Can we select patients most likely to benefit
from pemetrexed continuation maintenance?
SEONC00109
Baseline characteristics for patients surviving at
least 6, 12, 18 and 24 months1
Pemetrexed Arm %Pts
Median age (yrs)
Baseline
6 mos
12 mos
18
18 mos
mos
24mos
61
61
62
62
62
63
Age <65
66
65
62
62
62
61
Male
56
55
54
47
47
49
Caucasian
94
95
96
96
96
96
Ever smoker
76
72
69
66
66
68
Never smoker
23
27
30
33
33
30
0
32
39
42
46
46
53
1
68
61
59
54
54
47
Stage IV
91
92
92
92
92
90
86
89
89
88
88
89
7
6
7
77
6
CR/PR
44
44
45
48
48
47
SD
53
55
54
50
50
51
3
1
2
22
3
Sex/ethnic group
Smoker
ECOG PS
Histology
Adenocarcinoma
Large cell
Induction response
PD/Unknown
Baseline characteristics for patients surviving at
least 6, 12, 18 and 24 months1
Pemetrexed Arm %Pts
Median age (yrs)
Baseline
6 mos
12 mos
18 mos
24mos
61
61
62
62
63
Age <65
66
65
62
62
61
Male
56
55
54
47
49
Caucasian
94
95
96
96
96
Ever smoker
76
72
69
66
68
Never smoker
23
27
30
33
30
1
32
68
39
61
42
59
46
54
53
47
Stage IV
91
92
92
92
90
86
89
89
88
89
7
6
7
7
6
44
53
44
55
45
54
48
50
47
51
3
1
2
2
3
Sex/ethnic group
Smoker
ECOG PS
0
Histology
Adenocarcinoma
Large cell
Induction response
CR/PR
SD
PD/Unknown
Baseline characteristics for patients surviving at
least 6, 12, 18 and 24 months1
Pemetrexed Arm %Pts
Median age (yrs)
Sex/ethnic group
Baseline
6 mos
12 mos
18 mos
24mos
62
62
63
PARAMOUNT
61
61
data shows
Age <65
66
65
62
62
61
Male
56
55
54
47
49
Caucasian
94
95
96
96
96
Smoker
Ever smoker
OS benefit seen across
all subgroups
76
72
69
66
68
23
27
30
33
30
32
39
42
46
53
1
68
61
59
54
47
Stage IV
91
92
92
92
90
86
89
89
88
89
7
6
7
7
6
CR/PR
44
44
45
48
47
SD
53
55
54
50
51
3
1
2
2
3
Never smoker
ECOG PS
0
Histology
Adenocarcinoma
Large cell
Induction response
PD/Unknown
Basis for maintenance treatment decision
Maintenance Treatment Decision
Overall
treatment
goals
Performance
status
Tolerance to
induction
therapy
Did PARAMOUNT assess patients’ Quality of Life?
PARAMOUNT: study objectives2
Primary
objective
• Progression-free survival (PFS)
Secondary
objective
•
•
•
•
•
Overall survival (OS)
Objective tumor resposne rate (RR) (RESIST 1.0)
Patient-reported outcomes (EQ-5D)
Resource utilisation
Adverse events (AEs)
EQ-5D: EuroQol 5-dimensional questionnaire3
Questionnaire
VAS (Visual Analog Scale)
Best imaginable health state
By placing a tick in one box in each group below, please indicate which
statements best describe your own health state today.
Mobility
I have no problems in walking about
I have some problems in walking about
I am confined to bed
Self-Care
I have no problems with self-care
I have some problems washing or dressing myself
I am unable to wash or dress myself
✔
☐
☐
☐
✔
☐
☐
☐
Usual Activities (e.g. work, study, housework, family or leisure activities)
I have no problems with performing my usual activities
I have some problems with performing my usual activities
I am unable to perform my usual activities
✔
☐
☐
☐
Pain/Discomfort
I have no pain or discomfort
I have moderate pain or discomfort
I have extreme pain or discomfort
☐
☐
☐
✔
Anxiety/Depression
I am not anxious or depressed
I am moderately anxious or depressed
I am extremely anxious or depressed
✔
☐
☐
☐
Worst imaginable health state
High EQ-5D compliance3
Induction
79.4%
Pemetrexed
arm
Placeboarm
84.3%
80.9%
PARAMOUNT: EQ-5D results and safety data
EQ-5D results3
Safety data4
>10 MTC Cycles
Grade 1
Event (%)
Grade 2
Grade 3/4
PEM PBO PEM PBO PEM PBO
Fatigue
15
0
13
13
8
6
Renal*
4
6
8
0
1
0
Rash
4
0
1
0
0
0
Edema
13
13
8
0
0
0
Anemia
4
6
12
0
7
0
Neutropenia
4
0
7
0
11
0
What are the QoL and safety results in
PARAMOUNT?
