NEMATODES
Faculty: SAMUEL AGUAZIM, M.D.
• Lange Chapter 56
1
2
3
case
• 4 year old female with constant scratching
of her buttocks for 1 week. The mother
says that the child has been very irritable,
uncomfortable at night.
• On examination of her anal area:
numerous scratch marks, erythematous
and swollen.
4
• Pyrantel pamoate
2 doses
• Recovered
• Impression: Pinworm
infection, secondary
to Enterobius
vermicularis
5
Nematodes
• are roundworms with a cylindrical body and
complete digestive tract, including a mouth and
an anus.
• The body is covered with a noncellular, highly
resistant coating called a cuticle.
• Nematodes have separate sexes; the female is
usually larger than the male
6
Nematodes
The medical important nematodes can be
divided into two categories according to
their primary location in the body to:
Intestinal Nematodes
Tissue Nematodes
7
Intestinal Nematodes
Enterobius vermicularis
most common helminthic infection in the
United States
Disease: Pinworm infection.
Characteristics: Intestinal nematode.
8
Enterobius vermicularis
Life cycle:
• confined to humans.
• The infection is acquired by ingesting the worm eggs.
• The eggs hatch in the small intestine, where the larvae
differentiate into adults and migrate to the colon.
• The adult male and female worms live in the colon, where
mating occurs.
• At night, females migrate from the anus and lay many
thousands of fertilized eggs on perianal skin and in
environment.
• Embryo within egg becomes an infective larva within 4—6
hours.
• Reinfection can occur if they are carried to the mouth by
fingers after scratching the itching skin.
9
Life cycle of Enterobius
10
11
Enterobius vermicularis adult male and female
Enterobius egg(flattened side with
larvae inside)
12
MOT: ingestion of eggs
Females lay
eggs in
the perianal
area at night
13
14
Enterobius vermicularis
Transmission: Transmitted by ingesting eggs.
Humans are the only hosts. Occurs worldwide.
Pathogenesis: Worms and eggs cause perianal
itching. Scratching predisposed to Secondary
bacterial infection
Laboratory Diagnosis: Eggs visible by
“Scotch tape” technique. Eggs are not found in
stool . Adult worms found in stool or near anus.
Treatment: Mebendazole
15
Memory Tool
• On the bus (Enterobius), you sit on a pin
(pinworm), and get an itchy bottom and
use scotch tape to make it feel better.
16
Trichuris trichiura
Disease: Whipworm infection
Characteristics: Intestinal nematode. The
characteristic of “whiplike” apperance of the
adult worm.
Life cycle:
• Humans ingest eggs, which develop into adults
in gut.
• Eggs are passed in feces into soil, where they
embryonate, ie, become infectious.
17
18
The characteristic of “whiplike” apperance of the adult worm.
Trichuris trichiura
Transmission:
• More than 500 million infected.
• Transmitted by food or water contaminated with soil
containing eggs.
• Humans are the only hosts. Occurs worldwide,
especially in the tropics.
Pathogenesis:
• Worm in gut usually causes little damage.
• The whipworm infects about 2 million children in the
U.S.
• Causes rectal pruritis and tenesmus, which often
results in rectal prolapse.
19
Infectious Diseases
Whipworm – Rectal Prolapse
20
Infectious Diseases
Whipworm – Rectal Prolapse
21
Trichuris trichiura
Laboratory Diagnosis:
• Eggs visible in feces.
• The egg is barrel-shape with a plug at each
end, in the stool.
Treatment: Mebendazole.
Prevention: Proper disposal of human waste
22
Trichuris trichiura eggs, a typical barrel shape two polar plugs, that are
23
unstained
Trichuris trichiura
• Tricksy (Trichuris) carries a whip and ate
eggs which gave her rectal prolapse. Poor
Tricksy!!!
24
Ascaris
Disease: Ascariasis.
Characteristics: Intestinal nematode.
Life cycle:
• Humans ingest eggs, which form larvae in gut.
• Larvae migrate through the blood to the lungs, where they
enter the alveoli, pass up the trachea, and are swallowed.
• In the gut, they become adults and lay eggs that are passed in
the feces.
• They embryonate, ie, become infective in soil.
• The adult worms are the largest intestinal nematodes (25
cm or more).
25
Ascaris Life Cycle
26
Ascaris adult male and female
27
28
Erratic ascariasis
29
Ascaris
Transmission: food contaminated with soil containing eggs.
Humans are the only hosts. Endemic in the tropics.
Pathogenesis: Larvae in lung can cause pneumonia. Heavy
worm burden can cause intestinal obstruction or
malnutrition.
Laboratory Diagnosis: Eggs visible in feces. Eggs are
oval with irregular surface. Eosinophilia occurs.
