without known risk of infantile botulism. • Study Objective – To compare the effect of a novel formulation of pasteurized agave nectar vs placebo and no treatment on nocturnal cough and the sleep difficulty associated with nonspecific acute cough in infants and toddlers. Copyright restrictions may apply Methods • Study Design – Partially double-blinded, randomized trial comparing a single nighttime dose of agave nectar plus grape flavoring, placebo (grape-flavored water), and no treatment. – Surveys were administered to parents on 2 consecutive days: • Day 1: day of presentation, following no treatment the prior night. • Day 2: following agave nectar, placebo, or no treatment on previous night. – Agave and placebo dosing stratified by age: • 3 mL for ages 2-5 months, 4 mL for ages 6-23 months, 5 mL for ages 24-47 months. • Setting – Two outpatient, general pediatric practices. Copyright restrictions may apply Methods • Patients – 119 children aged 2 to 47 months with nonspecific acute cough, nocturnal symptoms, and illness duration of 7 days or less. – Patients were excluded if they had signs or symptoms of a more treatable disease or a history of asthma, chronic lung disease, or other severe chronic diseases. – Sample size calculations indicated that 120 participants (40 per arm) would have 80% power to detect a 0.5-point difference between treatment groups incrementally for the primary efficacy measure of change in cough frequency between the first night and the end of the second night. • Outcomes – Cough frequency, cough severity, bothersome nature of cough, rhinorrhea severity, congestion severity, and child and parent sleep quality. – Parental assessments of outcomes were assessed through a version of previously used and validated questions using a 7-point ordinal scale. Copyright restrictions may apply Methods • Limitations – Each child had a physician visit between the 2 nights of the study, which may explain some of the improvement in all of the groups, including the no treatment group. – Upper respiratory infections naturally improve with time, making it more difficult to detect treatment effects. – No objective outcome measures were used. – Compliance with treatment administration could not be guaranteed. Copyright restrictions may apply Results • 119 children completed the trial (mean [SD] age, 22.9 [14.0] months), with a mean (SD) cough duration of 4.0 (1.5) days prior to enrollment. • No demographic or baseline symptom severity differences were observed between the study groups. • For all outcomes except for cough bothersomeness to the child, both the agave nectar and placebo groups had significant improvement compared with the no treatment group, but no differences were detected for any outcome between the agave nectar and placebo groups. • A combined symptom score was calculated using all study outcomes, including cough frequency, cough severity, congestion severity, rhinorrhea severity, and cough effect on child and parent sleep. Again, both agave nectar and placebo were superior to no treatment, but no significant differences were detected between the agave nectar and placebo groups. Copyright restrictions may apply Results Between-Night Treatment Effects of Agave Nectar, Placebo, and No Treatment on Study Outcomes Using a Likert-Type Scale Copyright restrictions may apply Results • Secondary Analyses – No effect of illness duration was observed on treatment effect. – No significant differences were found between the study groups for other remedies given (eg, acetaminophen, ibuprofen). – Subgroup analysis for 30 participants younger than 1 year: • For all outcomes, the agave nectar did result in more than a 0.5point greater improvement than for the placebo (the a priori definition of a clinically meaningful difference), a finding limited by the small subgroup sample size and the reduced power to detect a statistically significant finding. – Adverse effects were rare; no significant differences were found between the study groups for any individual adverse event. Copyright restrictions may apply Comment • A significant placebo effect exists in the treatment of young children with nonspecific acute cough because the agave nectar and placebo both resulted in perceived improvement of child symptoms by parents compared with no treatment. • The common clinical advice of watchful waiting with no treatment may not be the best advice for parents whose infants and toddlers are struggling with cough and its associated sleep disruption. • These findings strengthen the validity of prior studies suggesting that honey is effective for acute cough given that similar methods were used in the current study with only a placebo effect demonstrated. • The intriguing (although not statistically significant) findings among children younger than 1 year suggest that further evaluation of agave nectar among a larger cohort in this age group may be warranted as this group is the most germane to therapeutic measures for nonspecific acute cough. Copyright restrictions may apply Contact Information • If you have questions, please contact the corresponding author: – Ian M. Paul, MD, MSc, Department of Pediatrics, Penn State College of Medicine, Mail Code HS83, 500 University Dr, Hershey, PA 17033-0850 (ipaul@psu.edu). Funding/Support • This study was funded by an unrestricted grant to the Penn State College of Medicine by Zarbee’s Inc. Conflict of Interest Disclosures • Dr Paul reported serving as a paid consultant to Zarbee’s Inc in 2012, with a total income of $1350; this consulting relationship was discontinued upon discussions of performing a clinical trial. Dr Paul’s relationship was evaluated and supervised by the Penn State College of Medicine Conflict of Interest System Committee. No other disclosures were reported. Copyright restrictions may apply