Holman-AnUpdateOnBabesiosis - Texas Department of State Health
advertisement
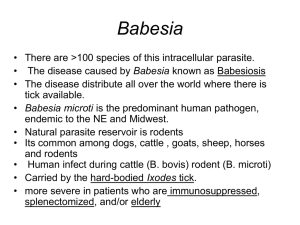
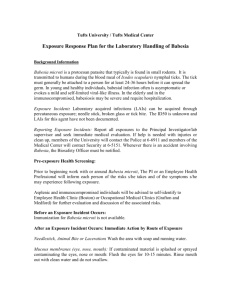
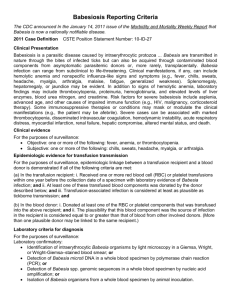
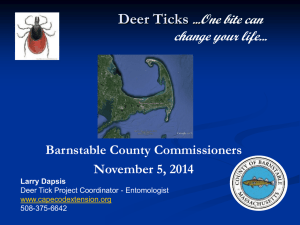
Human Babesiosis – An Update Patricia J. Holman Department of Veterinary Pathobiology College of Veterinary Medicine and Biomedical Sciences Texas A&M University College Station, TX Babesiosis • Emerging tick-borne disease • Zoonosis caused by intraerythrocytic protozoan parasites • Infections may range from asymptomatic to severe, or even fatal • Most cases occur in the U.S.; worldwide where ticks occur • Phylum – Apicomplexa – Babesia, Plasmodium, Toxoplasma, Cryptosporidium – Unique organelles comprise apical complex Electron micrograph courtesy of Dr. R.E. Droleskey USDA College Station, TX Babesia - Two-host life cycle Sexual reproduction in the vector tick Asexual reproduction in mammalian red blood cells Vertebrate Tick Salivary glands Kinete Ovaries, Eggs Gut Zygote Gamont Babesia microti Tick transstadial transmission 2. Tick picks up infection from parasitemic host 3. Tick molts to nymph - now infective 1. Larval ticks hatch 4. Tick feeds on mice or other hosts; transmits 6. Adult tick feeds on host, then females drop to lay eggs 5. Tick loses ability to transmit infection during molt from nymph to adult unless it feeds on an infected host as a nymph Babesia divergens Tick transovarial transmission 1. Adult tick picks up infection from parasitemic host 2. Infected larval ticks hatch 3. Tick feeds on cattle or other hosts; transmits Babesia Babesiosis • Symptoms 1-6 wks after tick feeds • Variable – Asymptomatic infection – Mild to moderate illness – Severe disease – usually immunosuppressed • • • • Medication Splenectomy HIV co-infection Malignancy Babesiosis • Symptoms – Fatigue – Intermittent fever • Chills, sweats, headache, arthralgia, anorexia, cough, nausea Asymptomatic infection • Clinical Presentation – Fever, pallor – Splenomegaly – Hepatomegaly • May last a week or months • Prolonged recovery; persistent parasitemia Babesiosis – Severe form • Most common complications – Respiratory failure – Congestive heart failure – DIC – Liver and kidney failure – Splenic rupture – Immunocompromised – 21% mortality Diagnosis • CBC – Hemolytic anemia with elevated reticulocytes – Thrombocytopenia – Normal to slightly decreased leukocyte count • Blood chemistry – Elevated serum liver enzymes (~ ½ of patients) – Proteinuria, elevated blood urea nitrogen and serum creatinine Diagnosis • Microscopic identification – Giemsa stained thick or thin blood films – Babesia ring forms can be mistaken for malaria • Serology - IFA – B. microti • B. duncani does not cross-react – B. divergens • Sera from B. divergens or B. ventorum patients cross react Diagnosis • Polymerase chain reaction – Highly sensitive and specific – Useful for extremely low parasitemias • Confirm infection • Determine species • FISH – Detects Babesia DNA in patient blood film – Specific probe binds to DNA – Highly specific; not as sensitive as PCR IGeneX Diagnosis • Subinoculation into laboratory animals – 2-4 weeks for parasites to appear in circulation – Hamster – Babesia microti – No known laboratory host for all of the human Babesia spp. Treatment • Atovoquone/azithromycin 7-10 days – B. microti infections – 