Treatment:
Mebendazole
Prevention: Proper disposal of human waste
30
Eggs are
oval with
irregular
surface
31
Billy (biliary obstruction) drives his car (Ascaris) while
eating eggs and gets short of breath. Poor Billy!!! Add
intestinal obstruction
32
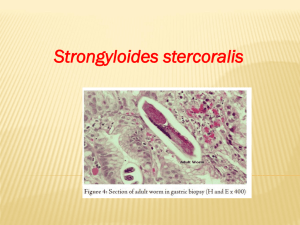
Strongyloides
Disease: Strongyloidiasis
Characteristics: Intestinal nematode.
Life cycle:
• Larvae penetrate skin, enter the blood, and
migrate to the lungs. They move into alveoli and
up the trachea and are swallowed.
• become adults and enter the mucosa, where
females produce eggs that hatch in the colon
into noninfectious, rhabditiform larvae that are
usually passed in feces.
• NOTE: the only helminth to secrete larvae (and not eggs)
in feces
33
Strongyloides
• Occasionally, rhabditiform larvae molt in the gut to
form infectious, filariform larvae that can enter the
blood and migrate to the lung (autoinfection).
• The noninfectious larvae passed in feces form
infectious filariform larvae in the soil.
• These larvae can either penetrate the skin or form
adults.
• Adults in soil can undergo several entire life cycles
there.
• This free-living cycle can be interrupted when
filariform larvae contact the skin.
34
Strongyloides
Transmission: Filariform larvae in soil penetrate skin. Endemic
in the tropics.
Pathogenesis:
• Little effect in immunocompetent persons.
• In immunocompromised persons, massive superinfection can
occur accompanied by secondary bacterial infections.
Laboratory Diagnosis: Larvae visible in stool. Eosinophilia
occurs.
Treatment: Thiabendazole.
Prevention: Proper disposal of human waste. Use of footwear
35
Memory Tool
• The strongman (Strongyloides) is brought down
by a larvae penetrating his skin causing
pulmonary distress and superinfection. Poor
strongman!
36
Ancylostoma duodenale
Necator Americanus
Disease:
Hookworm.
Characteristics: Intestinal nematode.
37
Ancylostoma
duodenale
• Filariform larvae in soil penetrate skin of feet,
enter the blood, and migrate to the lungs.
• enter alveoli, pass up the trachea, then are
swallowed.
• become adults in small intestine and attach to
walls via teeth (Ancylostoma) or cutting plates
(Necator).
• Eggs are passed in feces and form
noninfectious rhabditiform larvae and then
infectious filariform larvae.
38
Ancylostoma duodenale adult male and female
39
Ancylostoma duodenale
Transmission: Filariform larvae in soil penetrate skin of feet.
Humans are the only hosts.
Pathogenesis:
Anemia
gastrointestinal tract.
due
to
blood
loss
from
Laboratory Diagnosis: Eggs visible in feces. Eosinophilia
occurs.
Treatment: Mebendazole AND Iron therapy
Prevention: Use of footwear. Proper disposal of human waste.
40
ANCYLOSTOMA BRAZILIENSE
ANCYLOSTOMA CANINUM
• DOG and CAT Hook worm
• Forms/ Transmission.
• Filariform larvae penetrate intact skin but
cannot mature in humans
• Disease/organ most affected
• Cutaneous larvae migrans: intense itching
• Tunnels through tissue
• Diagnosis: clinical signs
41
• Treatment- ivermectin
Ancylostoma braziliensis
(cutaneous larva migrans/creeping eruption)
Pathognomonic:
serpiginous
tunnels
Lacks hydrolytic enzymes to penetrate
into the dermis;
remains localized in the epidermis
42
Ancylostoma braziliensis
(cutaneous larva migrans/creeping
eruption)
Dog, cat hookworm
Gulf states, South US
freezing with liquid nitrogen/ethyl
chloride;
Mebendazole
43
Trichinella
Disease: Trichinosis.
Characteristics: Intestinal nematode that
encysts in tissue.
44
Trichinella Life cycle:
• Humans ingest under cooked pork and other
meat containing encysted larvae, which mature into
adults in small intestine.
• Female worms release larvae that enter blood and
migrate to skeletal muscle or brain, where they
encyst.
• Pigs:most important reservoirs of human disease in
USA, except Alaska where bears are the ones.
Reservoir hosts are primarily pigs and rats.
• Humans are dead end hosts.
• Occurs worldwide but endemic in eastern Europe 45
and west Africa
Trichinella life cycle
46
Encysted larvae of Trichinella in pressed muscle tissue. The coiled 47
larvae can be seen inside the cysts. CDC
Trichinella
Pathogenesis: Inflammation of muscle
Laboratory Diagnosis:
• Encysted larvae visible in muscle biopsy
• Eosinophilia
• Serologic tests positive.
Treatment: Thiabendazole effective early against
adults. None for established disease
Prevention: Adequate cooking of pork
48
Memory Tool
• A tricky (Trichinella) pig caused cysts in
his owners muscles.
49
Tissue nematode
Dracunculus
Disease: Dracunculiasis.
Characteristics: Tissue nematode.
