Welcome to TRICARE - Joint Services Support
advertisement
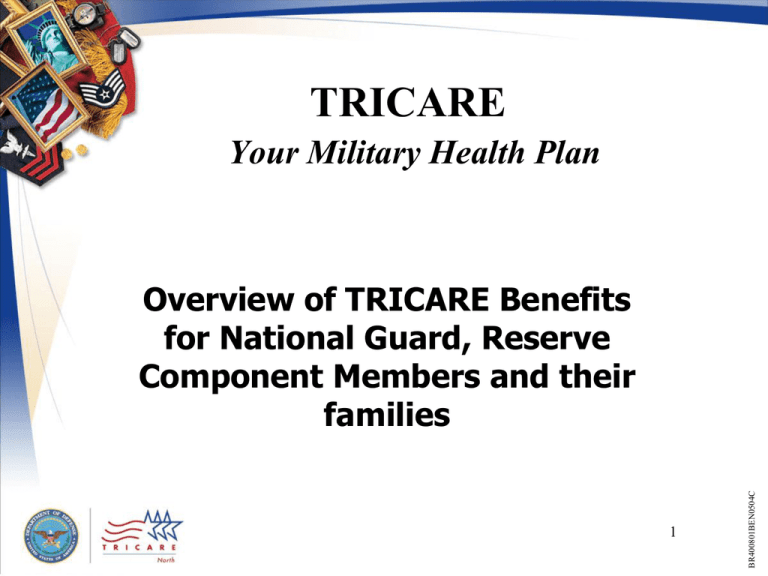
TRICARE Your Military Health Plan 1 BR400801BEN0504C Overview of TRICARE Benefits for National Guard, Reserve Component Members and their families TRICARE Regions West Region TriWest Healthcare Alliance 1-888-TRIWEST www.triwest.com North Region Health Net Federal Services, Inc. 1-877-TRICARE www.healthnetfederalservices.com South Region Humana Military Healthcare Services, Inc. 1-877-249-9179 (TPR/SHCP) 1-800-444-5445 (general) www.humana-military.com 2 Take Action to Ensure Eligibility! DEERS Registration is Required • Visit an ID card-issuing facility – Find one near you at www.dmdc.osd.mil/rsl • Call 1-800-538-9552 • Mail proof of Medicare-eligibility to: Defense Manpower Data Center Support Office Attn: COA 400 Gigling Road Seaside, CA 93955-6771 Registration in DEERS is key to TRICARE eligibility Who is eligible for TRICARE? • Active duty service members (ADSMs) and retirees of any of the seven uniformed services • NG and Reserve Component members on active duty for more than 30 consecutive days (under Federal orders), from any of the seven uniformed services • Spouses of active duty, retired, and eligible NG/ Reserve Component service members • Unmarried children (including stepchildren) up to age 21 (or 23 if full-time student) • Past age 21—Mental/Physical incapacity (Unmarried children remain eligible even if parents divorce or remarry) 4 BR400701BEW0404C • Service Member Coverage Varies… • When on military duty for 30 days or less – Line of duty coverage – TRICARE Dental Program – TRICARE Reserve Select • When called or ordered to active duty for more than 30 consecutive days – Active duty health and dental benefits, including pharmacy – Automatic termination from TRICARE Reserve Select – Transitional health coverage, including pharmacy – TRICARE Dental Program – TRICARE Reserve Select 5 BR413001BET0605W • After leaving active service, or demobilizing Service Member on Military Duty 30 Days or Less • Health: Line of Duty (LOD) Health Care – Any injury, illness, or disease incurred or aggravated in the line of duty • Includes emergency care – Covered portal to portal – Coordinate LOD health care through unit commander or designated medical representative • Dental: TRICARE Dental Program (TDP) Family members are not eligible for health coverage when you are on military duty for 30 days or less Service Member Activated More than 30 Days • Health: TRICARE / Military Treatment Facility – TRICARE Prime/TRICARE Prime Remote – TRICARE Overseas Prime/TRICARE Global Remote Overseas – Pharmacy coverage • Dental: Active Duty Dental Coverage – Military dental treatment facilities – Tri-Service Remote Dental Program If activated in support of a contingency operation, you may also qualify for pre-activation coverage Health Care Options for Family Members when Sponsor is Activated • • • • TRICARE Standard and TRICARE Extra (Automatic) TRICARE pharmacy benefit (Automatic) TRICARE Prime (Requires enrollment) TRICARE Prime Remote for Active Duty Family Members (TPRADFM) (Requires enrollment) Contact your TAO for information about health care options if you accompany your sponsor overseas when they are activated TRICARE Standard • Enrollment not required - Automatic • Care from non-network TRICAREauthorized providers – Provider may charge up to 15% above TRICARE allowable charge – May have to submit your own health care claims • Referrals not required for specialty care – Some services may require prior authorization • MTF care on a space-available basis only TRICARE Extra • Enrollment not required - Automatic • Care from TRICARE network providers – Providers agree to accept negotiated rate as TRICARE allowable charge – Lower cost-shares than TRICARE Standard – No claims to file (in most cases) • Referrals not required for specialty care – Some services may require prior authorization • MTF care on a space-available basis only TRICARE Standard and Extra Costs TRICARE Option TRICARE Standard Deductible Sponsor rank E1-E4: (Using non-network/Standard providers) Amount due each fiscal year before cost-sharing begins. $50/single or $100/family TRICARE Extra (Using Network/Prime providers) Same Sponsor rank E5 & above: $150/single or $300/family Outpatient Cost-share Inpatient Costs Inpatient Behavioral Health Care Catastrophic Cap 20%* $15.15/day ($25 minimum) $20/day ($25 minimum) 15% Same Same $1,000 per family per fiscal year The federal fiscal year is Oct. 1- Sept. 30. * Non-network providers may charge up to 15% above the TRICARE allowable charge. Get extra cost-savings with TRICARE Extra! TRICARE Prime Service Area (PSA) • Area defined as an approximate 40-mile radius around an MTF (actual radius can vary by military installation) • TRICARE-eligible beneficiaries living within the Prime service area are eligible for Prime • Beneficiaries living outside the Prime service area may be eligible for TRICARE Prime Remote for Active Duty Family Members (TPRADFM) 12 Enrolling in TRICARE Prime • Prime must be available in your area • Active duty and family members—no enrollment fee • Enroll by 20th of month—effective 