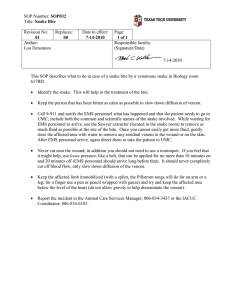
snake bite 1
advertisement
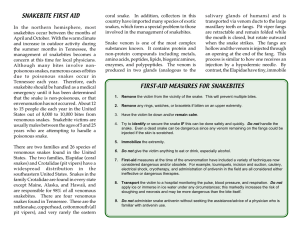
SNAKE BITE BY Dr. Riaz Ahmed OBJECTIVES INTRODUCTION / CLASSIFICATION WHO – STATISTICS. S.B- A- P.H. PROBLEM WHY? EPIDEMIOLOGY ETIOLOGY / CAUSES OF INCIDENCE OF S.B. GRAVITY OF S.B SNAKES VICTIM SOME DANGER SIGNS MANAGEMENT MAJOR VENOMOUS SNAKES OF PAKISTAN PREVENTION IMPORTANCE: SNAKES ARE REPTILES: NO (LEGS, EXT-EARS & EYE – LIDS). NIOCTURNAL IN NATURE / HABIT. AVOID CITIES & HEAVILY POPULATED AREAS. MORE NUMEROUS IN VILLAGES, FIELDS, AGRICULTURE-LANDS, VEGETATION, MARSHES & JUNGLES. CLASSIFICATION: PHYLUM CHORDATA SUB PHYLUM VERTEBRATA CLASS REPTILIA C.R ORDER SQUAMATA (KEY) P S.ORDER OPHIDIA S FAMILIES O C V S MEDICALLY IMPORTANCE FAMILIES & THEIR VENOM CHARACTERISTICS: VIPRIDAE HAEMATO TOXIC ELAPIDAE NEURO –TOXIC HYDRO – PHIDAE (MYO – TOXIC) W.H.O STATISTICS: WORLD WIDE OCCURRENCE: 3L / ANN MORTALITY: 30 – 40,000 / ANN TOTAL SPECLIES: UPTO – (1—2 MIL) WORLD 2500 to 3000 (Species) PAKISTAN 330 LAND SEA 300 29 VENOMOUS DEATH – RATE 30 BURMA – 15.40 L / ANN PAK – 1.90 7TH BRITISH GVIANA TOP 0.80 ( LOWEST ) SNAKE – BITE A PUB. HEALTH PROBLEM WHY? 68 % POP IN RURAL AREAS DUE TO URBANIZATION. MAJORITY FARM WORKERS. WATER LANDS BARE – FOOTED. LACK OF EDUCATION, MEDICAL & MECHANIZED FARMING FACILITIES. EPIDEMIOLOGY WHO (PERSON) / POP. AT RISK: / VICTIM: FARM-WORKERS, VILLAGERS, HARVESTORS, CULTIVATORS, MILITARY-TROOPS, SCOUTS, FISHERMEN, LANDPLOUGHERS, BATHERS, PADDLERS, LAB-WORKERS, ZOOWORKERS & HUNTERS etc. T WHEN (TIME): P P PEAK INCIDENCE BETWEEN JUNE – AUGUST? WHERE: (PLACE) ALREADY DISCUSSED. +. IN FIELDS, JUNGLES, GRASSYLANDS, MARSHES, PERI- URBAN & SLUM AREAS. FIRST DOCUMENTED CASE 1550 B.C. IN PAK: HOSPITAL DATA SHOWS: RISK ADULT MALES CHILDREN B / W 9 ---15 YEAR AT RISK ACTIVITIES ( IN WILD ) : FIRE WORK COLLECTION DISLODGING OF LOGS / STONES. PROBING OF CREVICES / NICHE ‘ S. CLIMBING ROCKS / TREES COVERED WITH VEGETATION. IN SIND (THAR) – 5TH COMMONEST CAUSE OF HOSPITAL ADMISSION. CAUSES OF HIGH INCIDENCE OF S.B IN JUNE TO AUGUST: COLD BLOODED MORE ACTIVE IN HOTTER MONTHS ( POKLIO-THERMIC) VENOM YIELD IS MORE SLEEPING HABITS OF PEOPLE IN RURAL AREAS BARE FOOTED & IN OPEN SITE. RAINS & FLOOD SEASON. COBRA & KRAIT OVIPAROUS IN SUMMER. RUSSEL’S VIPER VIVIPAROUS & SAW SCALED VIPER OVI – LAYING EGGS VIVI – GIVING YOUNG ONES. Gravity of snake-bite FACTORS IN SNAKE FACTORS IN VENOM Age, size, health of snake Also age and general health Agitation Absorption rate Weather Site of distal end / fatty area Hibernation Personality Prior attack Sensitivity of attack to venom Preventive measures