QoL and safety in PARAMOUNT
Good Overall QoL during maintenance
Induction therapy
Maintenance therapy
QoL and safety in PARAMOUNT
Good Overall QoL during maintenance
Induction therapy
Maintenance therapy
QoL and safety in PARAMOUNT
Rate of AEs possibly related to maintenance pemetrexed vs placebo2,†
4%* n=16
<1%* n=1
Anaemia
4%* n=15
<1%* n=1
Fatigue
Low rate of discontinuations due to
4%*
1%
Neutropenia
Infection 3
0%*adverse events
1%
n=13
n=1
n=4
n=2
2% n=6
0%* n=1
Leucopenia
1% n=3
0% n=1
Pain
9.2% for1%maintenance pemetrexed
1%
Neuropathy
1%
3.9% for0%placebo
Thrombocytopenia
n=4
n=1
0
10
20
n=1
n=1
30
0
10
Pemetrexed
(n=359)
20
30
placebo
(n=180)
* Difference between treatment groups was significant (Fisher’s exact test p≤0.05).
† Adverse events were reported using Common Terminology Criteria for Adverse Events version 3.0 (NCI 2006). Alanine aminotransferase, Nausea, Vomiting, Mucositis or
stomatitis, Oedema, Anorexia, Diarrhoea, Watery eye, Constipation Grade 3/4 adverse events were reported for less than 1% of patients.
Adapted from: 1,2
QoL and safety in PARAMOUNT
Change in ECOG PS from randomisation to last maintenance treatment3
% Change from Baseline in ECOG
Performance Status
100
90
14.7%
12.6%
Worse
No Change
80
Better
70
60
77.8%
77.3%
7.5%
10.2%
Pemetrexed
Placebo
50
40
30
20
10
0
* Difference between treatment groups was significant (Fisher’s exact test p≤0.05).
† Adverse events were reported using Common Terminology Criteria for Adverse Events version 3.0 (NCI 2006). Alanine aminotransferase, Nausea, Vomiting, Mucositis or
stomatitis, Oedema, Anorexia, Diarrhoea, Watery eye, Constipation Grade 3/4 adverse events were reported for less than 1% of patients.
Adapted from: 1,2
QoL and safety in PARAMOUNT
EQ-5D index scores: Quality of life was maintained throughout treatment3
Improvement
Mean score
0.8
0.7
0.6
1
2
3
4
1
2
3
4
5
Induction cycles
* p≤0.05, within-group change from baseline. † p≤0.05, comparing the difference in mean changes from baseline between treatment arms.
Adapted from: 3
6
QoL and safety in PARAMOUNT
EQ-5D index scores: Quality of life was maintained throughout treatment3
Improvement
Mean score
0.8
0.7
Pemetrexed
Placebo
0.6
1
2
3
Induction cycles
4
1
2
3
4
5
Maintenance cycles
* p≤0.05, within-group change from baseline. † p≤0.05, comparing the difference in mean changes from baseline between treatment arms.
Adapted from: 3
6
QoL and safety in PARAMOUNT
VAS: No overall treatment differences in quality of life were observed
during induction3
Improvement
Mean score
0.8
0.7
Pemetrexed
Placebo
0.6
1
2
3
4
1
Induction cycles
† p≤0.05, comparing the difference in mean changes from baseline between treatment arms.
Adapted from: 3
2
3
4
Maintenance cycles
5
6
QoL and safety in PARAMOUNT
VAS: No overall treatment differences in quality of life were observed
during induction3
Improvement
Mean score
0.8
0.7
Pemetrexed
Placebo
0.6
1
2
3
4
1
Induction cycles
† p≤0.05, comparing the difference in mean changes from baseline between treatment arms.
Adapted from: 3
2
3
4
Maintenance cycles
5
6
QoL and safety in PARAMOUNT
• Survival significantly improved with pemetrexed continuation
maintenance therapy vs placebo5
• HR=0.78 (95% CI: 0.64-0.96)5
• No statistical differences observed in patient-reported QoL
between maintenance treatment arms3
Does long-term pemetrexed maintenance
have an impact on QoL?