50
Dracunculus Life cycle:
• Humans ingest copepods containing infective
larvae in drinking water.
• Larvae are released in gut, migrate to body
cavity, mature, and mate.
• Fertilized female migrates to subcutaneous
tissue and forms a papule, which ulcerates.
• Motile larvae are released into water, where
they are eaten by copepods and form
infective larvae.
51
Dracunculus
Transmission:
•
•
•
•
copepods in drinking water.
Humans are definitive hosts.
Many domestic animals are reservoir hosts.
Endemic in tropical Africa, Middle East, and India
Pathogenesis:
• Adult worms in skin cause inflammation and ulceration.
Treatment:
• Niridazole.
• Extraction of worm from skin ulcer.
Prevention:
• Purification of drinking water
52
Dracunculiasis
53
Dracunculus: posterior end
54
Dracula ate an infected
crustacean and got an ulcer
with protruding worm.
He removed the worm by
winding it around a stick.
55
Loa Loa (eye worm)
Disease: Loiasis.
Characteristics: Tissue nematode.
56
Loa Loa
Life cycle:
• Bite of deer fly (mango fly) deposits infective
larvae, which crawl into the skin and develop
into adults that migrate subcutaneously.
• Females produce microfilariae, which enter
the blood.
• These are ingested by deer flies, in which the
infective larvae are formed.
57
Loa Loa
Transmission: Transmitted by deer flies. Humans are the only
definitive hosts. No animal reservoir. Endemic in central and
west Africa.
Pathogenesis: Hypersensitivity to adult worms causes
“swelling” in skin. Adult worm seen crawling across
conjunctivas
Laboratory Diagnosis:
• Microfilariae visible on blood smear.
Treatment: Diethylcarbamazine.
Prevention: Deer fly control.
58
59
Memory Tool
• Her name was Loa she was an eye worm
…….
60
Onchocerca
Disease: Onchocerciasis (river blindness).
Characteristics: Tissue nematodes.
61
Onchocerca
Life cycle:
• Bite of female black fly deposits infective
larvae, which mature in body cavity.
• Worms enter subcutaneous tissue, where they
mature within skin nodules.
• Females produce microfilariae, which migrate in
interstitial fluids and are ingested by black flies,
in which the infective larvae are formed.
62
RIVER BLINDNESS/SOWDA
trapped microfilaria in the cornea, choroid, iris and anterior
chambers, leading to photophobia, lacrimation and blindness63
64
Onchocerca
Transmission: Transmitted by female black flies. Humans are
the only definitive hosts. No animal reservoir. Endemic along
rivers of tropical Africa and Central America.
Pathogenesis: Microfilariae in eye ultimately can cause
blindness. Adults induce inflammatory nodules in skin.
Laboratory Diagnosis: Microfilariae visible in skin biopsy,
not in blood.
Treatment: Ivermectin affects microfilariae, not adult worms.
Suramin for adult worms.
Prevention: Black fly control and ivermectin
65
Toxocara canis
Disease: Visceral larva migrans.
Characteristics: Nematode larvae cause
disease.
66
Toxocara canis
Life cycle:
•
•
•
•
Toxocara eggs are passed in dog feces
Ingested by humans.
Hatch into larvae in small intestine
Larvae enter the blood and migrate to organs, especially liver,
brain, and eyes, where they are trapped and die.
Transmission:
• ingestion of eggs in food or water contaminated with dog
feces.
• Dogs are definitive hosts. Humans are dead end hosts.
Pathogenesis: Granulomas form around dead larvae.
Granulomas in the retina can cause blindness
67
Toxocara canis
Laboratory Diagnosis: Larvae visible in
tissue. Serologic tests useful.
Treatment: Diethylcarbamazine
Prevention: Dogs should be dewormed
68
Wuchereria
Disease: Filanasis.
Characteristics: Tissue nematodes.
69
Wuchereria
Life cycle:
• Bite of female mosquito
• Deposits infective larvae that penetrate bite
wound, form adults, and produce microfilariae.
• These circulate in the blood, chiefly at night,
and are ingested by mosquitoes, in which the
infective larvae are formed.
Transmission:
• Female mosquitoes of several genera.
• Humans are the only definitive hosts.
70
• Endemic in many tropical areas.
Here are microfilaria. These tiny worms circulate in the bloodstream. There are several
species with slightly different clinical characteristics, but they are spread by mosquitos.
71
These microfilaria happen to be Wuchereria bancrofti.
Wuchereria
Pathogenesis:
• Adult worms cause inflammation that blocks lymphatic vessels
(elephantiasis).
• Chronic, repeated infection required for symptoms to occur.
Laboratory Diagnosis: Microfilariae visible on blood smear.
Treatment: Diethylcarbamazine affects microfllariae. No
treatment for adult worms.
Prevention: Mosquito control
72
73
ELEPHANTIASIS
hydrocele: most common manifestation of
chronic W bancrofti infection
74
75
76
77
78