15% adverse reactions – Diarrhea and rash • Clindamycin/quinine 7-10 days – Recommended for severe babesiosis – 72% adverse reactions – Diarrhea; tinnitus and hearing loss • Exchange transfusion - severe illness Prevention • Avoid areas with ticks, mice and deer – Especially May-October – Especially immune compromised people • Anti-tick strategies – – – – Long sleeves, long pants tuck cuffs into socks Pyrethrins on clothing DEET on exposed skin Check for and remove ticks promptly after possible exposure Prevention II • Property – Keep grass short – Remove leaf litter – Discourage mice • Seal potential den holes • Pyrethrin treated cotton – Discourage deer • “Deer proof” plants • Fencing Prevention III • Transfusion risk – No FDA approved test for donated blood – Agencies prohibit donations by people who live in or visit endemic areas – Research ongoing for ways to inactivate organisms in blood Zoonotic Babesia spp. • Europe – Babesia divergens - France, Ireland, Great Britain (cattle production) – Babesia venatorum – Austria, Italy, Germany – Babesia microti • Asia, Africa, and South America – Babesia microti-like – B. divergens-like – Ovine Babesia-like Babesia divergens • Most cases occur in France & British Isles – – – – 30 reported human cases Associated with cattle 84% asplenic patients; 42% fatality rate Infection is considered a medical emergency • Hosts – Cattle, small mammals – Ixodes ricinus Babesia venatorum • Three documented cases – All asplenic and > 50 years – Mild to severe, but not fatal • Parasites – typical paired pyriform • Hosts – Roe deer – Ixodes ricinus Zoonotic Babesia spp. • United States – Babesia microti - Northeast and upper midwest – Babesia duncani – Washington state (WA1-3) – California CA1-6 (similar to B. duncani ?) – Babesia divergens-like – MO-1 and KY (Nantucket Island) – Babesia divergens-like – Washington state Babesia microti • Most cases occur in the U.S. – > 300 known cases – not a reportable disease – Variable severity of disease • Most symptomatic cases mild and self-limiting • Immune suppressed or >50 yrs at higher risk of severe disease • 5% mortality rate – Tick transmission May-October – Transfusion or blood product associated cases – Neonatal cases Babesia microti • U.S. endemic regions – – – – Ixodes scapularis White footed mouse White-tailed deer maintain the vector tick B. microti cannot infect deer • Parasites in tetrads in “paired” form Babesia microti • Not considered a major human pathogen in Europe – High prevalence in rodents – Ixodes trianguliceps vector tick – nest dwelling – Ixodes ricinus Babesia duncani • Washington and California • Five cases – Spleen intact individuals – Subclinical to severe illness – 2 were acquired via transfusion • Seroprevalence 4 to 17% • Tick vector and reservoir host unknown • Parasites in tetrads in “paired” form Babesia divergens-like • One case in Washington state – Asplenic, > 50 years – Similar molecularly to Babesia divergens – Tick and reservoir host not known Babesia divergens-like • Two cases - MO-1 and KY – Both asplenic, > 50 years – Both severe disease, 1 death – Parasite endemic on Nantucket Island • Eastern cottontail rabbits • Ixodes dentatus • Not infective to cattle • No human cases on Nantucket Island Babesia divergens-like cases of Human Babesiosis • KY isolate – Critically ill man admitted to emergency room in