Pemetrexed/cisplatin followed by pemetrexed
demonstrated a statistically significant OS benefit
in advanced non-squamous NSCLC6
pemetrexed + BSC (n=359)
placebo + BSC (n=180)
1.0
0.9
Survival probabality (%)
NOT reflected in the data endpoints
Induction = 4 cycles
of pemetrexed/cisplatin
Overall survival from randomisation
0.8
HR=0.78 (95% CI 0.64–0.96); p=0.0195
0.7
0.6
32%
0.5
0.4
24-months
survival rate
32%
0.3
0.2
21%
0.1
0
0
6
12
18
24
Time from randomisation (months)
30
36
Summary of maintenance therapy4
Pemetrexed
(n=359)
Placebo
(n=180)
4 (1–44)
4 (1–38)
8
5
≤10 cycles
76
90
>10 cycles
24
9
12
4
Median number of cycles (range)
Mean number of cycles
% of pts receiving MTC
% discontinuations due to
possibly drug-related AE
Adapted from: 4
Possible drug-related CTCAEs occurring
in all cycles of maintenance therapy4
>10 MTC Cycles
Grade 1
Event (%)
PEM
Grade 2
PBO
Grade 3/4
PEM
PBO
PEM
PBO
Fatigue
15
0
13
13
8
6
Renal*
4
6
8
0
1
0
Rash
4
0
1
0
0
0
Edema
13
13
8
0
0
0
Anemia
4
6
12
0
7
0
Neutropenia
4
0
7
0
11
0
* creatinine, GFR, ranal failure, and genitourinary-other.
No significant differences in drug-related
grade 3/5 toxicities – except grade 3/4 neutropenia3
≤6
maintenance cycles
Neutropenia
Grade 3/4
2.2%
Infections
Grade 3/5
2.9%
50
8.3%
1.2%
0
>6
p=0.015
p=0.691
50
Possible drug-related grade 1/2 adverse events3
≤6
maintenance cycles
8.7%
Nausea
16.7%
2.5%
Neutropenia
Sensory neuropathy
Ocular/visual events
11.9%
1.5%
6.0%
2.5%
13.1%
0.4%
Headache
50
>6
3.6%
0
p=0.044
p=0.001
p=0.036
p=0.001
p=0.041
50
Long-term pemetrexed maintenance impact on QoL
EQ-5D results
Pemetrexed
well-tolerated
safety profile
PS changes
Majority of patients
maintain QoL
Are PARAMOUNT QoL and safety results consistent
with JMEN?
Maintenance pemetrexed
in PARAMOUNT2 and JMEN7,8
PARAMOUNT
Paz-Ares et al. 2012
JMEN
Ciuleanu et al. 2009
Maintenance therapy with pemetrexed plus best supportive
care versus placebo plus best supportive care after induction
therapy with pemetrexed plus cisplatin for advanced nonsquamous non-small-cell lung cancer (PARAMOUNT):
a double-blind, phase 3, randomised controlled trial
•
Well-tolerated
safety profile,
consistently reported
•
QoL is well maintained
and similar to placebo
Maintenance pemetrexed plus best supportive care versus
placebo plus best supportive care for non-small-cell lung
cancer: a randomised, double-blind, phase 3 study
JMEN: Drug-related toxic effects8
Grades 3 or 4
Pemetrexed
Placebo
Hematologic toxicities
Neutropenia*
13
(3%)
0
Anemia
12
(3%)
1
(<1%)
7
(2%)
1
(<1%)
ALT
1
(<1%)
0
AST
0
Leukoperia
Non-hematologic toxicities
0
Fatigue†
22
(5%)
1
Anorexia
8
(2%)
0
Infection
7
(2%)
0
Diarrhoea
2
(<1%)
0
Nausea
4
(<1%)
1
Vomiting
1
(<1%)
0
Sensory neuropathy
3
(<1%)
0
Mukositis stomatitis
3
(<1%)
0
Rash
1
(<1%)
0
(<1%)
(<1%)
ALT=alanine aminotransferase. AST=aspartate aminotransferase. *p<0.05 for grade 3 or 4 rates of neutropenia and fatigue between study groups.
†Updated safety analysis done 6 months after initial analysis of progression-free survival. For the purpose of this table, a cut-off of 5% was used for inclusion of all events for which
the investigator considered a possible link with pemetrexed.