1st of the next month • If you enroll after the 20th of the month, your enrollment will begin on the 1st day of the 2nd month after that 13 Eligibility for TRICARE Prime Remote / TPRADFM • National Guard or Reserve sponsor – Activated more than 30 consecutive days – Live and work more than 50 miles (or an hour’s drive time) from an MTF – Sponsor’s residence address must be in DEERS – Family must reside with sponsor in a designated TPR ZIP code at time of activation To see if you qualify, check your ZIP code at www.tricare.mil/tpr. 14 TPR/TPRADFM • TRICARE Prime option for active duty families in remote locations – Available in designated TPR ZIP code areas • Enrollment required • TRICARE-authorized providers – Network providers when available – Same rules as TRICARE Prime for getting care • No claims to file (in most cases) 15 Enrolling in TRICARE Prime/TPRADFM • Submit completed enrollment application to your regional contractor – If received by 20th of month, coverage begins 1st of next month – If received after 20th of month, coverage begins 1st of following month • Select a PCM – From military treatment facility (MTF) or TRICARE network – For TPRADFM, select any TRICARE-authorized provider if a network PCM is not available Primary Care Manager • Any TRICARE-authorized provider – Network provider, if available – Non-network, if network provider not available • Provides most care—routine, urgent, and some clinical preventive services • Provides referrals for necessary specialty care – Coordinates referral request – Obtains necessary prior authorization Contact your regional contractor for assistance finding a PCM. 17 TRICARE Prime/TPRADFM Costs (TRICARE Prime Remote Active Duty Family Member) Enrollment Fees $0 Deductible* $0 Outpatient Costs* $0 Inpatient Costs* $0 Emergency Care $0 Catastrophic Cap $1,000 per family per fiscal year The federal fiscal year is Oct. 1- Sept. 30. *You’ll pay higher out-of-pocket costs if you use the point of service option (POS). Emergency Care 19 BR400701BEW0404C • Call 911 • Visit nearest emergency room • Notify your PCM or Regional Contractor within 24 hours of any emergency admission so that your follow-up care can be coordinated (if enrolled in TRICARE Prime) • A family member can call on your behalf Urgent Care 20 BR400701BEW0404C • Medically necessary treatment that is required for illness or injury • TRICARE Prime beneficiary must coordinate urgent care with PCM or Regional Contractor before receiving care • A TRICARE Prime beneficiary who seeks urgent care services without coordinating with his or her PCM will be utilizing the TRICARE Point-of-Service (POS) option Nonemergency Health Care While Traveling 21 BR400701BEW0404C • All routine medical care should be taken care of before you depart or delayed until you return and can see your PCM • For out-of-area urgent/acute care, you must coordinate with your PCM or Regional Contractor for an authorization before seeking care if enrolled in TRICARE Prime • For out-of-area emergency care, call 911 or go to the nearest emergency room (civilian or military) Point of Service Option • Seek nonemergency/specialty care without a referral or prior authorization • Higher out-of-pocket costs – Annual Deductible: $300/individual or $600/family – Cost-Shares: 50% after POS deductible is met • POS fees not reimbursed by TRICARE • POS fees do not apply to the annual catastrophic cap Avoid POS fees! Follow TRICARE Prime/ TPRADFM referral and authorization guidelines TRICARE and Other Health Insurance • TRICARE pays after all other health insurance plans except for: – – – – Medicaid TRICARE supplements The Indian Health Service Other programs/plans as identified by TMA • Not required to obtain TRICARE referrals or prior authorization for covered services, except for adjunctive dental care and behavioral health care services • However, you must follow the OHI referral and authorization requirements if applicable • TRICARE is NOT a supplement to other insurance. 23 TRICARE Pharmacy Coverage Generic Brand Name Non-Formulary MTF $0 $0 TMOP $3 $9 $22 Network Retail $3 $9 $22 (up to a 90-day supply) (up to a 90-day supply) (up to a 30-day supply) Non-network Retail Pharmacy (up to a 30-day supply) $0* †Non-TRICARE †Non-TRICARE †Non-TRICARE †TRICARE †TRICARE †TRICARE Prime: $9 or 20% Prime: 50% cost-share Prime: $9 or 20% Prime: 50% cost-share Prime: $22 or 20% Prime: 50% cost-share *Not available in the MTF unless medical necessity is established. †Deductibles apply. 24 BR413201BET0605W Type of Pharmacy TRICARE Dental Options Military dental treatment facilities Contact your local military dental treatment facility. Tri-Service Remote Dental Program Military Medical Support Office http://mmso.med.navy.mil TRICARE Dental Program • Active duty family members • National Guard and Reserve members (not activated) and family members United Concordia Companies, Inc. 1-800-866-8499 www.TRICAREdentalprogram.co m TRICARE Retiree Dental Program • Retired service members and family members • Medal of Honor recipients and family members Delta Dental Plan of California 1-888-838-8737 www.trdp.org Active Duty Dental Options 25 Questions? 26