Psychological impact, type of 1st aid. CLINICAL-MANIFESTATION: VIPRIDAE: - SEVERE LOCAL PAIN, ECCHYMOSIS, AND PAINFUL-LYMPHADENO PATHY. SYSTEMIC: NAUSEA, VOMITING, SWEATING HYPOTENSION. PASTHOGENESIS OF S.B INOCULATION / INJECTION BY SNAKES ENTERS SURROUNDING TISSUE AUTOPHARMACOLOGICAL MANIFESTATAION CAPILLARY ABSORPTION ACTS ON BLOOD VESSELS& LYMPHATICS,TARGET ORGANS SHOW SYSTEMIC EFFECT Recovery OR Death DIRECT VENOM ACTION DANGER SIGNS: NUMBNESS TINGLING OF FACE HAEMATEMESIS HAEMATO-CHAZIA ELAPIDAE (IIND FAMILY) (MEDICALLY IMPORTANT) VENOM NEURO-TOXIC RELATED S / S APPEAR. HYDRO-PHIDAE:(III ONE). AS VENOM IS MYO-TOXIC SO S / S LIKE TRISMUS, EXT. OPTHALMOPLEGIA, MYOGLOBIN + PROTEIN (URIA), DEATH USUALLY DUE TO EXTREME PAESIS RES. FUNCTION. DIAGNOSIS: HISTORY P BITES N.P VENOM EFFECTS i.e. MIN VS MAXIMUM MANAGEMENT LOCAL MEASURES FIELD & FIRST AID TOURNIQUET LOCALWASHING INCISION & DRAINAGE FASCIOTOMY RUPTURE OF BLEBS & BLISTERS. IMMOBALIZATION OF AFFECTED – EXTREMITY. SYSTEMIC: SPECIFIC SERUM THERAPY. SUPPORTIVE & SYMPTOMATIC. SPECIFIC: POLY - VENIN ANTI-VENIN THERAPY ANTI – VENIN ROUTE OF ADMINISTRATION 1 / V OR 1 / ART. 1/M S/S DOSAGE CHILDREN 1 / α SUPPORTIVE: BED-REST ANALGESICS & SEDATIVES WARMTH VENTILATION – SUPPORT SEQULAE: NO EFFECT PSYCOLOGICAL ACCORDING TO EN-VENOMATION OTHERS: OF TOURNIQUET INCISION WOUND SEPSIS HAZARDS OF ANTI-VEN Major Venomous Snakes of Pakistan Reassure First Aid Treatment : Do it R. I. • 70% of bites are from non-venomous snakes G. H. T • Only 50% of bites from venomous snakes envenomate, the rest are dry bites. Immobilize • As if for a broken limb with a cloth and/or splint • No tight bandages • No washing, cutting or sucking bite site. Get to Hospital • Without delay • No traditional treatments Tell tale signs • Mark rate of swelling • Note onset time of symptoms and tell the doctor. PREVENTIVE-MEASURES: WEARING OF HIGH KNEE BOOTS AS 50 % BITES BELOW KNEE (ESP FOR P.P AT RISK). E.g. SCOUTS, MIL. TROOPS ETC. USE OF TORCH WHILE WATERING THE FIELDS OR OTHERWISE AT NIGHT HEALTH EDUCATION FOR CHILDREN AS WELL AS FOR TROOPS ANTI-VENOM USE 1ST-AID MEASURES / ANTI-S.B-KIT. VACCINATION. Snake bite OSPE: (04) A farmer has been brought in hospital with H/O snake bite showing following Symptoms: i) Bleeding gums ii)Hematuria ii) Hematemesis (a) What is the likely family of snake? (01) (b) Which system of farmer will be affected by the venom of this snake? (01) (c) How will you manage the case? key: (a) Family Viperidae (b) Cardiovacular system (c) i) Application of tourniquet proximal to bleeding area ii) Analgesics iii) Anti-pyretics iv) ATS v) Anti-venin therapy