Adapted from: 4
PARAMOUNT: CTCAEs possibly related to study
drug during maintenance3
Grades 3 or 4
Pemetrexed
Placebo
Toxicity*
Laboratory
Anemia
16
1
Neutropenia
13
0
(0.6%)
Non-laboratory
Fatigue (asthenia, lethargy, malaise)
15
(4%)
1
Anorexia
1
(0.3%)
0
Constipation
0
0
Diarrhea
0
0
Mucositis stomatitis
1
(0.3%)
0
Nausea
1
(0.3%)
0
Vomoting
0
0
Edema
0
0
Sensory neuropathy
1
Watery eye (epiphora, tearing)
0
Pain
3
(0.3%)
1
(0.6%)
(0.6%)
0
(0.8%)
0
Toxicities were reported using CTCAE version 3.0 (National Cancer Institute 2006). Toxicities occurring in ≥ 3% of patients on either or both arms are listed. Two grade 5 events
(deaths) considered possibly related to study drug occurred during the maintenance period: pemetrexed – pneumonia; placebo-sudden death. Difference between treatment arms is
statistically significant (Fisher‘s exact test p ≤0.05). CTCAE, Common Terminology Criteria for Adverse Events.
Adapted from: 4
QoL in PARAMOUNT and JMEN
QoL Measurement
PARAMOUNT3
EQ-5D
JMEN7
LCSS
QoL in PARAMOUNT and JMEN
Mean maximum improvement in LCSS items7
Mean maximum improvement (mm)
12
p=0.136
p=0.959
p=0.592
p=0.897
Interference
with
activity
Overall
Overall
quality of
quality
of
life
10
p=0.533
p=0.204
p=0.039
6
4
p=0.831
2
0
Adapted from: 1,2
p=0.192
8
Loss of
appetite
Fatigue
Fatigue
Coogh
Dyspnoea
Haemolysis
Pain
Symptom
distress
Pemetrexed
Placebo
QoL in PARAMOUNT and JMEN
Patients are able to maintain their overall good quality of life3
Quality of lifeBest
imaginable health state
Worst imaginable health state
How robust are the findings of PARAMOUNT to
support a change in the treatment paradigm?
The robust findings of PARAMOUNT and their
likely impact on the current treatment paradigm2,5,10
The robust PARAMOUNT
results are based on a
number of valid points
The robust findings of PARAMOUNT and their
likely impact on the current treatment paradigm2,5,10
Direction of magnitude of PFS
and OS results are consistent
and favour pemetrexed
continuation maintenance
HR 0.62 (95% CI 0.49-0.79; p<0.0001)
PFS:
4.1 vs 2.8 months
OS:
16.9 vs 14.0 months
from induction
HR 0.78 (95% CI 0.64-0.96; p=0.0195)
The robust findings of PARAMOUNT and their
likely impact on the current treatment paradigm2,5,10
Direction of magnitude of PFS
and OS results are consistent
and favour pemetrexed
continuation1.0
maintenance
Investigator-determined PFS
results confirmed by
independent review
Survival probability (%)
PFS: Primary endpoint
pemetrexed + BSC (n=358)
placebo + BSC (n=180)
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0
HR 0.62 (0.49–0.79)
0
3
6
9
Time (months)
12
15
The robust findings of PARAMOUNT and their
likely impact on the current treatment paradigm2,5,10
Subgroup OS Hazard Ratio
Direction of magnitude
of PFS
All
Stage IV
and OS results
are consistent
IIIB
and favour pemetrexed
CR/PR
Induction response
continuation maintenance
SD
N
HR (95% CI)
Investigator-determined
PFS
0.78
results confirmed by0.79
independent review 0.82
0.81
539
490
49
234
285
0.76
CR/PR patients: OS HR=0.81
1
363
0.82
0
173
0.70
Never-smoker
117
0.75
Smoker
418
0.83
Male
313
0.82
SD patients:
226
Pre-randomisation
ECOG PS
Smoking status
Sex
Female
Relative treatment
effect of
Age (years) <70
≥70
pemetrexed consistent
across
<65
≥65
subgroups
Histology
Adenocarcinoma
OS HR=0.76
447
92
0.73
0.75
0.89
350
0.82
189
0.71
471
0.80
Large cell carcinoma
36
0.44
Other
32
0.81
Favours pemetrexed
0
0.2
0.4
0.6
0.8
1
1.2 1.4
1.6
1.8
2.0
Favours placebo
The robust findings of PARAMOUNT and their
likely impact on the current treatment paradigm2,5,10
pemetrexed
placebo
Direction of magnitude of PFS
Investigator-determined
PFS
(n=359) %*
(n=180) %*
and OS results are consistent
results confirmed by
64
Patients
with
PDT
64
and
favour
pemetrexed
independent review72
Drug name
continuation maintenance
Erlotinib
40
Docetaxel†
32
Gemcitabine
10
Vinorelbine
8
Investigational drug
6
Relative
treatment effect of
Carboplatin
5
Paclitaxel
pemetrexed
consistent across 3
Pemetrexed
2
subgroups
Cisplatin
1
43
43
8
6
4
Post-discontinuation
4 treatment
3
options were well balanced
4
between the two arms
2
* Data expressed as % of randomized patients. Systemic therapies used in ≥2% of patients in either arm are shown.