Kentucky • Fever • Chills • Bloody urine • Immediately started on doxycycline – Ehrlichiosis? Babesia divergens-like KY • Blood smear - Numerous babesia organisms • History – Splenectomy 9 years previously – Tick exposure • Recreational hunter • WTD and cottontail rabbits Diagnosis and Treatment • Negative for Ehrlichia and Babesia microti • *** Babesia divergens *** (Beattie et al. 2002) • Pathology - Asplenic • Morphology • 18S rRNA gene sequence • Hospitalized for 12 days • TX: Clindamycin, quinine, and doxycycline B. divergens-like MO-1 • MO-1 – – – – Fever, chills, headache, sore throat, and joint pain No improvement with erythromycin Fatal infection (Herwaldt et al, 1996) MO-1 18S rRNA gene identical to KY B. divergens-like NR • Nantucket (rabbit isolate) – KY/MO-1 18S rRNA gene identical to NR (Goethert & Telford 2003) – 16% of rabbits positive by PCR – Ixodes dentatus ticks, larval to nymphal stage 4% + Babesia divergens Discrepancies • Tick vector ? • Neither patient had traveled outside of the US • No known infection in U.S. cattle despite high cattle population in Kentucky and dairies on Nantucket Island SSUrRNA ITS1 5.8S ITS2 LSUrRNA rRNA ITS1 & ITS2 Percent Identities KY NR Bdiv KY 100 100 94 NR 100 100 94 Bdiv 90 90 100 Infection Studies • Source of parasites needed – No blood from the case • Rabbits – Limited by extremely low circulating parasitemias • In vitro culture – Produce quantities for additional characterization – Collaboration with Goethert and Telford, Tufts University Host erythrocyte specificity in vitro Parasite Host RBC Serum supplement Growth Nantucket Rabbit (NR774) Human Bovine Cottontail rabbit Human Bovine Human Yes No Yes Human Bovine Cottontail rabbit Human Bovine Human Yes Yes No B. divergens Results - Morphometric Parasite NR Bdiv KY Host RBC Size Human Cottontail rabbit Bovine 4.3 µm Human Bovine Cottontail rabbit 3.1 µm* Human (blood) 4.1 µm 4.2 µm N/A 2.2 µm N/A Stddev ± 0.48 ± 0.56 ± 0.53 ± 0.36 ± 0.58 Cattle Infection Study PCR Day -17 4 5 6 7 9 10 11 Controls Principals Aspl Spleen Aspl Spleen + Day - -17 4 + 5 6 + 7 + 109 + 11 + Culture Controls Principals Aspl Spleen Aspl Spleen - - - - PCR Culture Controls - Principals Controls Principals + + (4) Aspl Spleen Aspl Spleen Aspl Spleen Aspl Spleen +- - - - -- -- - - -+ (2)- + -(4)- - - + + - - - - + (4) - - +- + - - -- -- - - + (2) + (2) + (4) + -(2)- - - + + - - - - + (2) + (2) - - ++ + - - -- -- - - + (1) + (1) + (2) + -(2)- - - ND - - +++ ++ - -- --- --- -- - ND ND ND ND ND - - - - -++ + - - -- -- - - NDNDND ND + - - - - ND ND - - - - Conclusions • KY and NR are conspecific – – – – Identical 18S rRNA gene sequence Identical ITS1 / ITS2 sequences Size - large babesia Morphology • B. divergens distinct – – – – – ITS1 and ITS2 sequences vary from KY/NR Size - small babesia in natural host Morphology Infective for cattle Culture – Bovine RBC, not cottontail rabbit Babesia divergens is not endemic in the U.S. Acknowledgements Dr. Andy Allen, Washington State University, Pullman, WA Dr. Jim Beattie, Bowling Green Associated Pathologists, KY Dr. Bob Droleskey, USDA, College Station, TX Dr. Heidi Goethert, Tufts University, MA Dr. Sam Telford, Tufts University, MA Dr. Will Goff, USDA, Pullman, WA Dr. Don Knowles, USDA, Pullman, WA Angela Spencer & Lorien Schoelkopf Funding: NIH RO3, USDA/ARS, Texas Agricultural Experiment Station