† Only docetaxel usage differed significantly between arms (p=0.013).
What are the key takeaways for clinical practice?
2
Key PARAMOUNT takeaways
3
1
Results confirmfirst
PARAMOUNT:
the study
importance
to show
of that
choosing
Significant
OS
Benefit OS
consistent
benefit across
in favorall
of sub-groups,
Pemetrexed
Continuation
the
best treatment
Maintenance
up-front,
has
based
an impact
on histology
on
2,10 10
Continuation
with
acceptable
Maintenance
toxicity
10 characteristics2,10
disease
and
other
course
patient
4
References
1.
Reck M et al. PARAMOUNT: Descriptive subgroup analyses of final overall survival (OS) for the phase III study of maintenance
pemetrexed (PEM) versus placebo (PLB) following induction treatment with PEM plus cisplatin (CIS) for advanced nonsquamous (NS)
non-small cell lung cancer. ESMO Congress, Vienna, Austria, 2012. Abstract 1235PD.
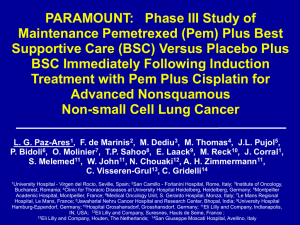
2.
Paz-Ares L et al. Maintenance therapy with pemetrexed plus best supportive care versus placebo plus best supportive care after
induction therapy with pemetrexed plus cisplatin for advanced non-squamous non-small-cell lung cancer (PARAMOUNT): a double-blind,
phase 3, randomised controlled trial. Lancet Oncol 2012;13:247-255.
3.
Gridelli C et al. Safety, resource use, and quality of life in PARAMOUNT: a phase III study of maintenance pemetrexed versus placebo
after induction pemetrexed plus cisplatin for advanced nonsquamous non-small-cell lung cancer. J Thorac Oncol. 2012;7(11):1713-1721.
4.
Pujol JL et al. Updated safety and quality of life results of PARAMOUNT study: maintenance pemetrexed + best supportive care (BSC)
vs placebo plus BSC immediately following induction treatment with pemetrexed plus cisplatin for advanced nonsquamous non-small cell
lung cancer. ESMO Congress, Vienna, Austria, 2012. Abstract 3376.
5.
Paz-Ares L et al. PARAMOUNT: Final overall survival (OS) results of the phase III study of maintenance pemetrexed (pem) plus best
supportive care (BSC) versus placebo (PLB) plus BSC immediately following induction treatment with pem plus cisplatin (cis) for
advanced nonsquamous (NS) non-small cell lung cancer (NSCLC). J Clin Oncol 30, 2012 (suppl; abstr LBA7507).
6.
ALIMTA Summary of Product Characteristics. Eli Lilly and Company Limited. November 2012.
7.
Belani CP et al. Quality of life in patients with advanced non-small-cell lung cancer given maintenance treatment with pemetrexed versus
placebo (H3E-MC-JMEN): results from a randomised, double-blind, phase 3 study. Lancet Oncol 2012;13:292-299.
8.
Ciuleanu T et al. Maintenance pemetrexed plus best supportive care versus placebo plus best supportive care for non-small-cell lung
cancer: a randomised, double-blind, phase 3 study. Lancet 2009;374:1432-1440.
9.
Hanna N et al. Randomized phase III trial of pemetrexed versus docetaxel in patients with non-small-cell lung cancer previously treated
with chemotherapy. J Clin Oncol 2004;22:1589–1597.


![[Lecture 19] studio system 2 for wiki](http://s2.studylib.net/store/data/005217793_1-c296c1b3b7b87d52a223478e417a702f-300x300.png)